Case Report, J Nephrol Ren Dis Vol: 7 Issue: 1
Lobar Pneumonia, Pulmonary Edema and Acute Post Streptococcal Glomerulonephritis: An Unusual Association
Ditya Devale Rinengo*, Intan Fatah Kumara, Budyarini Prima Sari
Department of Child Health, Gadjah Mada University, Yogyakarta, Indonesia
- *Corresponding Author:
- Ditya Devale Rinengo
Department of Child Health,
Gadjah Mada University,
Yogyakarta,
Indonesia;
E-mail: dityadevale@gmail.com
Received date: 23 September, 2022, Manuscript No. JNRD-22-75758; Editor assigned date: 26 September, 2022, PreQC No. JNRD-22-75758 (PQ); Reviewed date: 10 October, 2022, QC No. JNRD-22-75758; Revised date: 03 January, 2023, Manuscript No. JNRD-22-75758 (R); Published date: 30 January, 2023, DOI: 10.4172/2576-3962.1000019.
Citation:Rinengo DD, Kumara IF, Sari BP (2023) Lobar Pneumonia, Pulmonary Edema and Acute Post Streptococcal Glomerulonephritis: An Unusual Association. J Nephrol Ren Dis 7:1
Abstract
Acute Post Streptococcal Glomerulonephritis (APSGN) is characterized by an abrupt onset of edema, hypertension and hematuria. Although the association of lobar pneumonia and pulmonary edema with acute glomerulonephritis has been established, it is uncommon for children with APSGN to present with respiratory distress due to both lobar pneumonia and pulmonary edema. Here we report a 13 years old boy presented with pneumonia, pulmonary edema and glomerulonephritis simultaneously. Antistreptolysin-O titer was positive and he responded well to appropriate antibiotics and diuretics. We aimed to remind the simultaneous and rare presentation of pneumonia, pulmonary edema and glomerulonephritis.
Keywords: Lobar pneumonia; Pulmonary edema; APSGN; Glomerulonephritis
Introduction
Acute Post Streptococcal Glomerulonephritis (APSGN) is characterized by acute nephritic syndrome (hematuria, edema and hypertension) in the context of low serum C3 levels and elevated Antistreptolysin O Titer (ASOT) [1]. APSGN causes up to 21% of acute renal failure among children in developing countries. APSGN most commonly occurs in children two to 12 years of age with the clinical onset one to three weeks following group A Streptococcal (GAS)-positive pharyngitis or three to six weeks after gas impetigo [2]. Because post infectious nephritic syndrome is indistinguishable from different antecedent infectious etiologies, diagnosis of APSGN relies on documentation of preceding gas infection. Association of APSGN with lobar pneumonia and pulmonary edema are rarely reported. Here we report a thirteen years old boy with lobar pneumonia and pulmonary edema who presented simultaneously with APSGN.
Case Presentation
A 13-year-old boy presented with cough, fever, shortness of breaths and abdominal pain lasting for over four days. Past medical history was unremarkable. On physical examination his temperature was 38.7℃, pulse rate 129 beats/minute, respiratory rate 70 breaths/minute and blood pressure was 140/100 mmhg (>95th percentile for age, height and gender). Oxygen saturation was maintained above 95% by non-rebreathing mask 6 liter per minute [3].
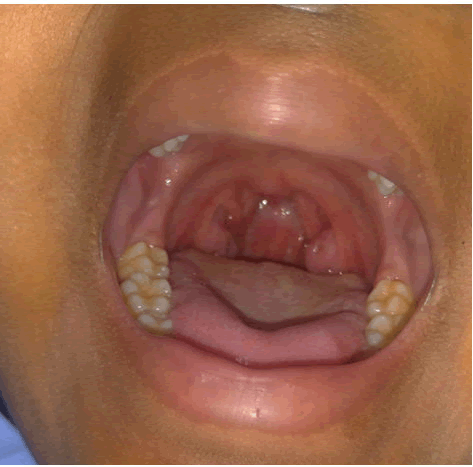
He had no erythematous posterior pharynx, but the tonsil size was 2+. On auscultation, respiratory voices were decreased on both basal regions and crackles especially on both upper lungs. Abdomen was diffusely tender. There were some brownish crusts with peripheral erythema on both legs. Other system examinations were normal.
Laboratory examinations revealed elevated white blood cells of 40.670/mm3 (89.9% neutrophils, 6.2% lymphocytes, 3.9% band forms) with hemoglobin 11.7 g/dl and platelets 715.000/mm3. Blood urea nitrogen and serum creatinine levels were within normal limit at 13.7 mg/dl (5.0 mg/dl-18 mg/dl) and 0.65 mg/dl (0.8 mg/dl-1.3 mg/dl) respectively. Estimated glomerular filtration rate was found to be 97.21 ml/min/1.73 m2 by modified schwartz formula.
On microscopic analysis of the urine there were 200 erythrocytes and 18 leukocytes per high power field. Urine dipstick test revealed no proteinuria. The spot urine protein/creatinine ratio was 0.113 (mg/ mmol) [4]. Qualitative antistreptolysin O serology was positive. C3 and C4 complement were within normal range.
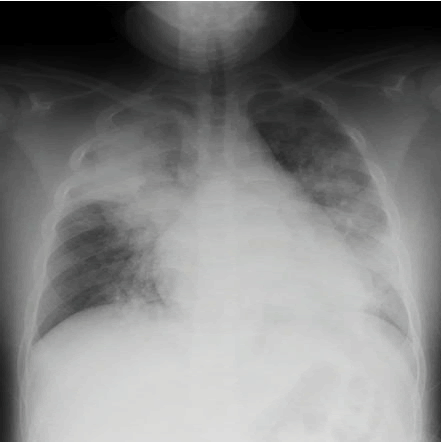
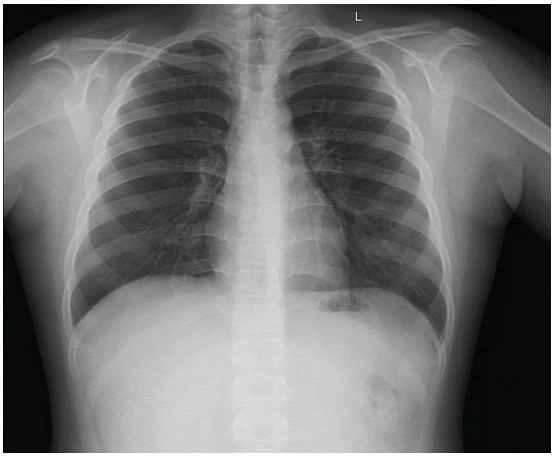
Tracheal aspirate cultures were obtained before antibiotic and the result was gram positive chains of crocus and gram negative solitary rod. On chest radiograph, there were consolidation on right upper lobe and cephalization of pulmonary vessels with hilar haze indicating lobar pneumonia and pulmonary edema [5].
The patient was diagnosed as lobar pneumonia, pulmonary edema and post streptococcal glomerulonephritis. Treatment of ampicillingentamycin and furosemide were started. Successful diuresis begun on the second day of his admission and blood pressure was in normal limits for his age [6]. He was discharged from the hospital on the seventh day and diuretic medications were discontinued (Figures 1-4).
Discussion
Pneumonia associated glomerulonephritis is a rare condition that occurs more commonly in adults than in children. In some reports glomerulonephritis developed soon after pneumonia; macroscopic hematuria developed after 24-72 hours of hospital admission, but in a study, glomerulonephritis developed within six weeks after the infection. In our patient microscopic hematuria was observed simultaneously with respiratory symptoms. However the GFR was still within normal limit. As in other forms of post infectious glomerulonephritis in pneumonia-associated glomerulonephritis, the inflammatory process that takes place in the glomeruli is triggered by antigen antibody reactivity that results in local activity of complement system and of the coagulation cascade.
Antistreptolysin O (ASO) titers were positive in our patient as reported in other series in the literature. Srivastava reported elevated ASO titers in 10 of 11 patients in his study. All of the 3 patients and 5 of the 6 patients in the studies of lechon and vila cots had also elevated ASO titers respectively. But none of these authors attributed glomerulonephritis to Streptococcus pyogenes infection because ASO titers may be affected from many other factors and no universally normal value was applicable. In our patient; tracheal aspirate culture was negative, there was typical clinical, laboratory and radiological findings of pneumonia; impetigo crusts was in both legs which could be risk factor of streptococcus infection.
In our case, the presentation of pulmonary edema complicating an underlying glomerular disease of APSGN is consistent with the well described term pulmonary renal syndrome, which indicates the coexistence of pulmonary and glomerular renal disease. Urinalysis and blood pressure recording should be an essential part of the work up in any severely ill patient who presents with pulmonary edema to investigate the possible coexistence of a glomerular renal disease. Similarly, in children with a glomerular renal disease such as APSGN, who have sudden onset of dyspneic respirations, a chest radiograph should be performed to make an early diagnosis of the potentially life threatening complication of pulmonary edema.
Conclusion
Treatment is usually supportive and directed towards potential complications such as sepsis, hypertension and severe electrolyte disturbances. Dialysis is rarely required in children for treatment of uremia, hyperkalemia or severe circulatory congestion. The respiratory and renal prognosis is favorable in patient with lobar pneumonia and pulmonary edema who presented simultaneously with APSGN. However, clinicians must be aware of the course to make prompt diagnosis and appropriate management and to avoid unnecessary medical intervention.
References
- Lechon FC, de la Torre Espi M, Abal RP, Peiro JEP (2010) Acute glomerulonephritis associated with pneumonia: A review of three cases. Pediatr Nephrol 25:161-164.
[Crossref] [Google Scholar] [PubMed]
- Srivastava T, Warady, Alon US (2002) Pneumonia associated acute glomerulonephritis. Clin Nephrol 57:175-182.
[Crossref] [Google Scholar] [PubMed]
- Vila Cots J, Piqueras Marimbaldo I, Arias Constanti V, Camacho Díaz JA, Gimenez Llort A, et al. (2011) Pneumonia associated acute glomerulonephritis: A review of 6 cases. An Pediatr (Barc) 74:332-335.
- Chiu CH, Huang YC, Wong KS, Hasia SH, Lin CJ, et al. (2004) Poststreptococcal glomerulonephritis with pulmonary edema presenting as respiratory distress. Pediatr Nephrol 19:1237-1244.
[Crossref] [Google Scholar] [PubMed]
- Ozlu SG, Yilmaz AC, Bulbul M, Aydog O, Senel S (2016) Lobar pneumonia and glomerulonephritis: An unusual association. J Nephrol Renal Ther 2:009.
- Coggon D, Inskip H, Winter P, Pannett B (1994) Lobar pneumonia: An occupational disease in welders. Lancet 344:41-43.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi