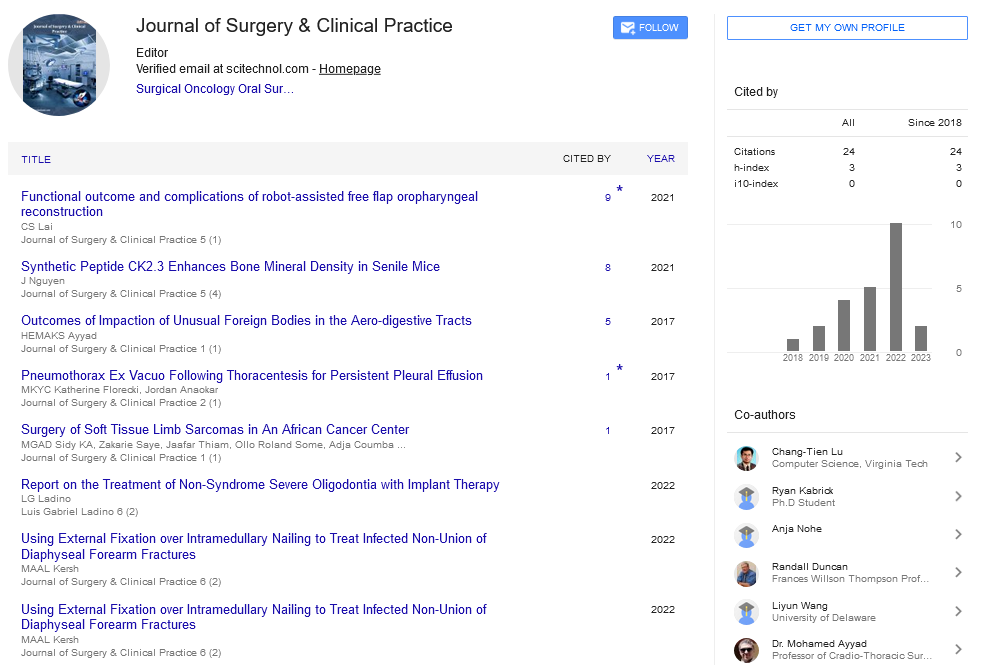
Opinion Article, J Surg Clin Prac Vol: 6 Issue: 3
Next Generation Sequencing in Pediatric Neurosurgery
Renan Chapon*
Department of Neurosurgery, Dijon University Hospital, Hopital Prive Dijon Bourgogne, Bouvet Island
*Corresponding Author: Renan Chapon
Department of Neurosurgery, Dijon University Hospital, Hopital Prive Dijon Bourgogne, Bouvet Island
Email: chaponr28@gmail.com
Received date: 13 April, 2022; Manuscript No. JSCP-22-42525;
Editor assigned date: 15 April, 2022; PreQC No. JSCP-22-42525 (PQ);
Reviewed date: 26 April, 2022; QC No. JSCP-22-42525;
Revised date: 06 May, 2022; Manuscript No. JSCP-22-42525 (R);
Published date: 16 May, 2022; DOI: 10.4172/Jscp.1000365
Citation: Chapon R (2022) Next Generation Sequencing in Pediatric Neurosurgery. J Surg Clin Prac 6:3.
Keywords: Neurosurgery
Description
Anterior lumbar inter-body fusion is now a well-established procedure to treat degenerative lumbar complaint. This approach has its own pitfalls and each chine surgeon must understand the risks that can be encountered when dealing with an deconstruction variation of the vessels in order to be suitable to perform the safest possible procedure. We report the case of a 48 times old man with a rare vascular deconstruction variation witnessing two-situations L4-L5 and L5-S1 ALIF procedure through a right sided retroperitoneal approach. The preoperative imaging planning revealed a duplication of the Inferior Vena Cava (IVC) located on each side of the aorta. Preoperative Imaging evaluation and a detailed knowledge of the deconstruction is the key of a safe and successful procedure as any variation can complicate the anterior approach. We believe that teaming up with a vascular surgeon for inferior surgeons during the first anterior procedures and especially in the environment of anatomical variation is recommended.
Perioperative X-ray control verified the good position of the interbody bias. Except the vascular injury we did not have any other perioperative or postoperative complications. The case was discharged at Day 3 after surgery and noticed enhancement in low reverse pain and leg pain. A post-operative X-ray imaging demonstrated acceptable position of coops at L4-L5 and L5-S1 situations. At 6-week postoperative follow-up, the case presented no rush of symptoms. Anatomical anomalies affecting the Inferior Vena Cava (IVC) have been known since 1793 when Abernathy presented to the Royal Society the case of a 10 months old child. The embryogenesis origin of the duplication of the IVC results from continuity of both supra cardinal modes. Morita described the different vascular position of the IVC using a bracket. We linked in our case a type 2a situation. The careful pre-operative planning allowed us to punctuate this vascular contortion and to acclimatize our surgical approach consequently. The vascular window was, in our opinion, large enough to allow us to perform this procedure safely. We also preferred to continue with our original suggestion because of the history of posterior surgery and performing postoperative fibrosis, but a TLIF could have been a possible result for the case. We believe that it's important that each chine surgeon masters all surgical ways in order to acclimatize to each case and not to totally propose the same fashion. In our knowledge no case report has yet described an anterior approach with that anatomical variation. We do recommend for every chine surgeon to pay particular attention to the vascular deconstruction on the coronal and axial imaging when deciding to perform an Anterior or Oblique approach of the lumbar chine. Access to 3-dimensional imaging examinations is getting easier these days. This allows surgeons to have a veritably precise vision of the operating strategy in order to acclimatize to each situation, particularly in the event of anatomical variation. We do also recommend for the youngish surgeons to work in platoon with a vascular surgeon or an access surgeon in order to get a precious help when planning and performing the spinal emulsion procedure by anterior way. In the world of surgery, spinal surgery is one of the motifs that their surgical suggestions largely depend on the case's clinical symptoms and physical examination, while the para-clinics have only supplementary or conformational places. For case, lumbosacral glamorous resonance imaging in asymptomatic population has a 30-35 incidental finding that hasn't inescapably associated with clinical complaints. These incidental findings include vertebral hemangioma, degenerative slice, transitional backbone, thickened filum terminale, synovial tubercle of the hand joint, or indeed spondylolysis or spondylolisthesis. None of these findings bear treatment when they aren't accompanied by clinical symptoms, but only the croaker knows this principle, not the case.
Perioperative X-ray Control
On the other hand, contriving new seductive and minimally invasive ways in the field of chine surgery, has led to the overpopularity of these surgeries. Because the lesser the number and complexity of surgeries, the lesser the surgeon's benefit, these factors have cumulatively led to the over-prevalence of spinal surgeries, especially in the lumbar region. And in this fermentation and mess bazar, real surgical suggestions which is the most important and vital corridor of drug, has faded or may have been designedly forgotten.
It seems that it's time to go back to the morning and remember the holy pledge at the medical scale form. And at least as altruism, we should always put the case's benefit ahead of our own and come to believe that I may be the case of a croaker in a veritably soon unborn, and in this script, what do we anticipate from our trusted croaker? Let us not allow the fiscal gain to be a hedge for the sense of humanity. Anterior Lumbar Antibody Emulsion (ALIF) was first described in 1906 and is now well established as a safe and effective emulsion procedure. This procedure allows access to a large face of the slice, helping the surgeon to perform an effective and complete discectomy with a high emulsion rate. Each surgeon must be completely apprehensive of the anatomical connections and its possible variations in the retroperitoneal region in order to minimize vascular pitfalls, certain intraoperative complications can snappily lead to life-changing situations. To our knowledge many studies published in literature describe ALIF cases performed in cases with natural vascular. Anomalies we believe that teaming up with a vascular surgeon for inferior surgeons during the first anterior procedures and especially in the environment of anatomical variation are recommended.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi