Case Report, J Otol Rhinol Vol: 8 Issue: 3
Reflection on the Misdiagnosis of Tonsil Malignant Lymphoma as Chronic Tonsillitis in Clinical Treatment
Feng Chen*, Qiu Xiaodong, Wang Yan and Li Yanzhong
Department of Otorhinolaryngology, Qilu Hospital of Shandong University, NHC Key Laboratory of Otorhinolaryngology, Jinan, Shandong, PR China
*Corresponding Author : Feng Chen
Department of Otorhinolaryngology, Qilu Hospital of Shandong University, NHC Key Laboratory of Otorhinolaryngology, Jinan, Shandong, P.R. China
Tel: 0531 82166791
E-mail: drfengchen@icloud.com
Received: October 09, 2019 Accepted: October 22, 2019 Published: October 22, 2019
Citation: Chen F, Xiaodong Q, Yan W, Yanzhong L (2019) Reflection on the Misdiagnosis of Tonsil Malignant Lymphoma as Chronic Tonsillitis in Clinical Treatment. J Otol Rhinol 8:3.
Abstract
The clinical data of one patient who was misdiagnosed as chronic tonsillitis and finally diagnosed as malignant lymphoma of tonsil were analyzed retrospectively. To summarize and reflect on the clinical manifestations, diagnosis and treatment of malignant lymphoma of tonsil, so as to improve the clinical understanding and diagnosis of this disease. It has been reported that the misdiagnosis rate of malignant lymphoma of tonsil is quite high, up to 41.3%.
Keywords: Tonsil malignant lymphoma; Chronic tonsillitis; Misdiagnosis
Case Presentation
The patient, a 46-year-old woman, was admitted to the hospital on May 31, 2019 with a “blocking sensation when swallowing and snoring during sleep for half a year”. The patient had no obvious incentives for swallowing six months ago, accompanied by a snoring with mouth breathing during nighttime sleep, accompanied by breath holding and occasional wakefulness. No fever, night sweats, sore throat, dyspnea and other discomfort. The patient was admitted to a local hospital and was diagnosed as "chronic tonsillitis". The patient was treated with antibiotics (unspecified) and the symptoms were not relieved. The body mass is relieved, the patient is relatively thin, and the family history of cancer and tumor is denied.
Physical examination
Bilateral tonsils are swollen with III degree, rough surface, hard surface, no congestion, pus. The bilateral inguinal lymph nodes are swollen. The cervical lymph nodes did not touch the obvious swelling, and the trachea was in the middle.
Auxiliary examination
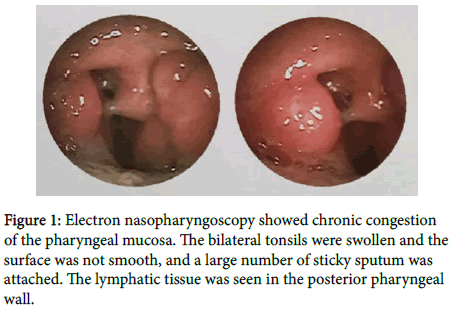
Electronic nasopharyngoscopy showed tonsil hypertrophy, a large number of lymph node hyperplasia at the base of the tongue, lymphoid follicular hyperplasia of the posterior pharyngeal wall, chronic pharyngitis (Figure 1); dynamic electrocardiogram: atrial premature beats, frequent multi-source ventricular premature beats Second degree type atrioventricular block; chest X-ray film: interstitial lung disease; ventilation diffuse function test: normal lung ventilation function, mild pulmonary diffuse dysfunction; hematuria routine is generally normal. Bilateral plasma tonsillectomy was performed under general anesthesia for chronic tonsillitis. Postoperative pathological diagnosis showed (Figure 2) (bilateral tonsil) lymphoid proliferative lesions, T-cell hyperplasia with heterotypic, prone to peripheral T-cell lymphoma, suggesting further T Cellular gene rearrangement is clearly diagnosed. Combined with medical history, clinical manifestations, and auxiliary examination, it was diagnosed as peripheral T-cell lymphoma (non-specific). The patient transferred to the hematology department to continue treatment. The follow-up is still ongoing.
Figure 2: (Bilateral tonsils) lymphoid proliferative lesions, T-cell hyperplasia with heterotypic, prone to peripheral T-cell lymphoma, suggest further diagnosis of T cell gene re-arrangement. Immunohistochemistry: CD4 diffuse (+), CD8 scattered (+), CD2 (+), CD3 (+), CD5 (+), CD20 (-), CD79a (-), CD10 (-), CyelinD1 (-), Bc1-2(+), CD21 dendritic network (+), CD43(+), LEF1(+), CD23(-), S0X11(-), Bc1-6(-), CK(+), ALK( -), CD30 focal (+), PD-1 focal (+), CD56 (-), EBER (-), Ki-67 positive rate of 30%.
Discussion
The tonsil belongs to the Webster's ring structure and is a common site of the pharyngeal lymphatic ring non-Hodgkin's lymphoma (NHL), while Hodgkin's lymphoma (HL) rarely invades the Wechsler ring [1]. The etiology of HL is unknown, but EB virus genome fragments can be detected in RS cells of about 50% of patients. Patients with known immunodeficiency and autoimmune diseases have an increased risk of Hodgkin's lymphoma. Malignant lymphoma of the tonsils is a common extranodal lymphoma, accounting for more than 60% of the lymph nodes of the pharynx, accounting for 35% of head and neck lymphoma, and 4.7% of systemic lymphoma [2]. The rate of misdiagnosis of tonsil malignant lymphoma is quite high, as reported in the literature, reaching 41.3% [3]. Primary tonsil non-Hodgkin's lymphoma is often the first symptom of tonsil enlargement and sore throat discomfort. The following three types can be found clinically:
Obstructive type
Rapid growth, no ulcer, large tumor, hindering swallowing and breathing.
Inflammatory type
Repeated inflammatory attacks, elevated body temperature, such as acute tonsillitis, but not easy to completely disappear.
Early metastatic type
Local lesions are not significant and early cervical lymph node metastasis. Lymphoma can occur simultaneously in bilateral tonsils or into sarcoma leukemia. Cervical lymphadenopathy is an early manifestation of tonsillar malignant lymphoma. In the advanced stage, multiple lymph nodes can be found in the whole body. The examination is easy to be detected [4]. In this case, there is no lymph node enlargement in the neck. There is also the lack of clinical experience of the author as a low-grade doctor. The above reasons lead to the initial diagnosis of the case, the main reason for misdiagnosis is the lack of specificity of the clinical manifestations of tonsillar malignant lymphoma, early manifestations are often atypical, mostly non-specific manifestations such as sore throat, pharyngeal foreign body sensation, swallowing obstruction, which were difficult to distinguish from chronic tonsillitis clinically. The secondary cause is often misdiagnosis of pathology, but this case is an exception. The early tumor cells of tonsillar malignant lymphoma mainly proliferate in the submucosal lymphoid tissue. In addition, tonsillar malignant lymphoma is often associated with tonsillitis, and local biopsy is difficult to obtain tumor tissue at one time.
Methods to reduce misdiagnosis
If bilateral tonsils are significantly unequal, grow rapidly, form ulcers, and have a smooth surface like children's tonsils, accompanied by cervical lymph node swelling and no acute inflammatory manifestations, the possibility of malignant tonsil lymphoma should be suspected, and tonsil biopsy should be performed first. Appropriate biopsy is necessary for the evaluation and treatment of all patients with non-hodgkin's lymphoma, and appropriate treatment requires accurate typing. If a tonsil malignancy is suspected and multiple biopsies are not confirmed, the tonsil biopsy can be removed. If there is a high degree of suspicion of tonsil malignant lymphoma, CT should be performed in imaging studies to see if the surrounding tissues and organs are involved, and whether important nerves and blood vessels are invaded [5]. If necessary, positron emission tomography (PET) imaging is required to determine whether the tumor has metastasis or malignancy. PET is a new imaging technology that can monitor the range of tumors in the body and determine the specific location of the lesions. Clinically, patients with chronic tonsillitis have a fast turnover rate after admission. Generally, patients can be discharged 3 to 5 days after admission. Sometimes due to poor specimen collection and pathological morphology, pathological returns are slow, and patients are not required to pay attention to discharge. The doctor should do the explanation work as much as possible, and make decisions after the pathological return. Remember that pathological diagnosis is the only gold standard [6]. If the pathology is malignant, the diagnosis should be corrected to avoid missed diagnosis, misdiagnosis, and timely postoperative radiotherapy and chemotherapy treatment, which helps to improve patient survival [7].
Conclusion
The treatment of lymphoma has made significant progress in recent years. Most of Hodgkin's lymphoma can be cured. Although the efficacy of non-Hodgkin's lymphoma is not as good as that of Hodgkin's lymphoma, some cases have been cured. At present, malignant lymphoma is mainly treated by comprehensive therapy, which means that according to different tumors, different pathological types, different disease stages and development trends, different behavioral states of the body and important organ functions, existing treatment means are applied to protect the body and kill tumor cells to the maximum extent, so as to achieve the goal of improving the cure rate. The treatment of malignant lymphoma is a comprehensive treatment based on chemotherapy. Therapeutic measures include chemotherapy, radiotherapy, surgery, and biological therapy. Through this comprehensive treatment, the patient can be completely relieved or partially cured.
References
- Yin W (2008) Tumor radiotherapy [M]. 4th (Edn.) Beijing: China Union Medical University Press, 686.
- Nan K, Wei Y, Li C (2002) Survival analysis of 128 cases of primary extranodal lymphoma[J]. Journal of the Fourth Military Medical University 23: 1343-1344.
- Wang W, Zhou X (2005) Misdiagnosis of 62 cases of tonsil malignant lymphoma[J]. Modern Oncol Med 2: 265-266.
- Williams MD, Brown HM (2003) The adequacy of gross pathological examination of routine tonsils and adenoids in patients 21 years old and younger [J]. Hum Pathol 34: 1053-1057.
- Wang R, Liu Y (2015) CT diagnosis of primary tonsil lymphoma[J]. Xinjiang Medical Journal 2015: 367-369.
- Fan H (2017) A case of misdiagnosis of tonsil malignant lymphoma [J], using clinical medicine. 18: 73-74.
- Gao Y, Li Y, Yuan I (2002) Prognostic factors in patients with primary non-hodgkin’s lymphoma of the tonsil [J], Zhong hua zhong liu za zhi 25: 483-485.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi