Research Article, Arch Transplant Vol: 1 Issue: 1
Parathyroidectomy Outcomes in Renal Transplant Recipients: Subtotal vs. Total
Rathore R1,3*, Tomlinson K1, Sharma A2,3 and Halawa A3,4
1University Hospital of North Midlands, Stoke-on Trent, UK
2Royal Liverpool Hospital, Liverpool, UK
3Faculty of Health and Science, Institute of Learning and Teaching, University of Liverpool, Liverpool, UK
4Sheffield Teaching Hospitals, Sheffield, UK
*Corresponding Author : Dr Roshni Rathore
Department of Renal Medicine, University Hospitals of Coventry and Warwickshire Clifford Bridge Road, Coventry CV2 2DX, UK
Tel: 00447894910481
E-mail: roshni.rathore@nhs.net
Received: November 29, 2017 Accepted: December 18, 2017 Published: December 22, 2017
Citation: Rathore R, Tomlinson K, Sharma A, Halawa A (2017) Parathyroidectomy Outcomes in Renal Transplant Recipients: Subtotal vs. Total. Arch Transplant 1:1.
Abstract
Persistent hyperparathyroidism in renal transplant recipients has been associated with increased mortality and decreased allograft survival in up to 50% of patients. Management involves Cinacalcet and/or Parathyroidectomy and practices vary. Merits of subtotal vs. total parathyroidectomy have been debated and currently there is no consensus on best practice. In this single centre retrospective study, we identified patients that had a parathyroidectomy post transplantation between 1/01/2007 and 1/01/2017 (n=22) and graft survival and bone biochemistry were evaluated over a 12 month period. Patients with failed transplants and multiple transplants were excluded. Remaining 11 patients were divided into 2 groups –those that had subtotal parathyroidectomy (SP) vs. those that had total parathyroidectomy (TP) without auto transplantation.
Keywords: Hyperparathyroidism post-transplant; Parathyroidectomy; Total parathyroidectomy; Subtotal parathyroidectomy
Introduction
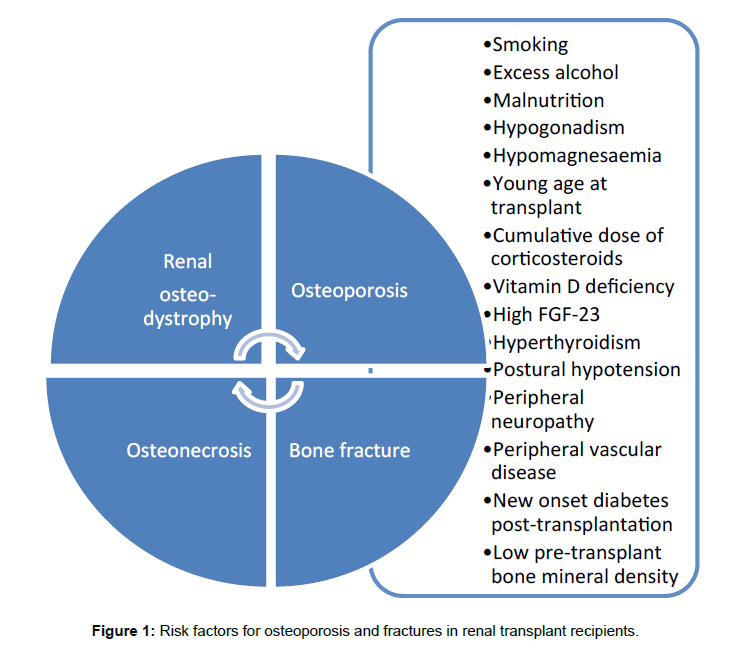
Persistent hyperparathyroidism post renal transplantation is a significant cause of morbidity and mortality with increased risk of osteoporosis and fractures. Once graft function stabilises after transplantation, mild hyperparathyroidism resolves and bone biochemistry normalises [1-3]. However, it has been reported that between 15-50% patients have persistent hyperparathyroidism due to residual structural changes of hyperplasia or adenoma in parathyroid gland and complex interactions of immunosuppressive medication and bone minerals in the new milieu [4-8] (Figure 1).
Whereas in chronic kidney disease, secondary and later tertiary hyperparathyroidism are responsible for changes in bone parameters and bone mineral density, after renal transplantation, changes in bone parameters (hypophosphatemia and hypocalcaemia) mimic primary hyperparathyroidism. Hypercalciuria that could lead to renal tubular injury and increase risk of stone formation, soft tissue calcification, myopathy and hypertension have also been reported with persistent hyperparathyroidism.
Management of persistent hyperparathyroidism is either medical or surgical or both and practices vary across different centres. Use of cinacalcet has increased in recent years both as bridging therapy prior to parathyroidectomy or instead of parathyroidectomy. Although it reduces the burden of hypercalcaemia related morbidity, no benefit on bone mineral density has been reported in the literature. Rebound hyperparathyroidism on discontinuation, significant gastro-intestinal side-effects, cost of the drug and lack of availability limit its use.
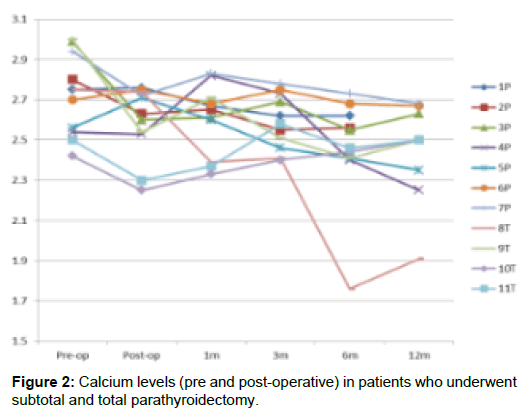
In terms of surgical treatment, the merits of subtotal vs. total parathyroidectomy have been debated and currently there is no consensus on best practice [4-6]. Some centres report underutilisation of surgical treatment [7]. Total parathyroidectomy has been known to cause hypocalcaemic events that require IV calcium replacements and parathyroid auto-transplantation in some instances [9]. Subtotal parathyroidectomy on the other hand may not be sufficient to keep calcium levels in the normal range in the longer term therefore necessitating re-exploration or use of cinacalcet (Figure 2).
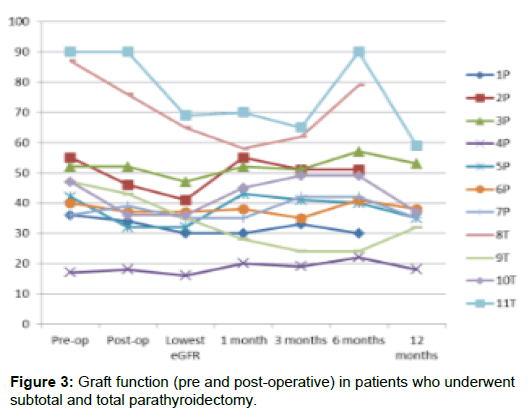
There have been some reports of adverse effects on the graft function after parathyroidectomy [9]. However, in a systematic review of 47 articles published on treatment for tertiary hyperparathyroidism, renal graft survival after surgical treatment was comparable with cinacalcet therapy. Both modalities were safe although surgical treatment appeared to have higher cure rate than medical therapy [4]. In the early post-operative period, transient reduction in graft function has been reported but function is restored in the longer term [5] (Figure 3).
Objectives
This retrospective study was done with the aims of a) comparing short term outcomes in terms of bone chemistry (Calcium, PTH) and graft function over a 12 month period between those patients that underwent subtotal parathyroidectomy (after adenoma identified on MIBI imaging) and those that had total parathyroidectomy. b) determining if there was sustained deterioration in graft function post parathyroidectomy both in the total as well as subtotal parathyroidectomy group and if there were specific causes. c) determining appropriate pre-operative loading regimes for the two groups.
Methods
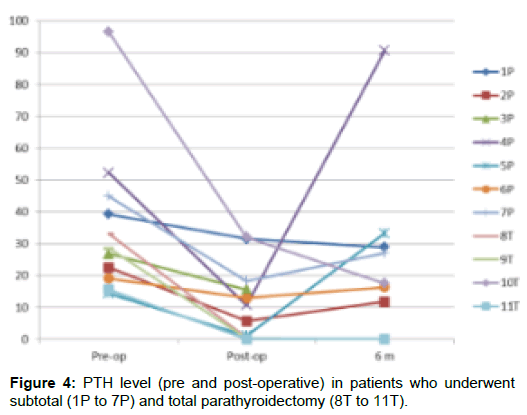
In this single centre retrospective study, we identified patients that had a parathyroidectomy post transplantation between 1/01/2007 and 1/01/2017 (n=22). Patients with failed transplants and multiple transplants were excluded on the rationale that the disease process of hyperparathyroidism is different in these individuals. Remaining 11 patients were divided into 2 groups –those that had total parathyroidectomy (TP)-n=4 vs. those that had subtotal parathyroidectomy (SP)-n=7. Graft function and bone biochemistry (Calcium, Phosphate and PTH) were recorded immediately postoperatively, at 1 month, at 3 months, at 6 months and at 12 months for all of these patients. Nadir Calcium level post-operatively and use of IV Calcium to correct hypocalcaemia were also recorded.
Demographic characteristics for each patient included age, sex and ethnicity. Details were also obtained for use of bisphosphonate therapy, use of Cinacalcet and histology of tissue obtained during surgery. Results were statistically analysed using unpaired T-test on graphpad calculator.
Results
We found that in TP group, 100% achieved normocalcaemia and in SP group 57% achieved normocalcaemia at 1 year post surgery. Calcium levels remained marginally elevated in remaining 43%. In 75% of TP group, there was sustained decline in eGFR at 1 year. Causes included profound hypercalcaemia post-operatively due to high dose of calcitriol, cellular rejection and recurrent urinary tract infections. These causes were thought not to be directly related to the surgery.
Only minor complications occurred post-op: 2 patients had cyst formation in SP group and 1 patient in TP group. IV Calcium post-operatively was required in 1 patient in TP group and in none of SP group. Histology showed adenoma in 2 specimens from SP, nodular hyperplasia in 4 specimens from SP, multinodular goitre in 1 specimen from SP and all of the 4 TP specimens showed nodular hyperplasia.1 patient from TP group had received cinacalcet prior to surgery. There was no episode of hypocalcaemia post-operatively. Calcium level was in normal range at 12 months. PTH levels dropped post-operatively in all the patients. At 6 months, 1 patient had high PTH requiring cinacalcet to be restarted. 2 patients from SP group had received cinacalcet prior to surgery. There were no episodes of hypocalcaemia post-operatively and although calcium levels were in the normal range at 12 months, PTH level was above the normal range (11.7, 16.4 pmol/L) (Figure 4).
Mean eGFR at 12 months for SP group was 40 ml/min and mean eGFR at 12 months for TP group was 60 ml/min. There was no statistically significant difference in the graft function at 12 months between the 2 groups (p=0.134).
Discussion
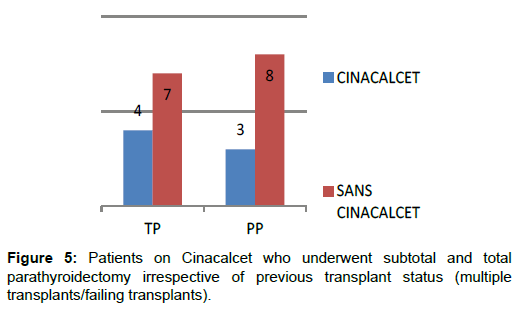
Evidence on best practice for managing hyperparathyroidism after renal transplantation is lacking. Often, the decision to treat medically or intervene surgically is based on the clinician’s discretion and availability of resources. Tailored approach of management, which takes into consideration patient’s age, co-morbidities, severity of bone mineral disease based on blood biochemistry as well as objective evidence of reduced bone mineral density (DEXA, bone biopsy) surgical expertise for parathyroidectomy and availability of cinacalcet may need to be adopted (Figure 5).
It is recognised that bone disease post-transplantation is different from CKD-MBD pre-transplantation. Corticosteroids cause rapid loss of bone mass post-transplantation by reducing bone formation as well as bone density in trabecular bones of the axial skeleton. There is an inter-play of various other factors and pre-existing osteodystrophy gets worse after transplantation.
Hip and ankle/foot fractures are the commonest after transplantation. Recent analysis of 21,769 kidney transplant recipients in UK showed that outcomes after hip fractures are poor. Hip fractures were independently associated with a threefold increase in mortality risk [17].
There are published studies which have looked at the predictors of aggressive hyperparathyroidism post-transplantation and by and large, high PTH and high Calcium levels prior to transplantation appear to be the most important biomarkers [18-27]. Dialysis vintage >6 years, calcium phosphate products >55 and cinacalcet use before kidney transplantation were found to be strong predictors of persistent hyperparathyroidism post transplantation [24]. However, PTH level alone is a poor predictor of underlying bone health and turnover. Bone biopsy is able to detect adynamic bone disease, bone density, presence of osteodystrophy or osteonecrosis. Bone biopsy with double-tetracycline labelling is the gold standard to accurately diagnose type of post-transplantation bone disease. It is not widely available and therefore its practical use in clinical practice is limited.
In a recent systematic review and meta-analysis that included 13 cohort studies and 22053 patients, parathyroidectomy treated patients had 28% reduction in all-cause mortality and 37% reduction in cardiovascular mortality as compared to medically treated patients [15].
Following table demonstrates use of cinacalcet for treating persistent hyperparathyroidism in rcent studies (Table 1). Comparison of medical therapy with surgical therapy in terms of calcium levels and bone mineral density has been demonstrated in these studies [28-40].
| [5] |
|
|
| [19] |
|
|
| [30] |
|
|
| [28] |
|
|
| [23] |
|
|
| [21] |
|
|
| [25] |
|
|
| [24] |
|
|
| [29] |
|
|
| [18]. |
|
|
Table 1: Overview of studies done using cinacalcet in renal transplant recipients.
Cinacalcet is a calcimimetic agent and it binds selectively to calcium sensing receptors in parathyroid glands and reduces serum PTH levels by enhancing the inhibitory effect of extracellular calcium ions on PTH secretion even with normal or low serum calcium levels. Cinacalcet has been shown to be an effective strategy for managing persistent hyperparathyroidism in renal transplant recipients [10,11]. Recent meta-analysis of 21 non-randomised studies with 411 patients demonstrated that cinacalcet corrected hypercalcaemia and decreased PTH levels [11]. But it is not approved for use in transplant recipients and it has been reported to cause gastrointestinal disturbances and may not be well tolerated. Cinacalcet has also been shown not to improve all-cause or cardiovascular mortality as per EVOLVE trial [16]. Correction of severe hyperparathyroidism has been shown to be similar in both surgical and Cinacalcet groups in reported studies [17].
Changes such as bone remodelling, alteration in the PTH-Vitamin D-FGF-23 axis, corticosteroid usage and other complex metabolic interactions after transplantation result in reduction of bone density, increased risk of fractures and overall increased risk of mortality [12]. It is well established that persistent hyperparathyroidism is associated with adverse cardiovascular outcomes in chronic kidney disease [13].
Denosumab is a humanised monoclonal antibody against the receptor activator of NF-KB ligand (RANKL) and it decreases bone resorption while significantly increasing bone mineral density and reducing the risk of fractures in patients with impaired kidney function. In a recent randomized controlled clinical trial in kidney transplant recipients, denosumab significantly improved bone mineral density as well as bone quality when given during the first year after transplantation [14]. As it is not renally cleared, no dose adjustment is required for reduced kidney function unlike bisphosphonates and therefore, it is considered superior to bisphosphonates for use in in patients with significant graft dysfunction, although its use has not been widely reported in renal transplant recipients [12,14].
Conclusions
From this study, we can conclude that subtotal parathyroidectomy can safely lower calcium and PTH levels in renal transplant recipients with persistent hyperparathyroidism. No requirement for IV Calcium makes subtotal parathyroidectomy more favourable in terms of reduced inpatient stay, less frequent blood monitoring and fewer complications such as thrombophlebitis from the intravenous infusion. Graft function is largely unaffected by either of the 2 types of procedures and for those that have decline in graft function post-op- in the majority, eGFR stabilises by 1 year. This is similar to other studies that have looked at impact of parathyroidectomy on graft function [9,10]. In 1 patient, graft function was affected by hypercalcaemia which causes direct vasoconstriction of the allograft and natriuresis-induced volume contraction. Negative haemodynamic effect of parathyroidectomy on renal blood flow may be augmented in the presence of calcineurin inhibitor induced renal vasoconstriction especially in the early post-transplant phase [41]. It has also been shown that PTH has vasodilatory effects on preglomerular vessels while constricting efferent arterioles, therefore, when glomerular filtration is reversed by parathyroidectomy, GFR may deteriorate acutely [42]. PTH-related protein expressed in renal tubules and vessels may also play a role in regulating graft function post-parathyroidectomy.
Longer term study is needed to determine best practice to improve long term outcomes in terms of bone biochemistry and associated morbidity. Subtotal parathyroidectomy is a safe procedure and has the added benefit of low rate of acute hypocalcaemic events as compared to total parathyroidectomy [24]. Cinacalcet is also safe and effective and may be bridging therapy or rescue therapy post parathyroidectomy for aggressive persistent hyperparathyroidism.
Adynamic bone disease and increased risk of vascular calcification has been reported with total parathyroidectomy alone (without autotransplantation). However, there is increasing evidence that systematic removal of all four parathyroid glands without autotransplantation may be treatment of choice for aggressive secondary hyperparathyroidism, for those with no access to renal transplantation and of advanced dialysis vintage [43]. Recent systematic review and meta-analysis demonstrated that total parathyroidectomy was superior for reducing risk of recurrence of secondary hyperparathyroidism and reoperation than total parathyroidectomy and auto-transplantation but comparative studies will be needed in the future due to lack of high powered randomised controlled trials [44].
References
- Heaf JG (2003) Bone disease after renal transplantation. Transplantation 75: 315-325.
- Evenepoel P, Claes K, Kuypers D, Maes B, Bammens B, et al. (2004) Natural history of parathyroid function and calcium metabolism after kidney transplantation: a single-centre study. Nephrol Dial Transplant 19: 1281-1287.
- Sprague SM, Belozeroff V, Danese MD, Martin LP, Olgaard K (2008) Abnormal bone and mineral metabolism in kidney transplant patients-a review. Am J Nephrol 28: 246-253.
- Chen J, Jia X, Kong X, Wang Z, Cui M, et al. (2017) Total parathyroidectomy with autotransplantation versus subtotal parathyroidectomy for renal hyperparathyroidism: A systematic review and meta-analysis. Nephrology Carlton 22: 388-396.
- Dulfer RR, Franssen GJH, Hesselink DA, Hoorn EJ, van Eijck CHJ, et al. (2017) Systematic review of surgical and medical treatment for tertiary hyperparathyroidism. Br J Surg 104: 804-813.
- Pitt SC, Panneerselvan R, Chen H, Sippel RS (2009) Tertiary hyperparathyroidism: is less than a subtotal resection ever appropriate? A study of long-term outcomes, Surgery 146: 1130-1137.
- Chudzinski W, Wyrzykowska M, Nazarewski S, Durlik M, Galazka Z (2016) Does the Parathyroidectomy Endanger the Transplanted Kidney? Transplant Proc 48: 1633-1636.
- Lou I, Schneider DF, Leverson G, Foley D, Sippel R (2016) Parathyroidectomy is underused in patients with tertiary hyperparathyroidism after renal transplantation. Surgery 159: 172-180.
- Yamamoto T, Tominaga Y, Okada M, Hiramitsu T, Tsujita M (2016) Characteristics of Persistent Hyperparathyroidism After Renal Transplantation. World J Surg 40: 600-606.
- Dewberry LC, Tata S, Graves S, Weber CJ, Sharma J (2014) Predictors of tertiary hyperparathyroidism: Who will benefit from parathyroidectomy? Surgery 156: 1631-1636.
- Lin Chen, Kongbo Wang, Shanlan Yu, Liping Lai, Xiaoping Zhang, et al. (2016) Long–term mortality after parathyroidectomy among chronic kidney disease patients with secondary hyperparathyroidism: a systematic review and meta-analysis. Renal Failure 38: 1050-1058.
- Ferro CJ, Arnold J, Bagnall D, Ray D, Sharif A (2015) Fracture risk and mortality post-kidney transplantation. Clin Transplant 29: 1004-1012.
- Simons M, Bautista J, Occhiogrosso R, Scott-Sheldon LA, Gohh R (2017) Acute hypocalcemia following kidney transplantation may depend on the type of remote parathyroidectomy: a retrospective cohort study, Clin Nephrol 87: 287-292
- Nakai K, Fujii H, Ishimura T, Fujisawa M, Nishi S (2017) Incidence and Risk Factors of Persistent Hyperparathyroidism After Kidney Transplantation. Transplant Proc 49: 53-56.
- Thiem U, Gessl A, Borchhardt K (2015) Long-term clinical practice experience with cinacalcet for treatment of hypercalcemic hyperparathyroidism after kidney transplantation. Biomed Res Int 2015:292654.
- Parfrey PS, Drueke TB, Block GA et al. (2015) The effects of Cinacalcet in older and younger patients on haemodialysis: the evaluation of Cinacalcet Hcl therapy to lower cardiovascular evets (EVOLVE) trial, Clin J Am Soc Nephrol 10: 791-799.
- Douthat WG, Chiurchiu CR, Massari PU (2012) New options for the management of hyperparathyroidism after renal transplantation. World Journal of Transplat 2: 41-45.
- Torres A, Lorenzo V, Salido E (2002) Calcium metabolism and skeletal problems after transplantation. J Am Soc Nephrol 13: 551.
- Borchhardt K, Sulzbacher I, Benesch T, Födinger M, Sunder-Plassmann G (2007) Low-turnover bone disease in hypercalcemic hyperparathyroidism after kidney transplantation. Am J Transplant 7: 2515-2521.
- Sirilak S, Chatsrisak K, Ingsathit A, Kantachuvesiri S, Sumethkul V (2012) Renal phosphate loss in long-term kidney transplantation. Clin J Am Soc Nephrol 7: 323-331.
- Wolf M, Weir MR, Kopyt N, Mannon RB, Von Visger J, et al. (2016) A Prospective Cohort Study of Mineral Metabolism After Kidney Transplantation. Transplantation 100: 184-193.
- Parikh S, Nagaraja H, Agarwal A, Samavedi S, Von Visger J, et al. (2013) Impact of post-kidney transplant parathyroidectomy on allograft function. Clin Transplant 27: 397-402.
- Ferreira GF, Montenegro FL, Machado DJ, Ianhez LE, Nahas WC, et al. (2013) Parathyroidectomy after kidney transplantation: short-and long-term impact on renal function. Clin Transplant 27: 397-402.
- Bouquegneau A, Salam S, Delanaye P, Eastell R. Khwaja A (2016) Bone disease after kidney transplantation. Clin J Am Soc Nephrol 11: 1282-1296.
- López V, Toledo R, Sola E, Gutiérrez C, Sujan S (2009) Treatment with cinacalcet in 29 kidney transplant patients with persistent hyperparathyroidism. Transplant Proc 41: 2394-2395.
- Zavvos V, Fyssa L, Papasotiriou M, Papachristou E, Ntrinias T, et al. (2017) Long-Term Use of Cinacalcet in Kidney Transplant Recipients With Hypercalcemic Secondary Hyperparathyroidism: A Single-Center Prospective Study. Exp Clin Transplant.
- Sharma AK, Masterson R, Holt SG, Tan SJ, Hughes PD, et al. (2016) Impact of cinacalcet pre-transplantation on mineral metabolism in renal transplant recipients. Nephrology 21: 46-54.
- Ważna-Jabłońska E, Gałązka Z, Durlik M (2016) Treatment of Persistent Hypercalcemia and Hyperparathyroidism With Cinacalcet After Successful Kidney Transplantation. Transplant Proc 48:1623-1625.
- Cruzado JM, Moreno P, Torregrosa JV, Taco O, Mast R, et al. (2016) A Randomized Study Comparing Parathyroidectomy with Cinacalcet for Treating Hypercalcemia in Kidney Allograft Recipients with Hyperparathyroidism. J Am Soc Nephrol 27: 2487-2494.
- Cohen JB, Gordon CE, Balk EM, Francis JM (2012) Cinacalcet for the treatment of hyperparathyroidism in kidney transplant recipients: a systematic review and meta-analysis. Transplantation 94: 1041-1048.
- Evenepoel P, Cooper K, Holdaas H, Messa P, Mourad G, et al. (2014) A randomised study evaluating Cinacalcet to treat hypercalcaemia in renal transplant recipients with persistent hyperparathyroidism. Am J Transplant 14: 2545-2555.
- Borchhaerdt KA, Diarra D, Sulzbacher I, Benesch T, Haas M, et al. (2010) Cinacalcet decreases bone formation rate in hypercalcaemic hyperparathyroidism after kidney transplantation. Am J Neph 31: 482-489.
- Courbebaisee M, Diet C, Timsit M-O, Mamzer M-F, Thervet E (2012) Effects of Cinacalcet in renal transplant patients with hyperparathyroidism 2010. Am J Neph 35: 341-348
- Soliman AR, Maamoun HA, Soliman MA, Darwish H, Elbanna E (2016) Cinacalcet versus Parathyroidectomy in the Treatment of Secondary Hyperparathyroidism Post Renal Transplantation. Rom J Intern Med 543: 184-189
- Cho ME, Duan Z, Chamberlain CE, Reynolds JC, Ring MS, et al. (2010) Cinacalcet improves bone density in post-kidney transplant hyperparathyroidism. Transplant Proc 42: 3554-3558
- Mawad H, Bouchard H, Tran D, Ouimet D, Lafrance JP, et al. (2017) Retrospective Study Looking at Cinacalcet in the Management of Hyperparathyroidism after Kidney Transplantation. J Transplant 2017:8720283
- Thiem U, Gessl A, Borchhardt K (2015) Long-term clinical practice experience with cinacalcet for treatment of hypercalcemic hyperparathyroidism after kidney transplantation. Biomed Res Int 2015:292654
- Wada Y, Iyoda M, Iseri K, Arai-Nunota N, Saito T, et al. (2016) Combination Therapy of Denosumab and Calcitriol for a Renal Transplant Recipient with Severe Bone Loss due to Therapy-Resistant Hyperparathyroidism. Tohoku J Exp Med 238: 205-212
- Covic A, Kothawala P, Bernal M, Robbins S, Chalian A (2009) Systematic review of the evidence underlying the association between mineral metabolism disturbances and risk of all-cause mortality, cardiovascular mortality and cardiovascular events in chronic kidney disease. Nephrol Dialysis Transplant 24: 1506-1523
- Bonani M, Meyer U, Frey D, Graf N, Bischoff-Ferrari HA, et al. (2016) Effect of Denosumab on Peripheral Compartmental Bone Density, Microarchitecture and Estimated Bone Strength in De Novo Kidney Transplant Recipients. Kidney Blood Press Res 41: 614-622
- Jeon HJ, Kim YJ, Kwon HY, Koo TY, Baek SH, et al. (2012) Impact of Parathyroidectomy on allograft otcomes in kidney transplantation. Transplant Int.
- Massfelder T, Parekh N, Endlich K, Saussine C, Steinhausen M, et al. (1996) Effect of intrarenally infused parathyroid hormone-related protein on renal blood flow and glomerular filtration rate in the anaesthetized rat. Br J Pharmacol 118: 1995-2000
- Conzo G, Perna AF, Sinisi AA, Palazzo A, Stanzione F (2012) Total parathyroidectomy without auto transplantation in the surgical treatment of secondary hyperparathyroidism of chronic kidney disease. J Endocrinal Invest 35: 8-13
- Li C, Lv L, Wang H, Wang X, Yu B, et al. (2017) Total parathyroidectomy versus total parathyroidectomy with auto transplantation for secondary hyperparathyroidism: systematic review and meta-analysis. Ren Fail 39: 678-687
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi