Research Article, Int J Glob Health Vol: 8 Issue: 1
Prevalence of Peripheral Neuropathy and Association between Cardiovascular Disease and Adult Non-Diabetic Peripheral Neuropathy in Trinidad
Adeoye Adenekan1 *, Srikanta Banerjee2
1Department of Public Health and Primary Care, Faculty of Medical Sciences, University of the West Indies, ST. Augustine, Trinidad and Tobago
2Department of Health Sciences and Public Policy, Walden University, Minneapolis, USA
*Corresponding Author: Adeoye Adenekan,
Department of Public Health and Primary Care, Faculty of Medical Sciences, University of the West Indies, ST.Augustine, Trinidad and Tobago
E-mail:Adeoye.Adenekan@uwi.ed
Received: 04 September, 2025, Manuscript No. IJGH-25-170710;
Editor assigned: 08 September, 2025, PreQC No. IJGH-25-170710 (PQ);
Reviewed: 20 September, 2025, QC No. IJGH-25-170710;
Revised: 10 October, 2025, Manuscript No. IJGH-25-170710;
Published: 17 October, 2025, DOI: 10.4172/Ijgh.1000215
Citation: Adenekan A, Banerjee S (2025) Prevalence of Peripheral Neuropathy and Association between Cardiovascular Disease and Adult Non-Diabetic Peripheral Neuropathy in Trinidad. Int J Glob Health 8:1.
Abstract
Peripheral Neuropathy (PN) is a disease of the peripheral nerves that may be insidious at onset, sometimes difficult to diagnose in the early stages, and may be associated with significant morbidity and mortality, but not necessarily so. The association between Diabetic Peripheral Neuropathy (DPN) and the development of Cardiovascular Disease (CVD) is well established. However, there are no published studies that have examined the prevalence of non-diabetic PN and its association with the development of CVD in Trinidad and Tobago and the Caribbean. Applying the socioecological model as the theoretical framework, the purpose of this crosssectional study was to determine the prevalence of nondiabetic PN and to determine whether non-diabetic PN was associated with the development of CVD, participants’ income, smoking, alcohol consumption, age, gender, and ethnicity among an adult population not suffering from diabetes in the South-Western part of Trinidad. Primary data from eight general medical practices were analyzed using binary logistic regression in SPSS. The prevalence of non-diabetic PN was 21.5%, while in adults with diabetes, the prevalence was 38.1%. CVD was significantly associated with non-diabetic PN (Odds Ratio (OR), 5.47, p<0.05, 95% CI: 1.61–18.60). Controlling for the other variables, older adults had a significantly increased risk for developing non-diabetic PN (OR, 2.70, p<0.05, 95% CI: 1.36–5.34). CVD was significantly associated with age (OR, 4.69, p<0.05, 95% CI: 1.67–13.14). Participants’ income, smoking status, alcohol consumption, gender, and ethnicity were not associated with the development of non-diabetic PN. Non-diabetic PN is insidious at onset and can be difficult to diagnose in the early stages. Patients with peripheral neuropathy not in the context of diabetes, especially older patients, should be screened for cardiovascular disease, and vice versa.
Keywords: Peripheral neuropathy, Non-diabetic, Prevalence, Adult, Cardiovascular disease, Trinidad
Keywords
Peripheral neuropathy; Non-diabetic; Prevalence; Adult; Cardiovascular disease, Trinidad
Introduction
PN, a neurologic problem encountered by family physicians and other healthcare providers, is quite common globally [1]. PN has an estimated global incidence of about 77/100,000 inhabitants per year and a prevalence of up to 30% in older people [2]. The overall prevalence of PN in adults with diabetes in the United States is 13.5%, whereas the prevalence in adults without diabetes in the United States is 11.6% [3]. Furthermore, PN is significantly associated with allcause or overall mortality (Hazard Ratio (HR)=1.49); CI, (1.15-1.94), p<0.001) [3]. In Latin America and the Caribbean (LAC), Diabetic Peripheral Neuropathy (DPN) is the most prevalent complication of diabetes mellitus, and the prevalence of DPN in LAC was 46.5% [4]. Considering that PN is associated with significant morbidity and mortality [5], from a public health perspective, this is clearly a public health burden.
Globally, CVD is a major cause of morbidity and mortality [6]. In Trinidad and Tobago, CVD accounts for approximately 33% of all annual mortality [6]. DPN, a complication of diabetes is more prevalent in the CVD group [7]. DPN in patients with CVD has been extensively studied in Trinidad and Tobago and the Caribbean. In other Caribbean countries, over 33% of people who had been diagnosed with diabetes in Barbados had evidence of PN with a loss of protective sensation [8]. Poverty and low income have been associated with poor health outcomes [9]. It is also argued that individuals with lower incomes tend to have lower educational achievements and less social capital and live in less affluent neighborhoods [9]; these situations have been shown to contribute to poor health outcomes and the development of chronic diseases such as non-diabetic PN [9], and sometimes with the attendant severe neuropathic pain [10]. Alcohol consumption and smoking have been associated with the development of non-diabetic PN [11,12]. We included these variables in the analysis since they could act as important confounders.
Non-diabetic PN usually starts through two pathologic pathways namely axonopathy and myelinopathy [13]. During axonopathy, there is an increase in calcium influx, which is attributed to the opening of ion-specific channels and, to a lesser extent, to the release from internal calcium stores, leading to the accumulation of free intracellular calcium [13]. This brief rapid rise in calcium influx leads to additional molecular events such as depletion of Nicotinamide Adenine Dinucleotide (NAD+) and adenosine triphosphate [13]. The depletion of NAD+ and adenosine triphosphate leads to impaired cellular function and energy metabolism, resulting in widespread damage within the peripheral nerves [13]. The brief rise in calcium influx also leads to the activation of calpains, and this activation of calpains leads to widespread inflammatory damage within the peripheral nerves [14]. Myelinopathy leads to the destruction of the myelin sheath, which is essential for efficient nerve signal transmission, as well as miscommunication between nerves, leading to incorrect signaling [15]. When these changes occur in organs such as the heart; it may result in the development of cardiomyopathy and cardiovascular disease, with its associated morbidity and mortality.
The theory of the socioecological model [14] was employed in this study. According to Kilanowski [14], the nature of individuals’ interaction with their physical and sociocultural environments can impact health and lead to the development of diseases. People’s income can influence their access to healthcare services or influence the choices they make about diet and their lifestyle. All these factors can ultimately affect their health outcomes and influence the development of diseases such as non-diabetic PN. By definition, nondiabetic PN encompasses all conditions, excluding diabetes, that cause damage to the Peripheral Nervous System (PNS), which may include mechanical, toxic, and metabolic causes [15]. Since non-diabetic PN is heterogeneous in its presentation and has a varied etiology, a systematic approach is critical for its evaluation and management. Non-diabetic PN can be encountered by clinicians and healthcare providers in a multitude of clinical settings [5]. This can range from a patient who presents at the emergency department with Guillain-Barre syndrome to a patient with suspected carpal tunnel syndrome requiring referral to orthopedic surgery or a patient in the oncology unit who recently developed adverse reactions to chemotherapy [5]. Globally, non-diabetic PN has been associated with a wide variety of causes such as connective tissue diseases such as amyloidosis, alcohol use, smoking, infectious diseases such as leprosy and lyme disease, nutritional deficiencies such as vitamins B6, B12, E, and thiamine deficiencies [16]. In a longitudinal study of women’s health, women who had experienced perceived discrimination in midlife had 29% higher odds of developing non-diabetic PN, when compared to women who did not report perceived discrimination [17]. The lack of information on the association between non-diabetic PN and the development of CVD was the justification for conducting this crosssectional research study in the southwestern part of Trinidad, which examined whether or not there was an association between nondiabetic PN among adults not suffering from diabetes and cardiovascular disease, income, smoking, alcohol consumption, age, gender, and ethnicity. As of 2011, the population of southwestern Trinidad was 178,410 [18]. The region is the least densely populated [18].
Materials and Methods
Study participants, design, and setting
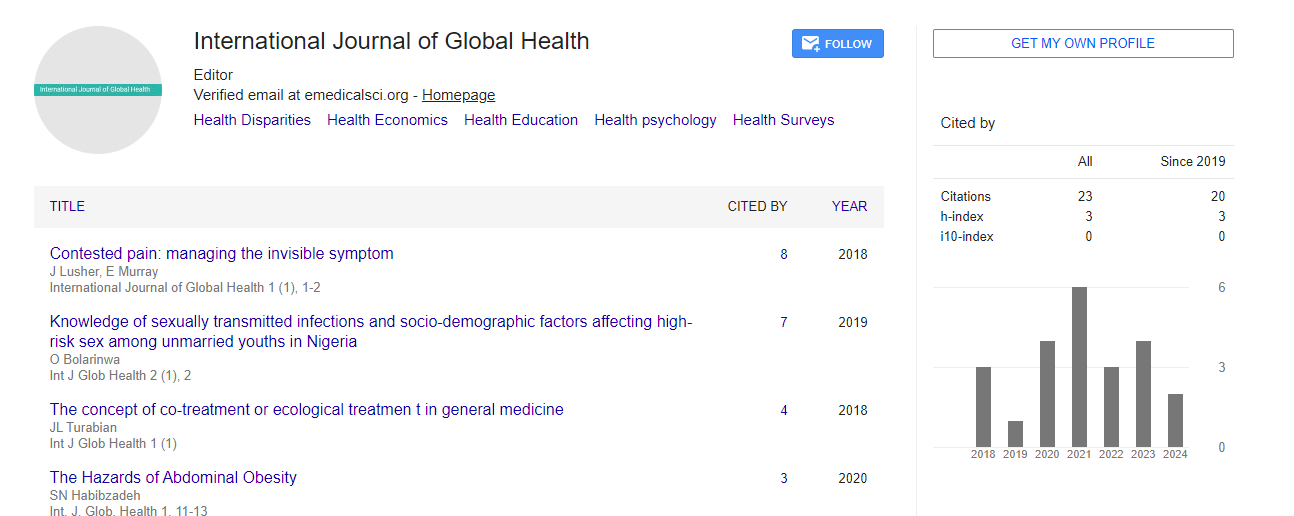
We conducted a cross-sectional study that involved the analysis of primary data to determine the prevalence of PN and whether or not CVD, income, smoking, alcohol consumption, age, gender, and ethnicity were associated with the development of non-diabetic PN in Southwestern Trinidad. The study setting was eight private general medical practices spread across the Southwestern part of Trinidad (Figure 1). The private medical practices were selected to ensure proper coverage and representation of the Southwestern part of Trinidad. The sampling frame was all adults who resided in Southwestern Trinidad and who attended any of the eight private general medical practices during the period of this cross-sectional study. Informed consent was obtained from the participants. All adults who attended any of the eight private general medical practices during the period of the cross-sectional study were included. Participants included also resided in the Southwestern part of Trinidad. Participants who did not reside in Southwestern Trinidad and declined to participate were excluded. The sample size estimated using G*Power [19] in this study, when the allowable error was 5%, was 314.
Figure 1: Map of Southwestern Trinidad showing the main cities. This image is in the public domain [20].
Variables/sources of data
The dependent variable in this study was non-diabetic PN, defined as numbness or tingling in the extremities, pain (which can be sharp), burning or throbbing, muscle weakness, sensitivity to touch, and loss of coordination and balance in a person not suffering from diabetes. The independent variables were cardiovascular disease, income, smoking, alcohol consumption, age, gender, and ethnicity. The data were primary sourced via a validated and slightly modified questionnaire. The dependent variable, non-diabetic PN, was a categorical dichotomous variable coded as Yes=1, and No=0. The independent variables were coded as follows: cardiovascular disease, Yes=1, No=0; income (monthly), TT USD 2470 to TT USD 9800=1 and above TT USD 9800=2; smoking, Yes=1, No=0; alcohol consumption, Yes=1, No=0; age, 18–49=1, 50–79=2, and 80 and above=3; gender, male=1, female=2; and ethnicity, Black=1, East Indian=2, and Other=3.
Sample recruitment
Participants were recruited at each of the eight private general medical practices spread across the Southwestern part of Trinidad. The respective physicians/medical directors of each of the eight private general medical practices were met in their offices, and the details of this research study were presented to them. With the assistance of the various clerical assistants/secretaries at the private general medical practices, potential participants were identified, and the research study explained them, including a detailed description or definition of nondiabetic PN. The participants that voluntarily consented were administered the survey questionnaires.
Data collection methods
We employed a convenience sampling at the general medical practices until the study’s sample size was attained. 319 participants were eventually recruited into the study for analysis. Data for this study were collected in 2025. Primary data on the variables of interest were collected from the participants using a slightly modified validated DN4 questionnaire, which contained seventeen questions. The DN4 questionnaire has a high diagnostic accuracy [10]. The reported sensitivity of the DN4 questionnaire was 95%, and its specificity was 96.6% [10]. The data were cleaned, entered in SPSS Version 28, and saved in a password-protected laptop only accessible to the researchers.
Ethical considerations
Before data collection, ethical approval for this study was granted by the University of the West Indies Campus Research Ethics Committee (CREC-SA.3267/04/2025) and the Ministry of Health of Trinidad and Tobago. To ensure anonymity and confidentiality, participants were de-identified at data collection by assigning each participant a unique identification number. The data collected were stored in a password-protected laptop. The data will be kept for a minimum of 5 years.
Data analysis
All analyses were conducted using SPSS software version 28. Descriptive statistics were carried out for the dependent variable (nondiabetic peripheral neuropathy) and independent variables (cardiovascular disease, income, smoking, alcohol consumption, age, gender, and ethnicity). A Chi-square test was performed to determine any significant associations between the dependent and independent variables. Bivariate logistic regression was performed to assess the association between each of the independent variables and the dependent variable. Bivariate logistic regression was also performed to assess the association between CVD and age independently.
Associations were considered significant if p<0.05. Multivariate logistic regression analysis was employed to adjust the effects of confounders and included all the variables (dependent and independent) [21].
Results
Descriptive statistics of the study participants, bivariate analysis, and multivariate analysis are shown below
In this study, the number of non-diabetic participants was 235 and 21.5% of these suffered from non-diabetic PN. Among the nondiabetic participants, only 6.8% had a history of CVD, while 59.1% earned a monthly salary of TT2470-9800 (USD 364 -1445). 51.1% of the participants were between the ages of 50 to 79 years, while females constituted 63.4% of the non-diabetic participants.
Discussion
In this study, the prevalence of non-diabetic PN was 21.5%, compared to 38.1% in the participants who suffered from diabetes (Table 1). This finding is consistent with a study in the U.S., where the prevalence of DPN was higher than non-diabetic PN [3]. A greater proportion of the participants did not suffer from CVD (93.2%), while only a small proportion had a history of CVD (6.8%). Most of the participants (59.1%) earned a monthly income of TT USD 2470-9800 (USD 364-1445), while a lesser proportion (40.9%) earned monthly income of over TT USD 9800 (over USD 1445). In this study, income was not associated with the development of non-diabetic PN (OR, 0.59, p>0.05, 95% CI: 0.27-1.27). This finding was quite unexpected, since poverty and low income have been associated with poor health outcomes [9].
| Variables | Total population | Chi-square | p | Logistic regression (Bivariate) | |||
| Non-diabetic PN (n=235) | _ | _ | OR | p | 95% CI | ||
| Yes % | No % | _ | _ | _ | _ | _ | |
| Diabetic PN | 38.1 | 61.9 | _ | _ | _ | _ | _ |
| Non-diabetic PN | 21.5 | 78.5 | _ | _ | _ | _ | _ |
| CVD | 6.8 | 93.2 | 12.06 | 0.01 | 5.42 | 0.02 | 1.91-15.38 |
| Income ($TT) | _ | _ | 0.83 | 0.36 | 0.74 | 0.36 | 0.39-1.41 |
| 2470-9800 (USD 364-1,445) | 59.1 | _ | _ | _ | _ | _ | _ |
| Over 9800 (over USD 1,445) | 40.9 | _ | _ | _ | _ | _ | _ |
| Smoking | 6 | 94 | 0.01 | 0.98 | 0.98 | 0.98 | 0.26-3.67 |
| Alcohol | 51.9 | 48.1 | 0.22 | 0.64 | 0.86 | 0.64 | 0.46-1.60 |
| Age (years) | _ | _ | 18.47 | 0.01 | 3.63 | 0.01 | 1.94-6.78 |
| 18-49 | 45.9 | _ | _ | _ | 1 | _ | _ |
| 50-79 | 51.1 | _ | _ | _ | 3.78 | 0.01 | 1.81-7.89 |
| 80 and over | 3 | _ | _ | _ | 11.76 | 0.03 | 2.32-59.51 |
| Gender | _ | _ | 3.07 | 0.08 | 0.57 | 0.08 | 0.31-1.07 |
| Male | 36.6 | _ | _ | _ | _ | _ | _ |
| Female | 63.4 | _ | _ | _ | _ | _ | _ |
| Ethnicity | _ | _ | 3.82 | 0.15 | _ | 0.16 | _ |
| Black | 49.8 | _ | _ | _ | 1 | _ | _ |
| East Indian | 24.7 | _ | _ | _ | 0.44 | 0.06 | 0.19-1.04 |
| Others | 25.5 | _ | _ | _ | 0.69 | 0.34 | 0.33-1.47 |
Table 1: Prevalence of diabetic and non-diabetic PN/characteristics of study participants. In the bivariate analysis, only cardiovascular disease and age were significantly associated with the development of non-diabetic PN.
Furthermore, 94% of the participants were non-smokers, while only 6% smoked (OR, 1.13, p>0.05, 95% CI: 0.27-4.80). Although there was an increased odd of developing non-diabetic PN from smoking, this association was not significant in this study. This finding is inconsistent with findings from other studies, where smoking was associated with the development of non-diabetic PN [11]. A probable explanation for this finding could be that most of the participants in this study were non-smokers.
Most of the participants consumed alcohol (51.9%), while a lesser proportion had no history of alcohol consumption (48.1%). In this study, there was an increased odd of developing non-diabetic PN from alcohol consumption (OR, 1.12, p>0.05, 95% CI: 0.55-2.29); however, this association was not significant. This finding is inconsistent with previous studies, where alcohol consumption was associated with the development of non-diabetic PN [12]. A possible explanation could be that the participants in this study did not engage in harmful alcohol use or consumption, as it is the harmful use or consumption of alcohol that is usually associated with many pathological conditions.
Majority of the participants in this study were females (63.4%), while males constituted a lesser proportion (36.6%). In this study, gender was not associated with the development of non-diabetic PN (OR, 0.69, p>0.05, 95% CI: 0.33-1.42). This finding is inconsistent with the finding in the study by [15], where women were found to have a higher prevalence of PN. However, in the study by [15], participants were not stratified based on their diabetes status. This could partly explain the results from that study.
For the variable age, 51.1% of the participants were between 50 and 79 years, 45.9% of the participants constituted the age range 18-49 years, while 3% of the participants were aged 80 years and over. In this study, the odds of developing non-diabetic PN was significantly associated with age (OR, 2.70, p<0.05, 95% CI: 1.36-5.34). This means there was an almost threefold increase in the odds of developing non-diabetic PN as participants aged. This finding is consistent with the results from other studies [15], where advancing age was associated with the presence of non-diabetic PN. This association between non-diabetic PN and age is not surprising because many disease processes occur probably because of the accumulation of a wide variety of cellular and molecular damage over time.
Most of the participants in this study were Black (49.8%), East Indian (24.7%), and Other (25.5%). While the Chi-square value of 3.82 indicated a strong association between non-diabetic PN and ethnicity in this study, this association was not significant (p>0.05). However, when compared to Blacks, East Indians and Others had a reduced odd of developing non-diabetic PN in this study. This finding is consistent with the results from other studies [22], where Blacks had higher odds of developing PN when compared to Hispanics and Whites. The reasons for the higher odds of developing non-diabetic PN among Blacks in this study are unclear. However, from the study by [22], individual risk factors such as poor access to health care services, lack of health insurance, and other social determinants of health, were suggested as possible reasons for the higher odds of developing PN among Blacks.
CVD was significantly associated with the development of nondiabetic PN in the multivariate logistic regression analysis, while controlling for the other variables (OR, 5.47, p<0.05, 95% CI: 1.61-18.60) (Table 2). There was more than a fivefold increase in the odds of developing CVD when participants were diagnosed with nondiabetic PN, and this association was significant. There are no previous studies conducted in Trinidad and Tobago and the Caribbean to compare this finding with. However, DPN, a complication of diabetes, is more prevalent in the CVD group [7]. This makes the finding of the association between CVD and non-diabetic PN in this study a novel one. Furthermore, in this study, CVD was significantly associated with age (p<0.05) in the bivariate logistic regression model (Table 3). The exact mechanism of the association between CVD and non-diabetic PN in this study is unclear, since important confounders of this association (smoking and alcohol consumption) were adjusted for in this study. Given the association between age and non-diabetic PN, it can be inferred in this study that the association between non-diabetic PN and CVD in this population was probably due to age.
| Variable | OR | p | 95% CI |
| Cardiovascular disease | 5.47 | 0.01 | 1.61-18.60 |
| Income | 0.59 | 0.18 | 0.27-1.27 |
| Smoking | 1.13 | 0.87 | 0.27-4.80 |
| Alcohol | 1.12 | 0.76 | 0.55-2.29 |
| Age | 2.7 | 0.01 | 1.36-5.34 |
| Gender | 0.69 | 0.31 | 0.33-1.42 |
| Ethnicity | 0.31 | ||
| Blacks | 1 | _ | _ |
| East Indians | 0.48 | 0.13 | 0.18-1.25 |
| Others | 0.89 | 0.8 | 0.38-2.13 |
Table 2: Multivariate logistic regression. In the multivariate analysis, only cardiovascular disease (p<0.05) and age (p<0.05) were significantly associated with non-diabetic PN.
|
Variable |
OR |
p |
95% CI |
|
Age |
4.69 |
0.01 |
1.67-13.14 |
Table 3: Bivariate logistic regression of cardiovascular disease and age. Cardiovascular disease was significantly associated with age (p<0.05).
Limitations
The diagnosis of non-diabetic PN was self-reported in this study. Recall bias on the part of the participants could have limited this process. Although a simple description of non-diabetic PN, including the signs and symptoms, was clearly attached to the questionnaire, participants with a low literacy level might have encountered challenges in accurately interpreting the description. This situation could have affected the prevalence of PN (both diabetic and nondiabetic) estimated in this study. Another limitation in this study was that alcohol consumption or use was not quantified. Without quantification, the association or lack of association with alcohol consumption is less definitive. The participants in this study were those who attended eight selected private medical practices in southwestern Trinidad. Hence, the prevalence of non-diabetic PN estimated in this study might not truly reflect the population prevalence. However, every effort was made to ensure that the eight selected private medical practices were strategically located to provide a good representation of Southwestern Trinidad.
Implications
This study has implications for the discipline of public health and healthcare. In this study, the prevalence of PN among participants who did not suffer from diabetes was 21.5%, which is quite high considering that non-diabetic PN is associated with morbidity and mortality. Also, the potential association between cardiovascular disease and nondiabetic PN is of public health significance.
Recommendations for further research
In this study, there was a significant association between the development of CVD and non-diabetic PN. Future research on this topic should be conducted by employing larger or population-based studies to characterize and better understand the mechanisms or pathogenesis behind this association.
Conclusion
The prevalence of non-diabetic PN among participants from this study was 21.5%. This prevalence was quite high, when compared to a prevalence of 11.6% from a study conducted in the United States. This should serve as a reminder for healthcare professionals to adequately manage people who do not suffer from diabetes but who present with the early signs and symptoms of PN in order to improve their health outcomes. Based on the results of this study, older patients who have been diagnosed with non-diabetic PN, have an increased risk of developing CVD. Hence, patients with peripheral neuropathy not in the context of diabetes, especially older patients, should be screened for cardiovascular disease, and vice versa. Based on the socioecological model, the association between non-diabetic PN, CVD, and age is not surprising, and could be due to the complex interaction between participants and their social and physical environment. Many disease processes such as non-diabetic PN and CVD occur probably because of the accumulation of a wide variety of cellular and molecular damage over time as participants aged, which can be exacerbated by chronic exposure to deleterious socioeconomic and environmental factors.
Author Contributions
A.A.: Conceptualization, methodology, formal analysis, investigation, resources, data curation, writing-original draft.
S.B.: Writing-review and editing, visualization, supervision.
All authors have read and agreed to the published version of the manuscript.
Funding
This research received no funding.
Institutional Review Board Statement
Ethical approval for this study was granted by the relevant ethics board in Trinidad. To ensure anonymity and confidentiality, participants were de-identified at data collection by assigning each participant a unique identification number. The data collected were stored in a password-protected laptop. The data will be kept for a minimum of 5 years.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data used for this study are unavailable due to privacy or ethical restrictions. However, the researchers can be contacted directly for any requests pertaining to data availability for this study.
Acknowledgments
We wish to acknowledge the support received from the physicians and the staff at the various private medical practices in Trinidad where data were collected for this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Callaghan BC, Gao L, Li Y, Zhou X, Reynolds E, et al. (2018) Diabetes and obesity are the main metabolic drivers of peripheral neuropathy. Ann Clin Transl Neurol 5: 397–405.
[Crossref] [Google Scholar] [PubMed]
- Lehmann HC, Wunderlich G, Fink GR, Sommer C (2020) Diagnosis of peripheral neuropathy. Neurol Res Pract 2: 1-7.
[Crossref] [Google Scholar] [PubMed]
- Hicks CW, Wang D, Matsushita K, Windham BG, Selvin E (2021) Peripheral neuropathy and all-cause and cardiovascular mortality in U.S. adults. Ann Intern Med 174: 167-174.
[Crossref] [Google Scholar] [PubMed]
- Yovera-Aldana M, Velasquez-Rimachi V, Huerta-Rosario A, Yupanqui M, Osores-Flores M, et al. (2021) Prevalence and incidence of diabetic peripheral neuropathy in Latin America and the Caribbean: A systematic review and meta-analysis. Plos One 16: 1-29.
[Crossref] [Google Scholar] [PubMed]
- Nold CS, Nozaki K (2020) Peripheral neuropathy: Clinical pearls for making the diagnosis. J Am Acad Physician Assist 33: 9-15.
[Crossref] [Google Scholar] [PubMed]
- Ramkhelawan S, Joseph A, Clarke R (2024) Prevalence of risk factors in cardiovascular patients in a Caribbean country: Age and sex differences. Clin Epidemiol Glob Health 29: 1-5.
- AlGhamdi G, Saati H, Almotairi E, Alsofiani BS, Kinsara AJ (2020) Peripheral neuropathy as a risk factor for developing cardiovascular disease in diabetic patients. Cereus 12: e11922.
[Crossref] [Google Scholar] [PubMed]
- Adams OP, Herbert JR, Howitt C, Unwin N (2019) The prevalence of peripheral neuropathy severe enough to cause a loss of protective sensation in a population-based sample of people with known and newly detected diabetes in Barbados: Cross-sectional study. Diabet Med 36: 1629–1636.
[Crossref] [Google Scholar] [PubMed]
- Oshio T (2019) Exploring the health-relevant poverty line: A study using the data of 663,000 individuals in Japan. Oshio Int J Equity Health 18: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, et al. (2005) Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 114: 29-36.
[Crossref] [Google Scholar] [PubMed]
- Celik SB, Can H, Sozmen MK, Sengezer Kaplan YC, Utlu G, et al. (2017) Evaluation of the neuropathic pain in the smokers. J Turk Soc Algol 29: 122–126.
[Crossref] [Google Scholar] [PubMed]
- Julian T, Glascow N, Sveed R, Zis P (2018) Alcohol-related peripheral neuropathy: A systematic review and meta-analysis. J Neurol 266: 2907-2919.
[Crossref] [Google Scholar] [PubMed]
- Schenone A, Massucco S, Schenone C, Venturi CB, Nozza P, et al. (2025) Basic pathological mechanisms in peripheral nerve diseases. Int J Mol Sci 26: 1-26.
[Crossref] [Google Scholar] [PubMed]
- Kilanowski JF (2017) Breadth of the socio-ecological model. J Agromedicine 22: 295-297.
[Crossref] [Google Scholar] [PubMed]
- Szewczyk AK, Jamroz-Wisniewska A, Rejdak K (2021) A retrospective analysis of pain etiology in middle-aged patients with peripheral neuropathy. Medicina 57: 1-13.
[Crossref] [Google Scholar] [PubMed]
- Castelli G, Desai KM, Cantone RE (2020) Peripheral neuropathy: Evaluation and differential diagnosis. Am Fam Physician 102: 732–739.
[Google Scholar] [PubMed]
- Dusendang JR, Karvonen-Gutierrez CA, Ylitalo KR (2019) The association between perceived discrimination in midlife and peripheral neuropathy in a population-based cohort of women: the study of women’s health across the nation. Ann Epidemiol 37: 10-16.
[Crossref] [Google Scholar] [PubMed]
- Central Statistical Office (2024) Population Statistics.
- Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analysis using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 41: 1149-1160.
[Crossref] [Google Scholar] [PubMed]
- Diabetes and obesity are the main metabolic drivers of peripheral neuropathy.
- Frankfort-Nachimas C, Leon-Guerrero A (2018) Social statistics for a diverse society, 8th ed.; Sage Publications: Thousand Oaks, CA, USA.
- Smyth P (2025) Known risk factors only partly explain peripheral neuropathy prevalence: Differences emerge in Hispanic, Black, and White populations. BreakingMED.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi