Research Article, J Spine Neurosurg Vol: 6 Issue: 4
Remote Cauda Equina Syndrome Due to Overgrowth of Epidural Free Fat Graft: Case Report
Abolfazl Rahimizadeh*, Ava Rahimizadeh, Valiolah Hassani and Shaghayegh Rahimizadeh
Pars Advanced and Minimally Invasive Manners Medical Center, Pars Hospital, Tehran, Iran
*Corresponding Author : Dr. Abolfazl Rahimizadeh
Department of Neurosurgery & Spinal Surgery, Pars Hospital. Address: 83 Keshwarz Blvd, Tehran, Iran
Tel: +989123226149
E-mail: a_rahimizadeh@hotmail.com
Received: September 04, 2017 Accepted: September 21, 2017 Published: September 28, 2017
Citation: Rahimizadeh A, Rahimizadeh A, Hassani V, Rahimizadeh S (2017) Remote Cauda Equina Syndrome Due to Overgrowth of Epidural Free Fat Graft: Case Report. J Spine Neurosurg 6:4. doi: 10.4172/2325-9701.1000279
Abstract
Lumbar discectomy is being done in increasing frequency worldwide where formation of epidural scar formation has been known as a common cause of its failure. Application of a free fat graft despite controversies has been widely used to prevent further adhesion and post-laminectomy scarring. Single nerve root compression and cauda equina syndrome due to compressive effect of free fat graft with a few days to weeks after laminectomy is well known early complication of lumbar discectomy. However, late neurological deficit as the result of significant increase of fat graft volume has been not addressed previously in the literature. Herein, the authors present a middle-age man who was admitted with cauda equina syndrome for one day duration developing 11 years after a redo laminectomy for recurrent disc herniation and local stenosis. The MRI obtained urgently revealed significant overgrowth of the free fat graft that had been already used for prevention of scar formation. Piecemeal surgical removal of fat with clearance of the theca and the corresponding nerve roots result in steady but good recovery within a few weeks. To our knowledge, although overgrowth of fat has been reported in other locations, but this is the first example occurring after its application at the site of laminectomy. Therefore, overgrowth of free fat graft should be added to all previously describe unusual complication of lumbar discectomy.
Keywords: Cauda equina syndrome; Lumbar discectomy; Epidural scar
Introduction
Lumbar discectomy is being done in increasing frequency worldwide where formation of epidural scar formation has been known as a common cause of its failure. Up to 20% of the patients undergoing lumbar discectomy might suffer from this complication. Rocca and Mc.nab were the first who reported the scenario of post-laminectomy peridural fibrosis and called it the laminectomy membrane [1].
Subsequently, preliminary experience indicating that adipose tissue acts as a barrier to fibrosis was reported by Langenskiöld and Kiviluoto in two separate papers in 1976 [2,3]. Subsequently, In 1978, Barber et al. used a layer of free fat graft for prevention of epidural fibrosis formation for the first time [4].
In the same year, Keller demonstrates the fate of epidural free fat graft (FFG) [5]. Since then, several clinical studies in favor of epidural free fat graft application for reducing peridural fibrosis was published so far [6-9].
The general concept was that the graft’s adipose tissue remodels in relation to the bony defect and acts like a greasy fluid permitting gliding of the roots and the dural sac on it [8].
Later, with popularity of fat transplantation either as an epidural barrier in neurosurgery or as a filler in plastic and reconstructive surgery, its natural behavior became more evident. Corresponding studies about the longevity and durability of transplanted adipose tissue showed that it remains alive despite shrinkage and reduction in size with time. The concept of survival of the grafted fat made the neurosurgeons to use it more and more with time. In particular, once the superiority of FFG in compare to other material was published [10].
However, the benefits derived from application of epidural fat graft became questionable when the uncommon early drawbacks of its application in a spectrum from acute radiculopathy to cauda equina syndrome were verified [11-18].
Later, with consideration of several new studies, its real value in prevention of postoperative scar tissue formation and late radiculopathy became more controversial [19-22].
A few unusual events, remote overgrowth of free fat with its significant increase in its volume was reported by plastic surgeons [23,24].
Recently in our practice, we faced a 49-year old male with remote cauda equina syndrome due to significant overgrowth of free fat graft which was used as an epidural layer eleven years earlier. Meticulous decompression of the theca and the nerve roots achieved with piecemeal excision of a large mass composed of adipose tissue result in steady but good recovery of the patient. To the best of our knowledge, enlargement of epidural free fat graft over time to such a considerable degree that can cause remote neurological deficit has been not reported previously.
Case Report
A 49-year-old male was admitted to our department because of pain and the weakness of the lower extremity for a 4 days and difficulty in voiding for 24 hours. In his past history, he had three time surgery for L5-S1 discectomy, partial laminectomy for L4-L5 stenosis and recurrent L5-S1 disc herniation and L4-L5 block in the last 17 years. The first two surgeries had been done in other hospitals but the last surgery was done in our department where after removal of the recurrent disc at L5 –S1 and laminectomy of L5 and partial L4, in order to prevent epidural fibrosis, the dura was covered with 4mm layer of fat, composed of free fat globules. On his recent admission, neurological examination revealed weakness of dorsiflexion ob both sides, with score of 3/5 on the right and 4/5 on the left. Ankle jerks were diminished bilaterally; hypoesthesia of saddle region was also present more on the left side. A Foley catheter had been already used because of urinary retention.
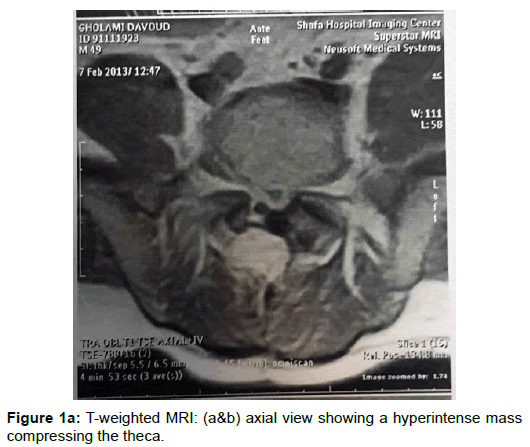
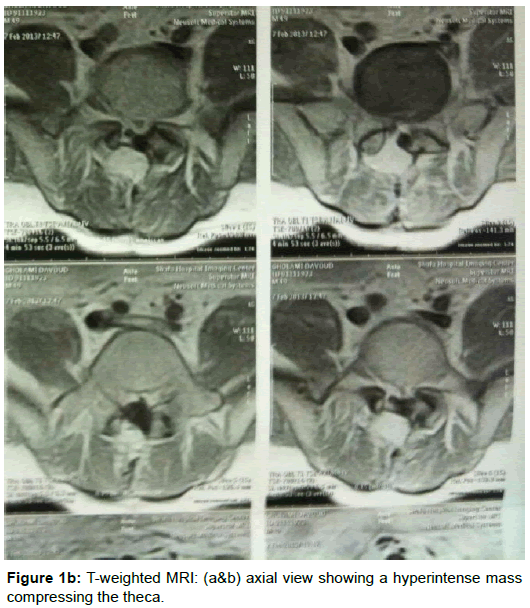
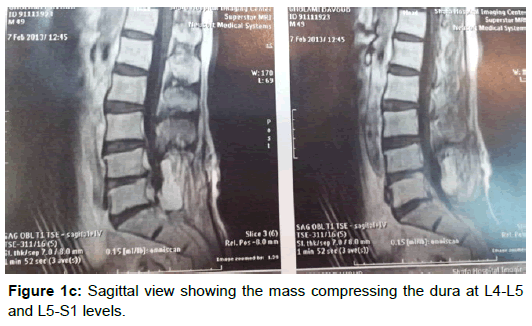
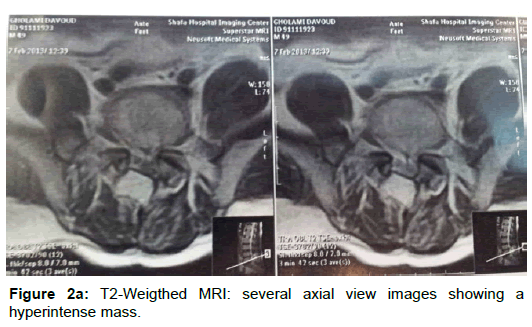
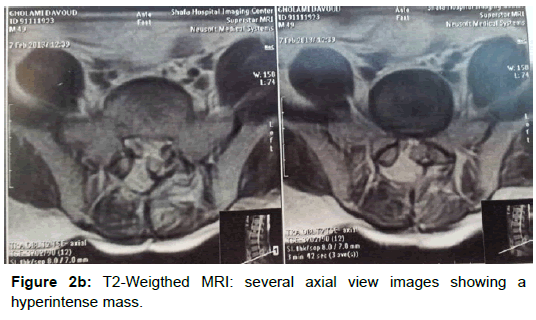
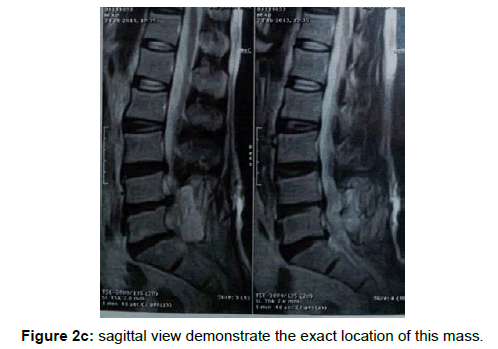
MRI demonstrate a rather large hyperintense mass starting at the laminectomy defect at L4L5 and extending to the fascia in T1- weighted images (Figure 1a-c). T2-weighted images demonstrated the same mass with hyperintensity, compressing the corresponding roots and theca (Figure 2a-c). Hyper intensity both in T1 and T2-weighted images were in favor of the overgrowth of free fat graft.
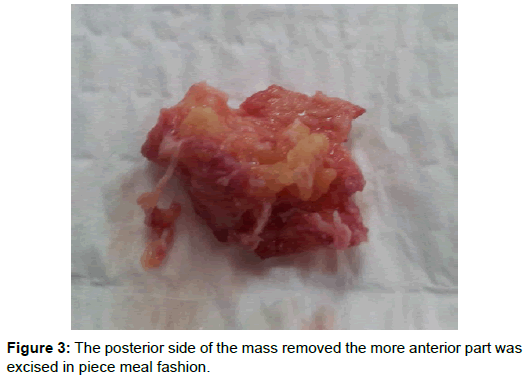
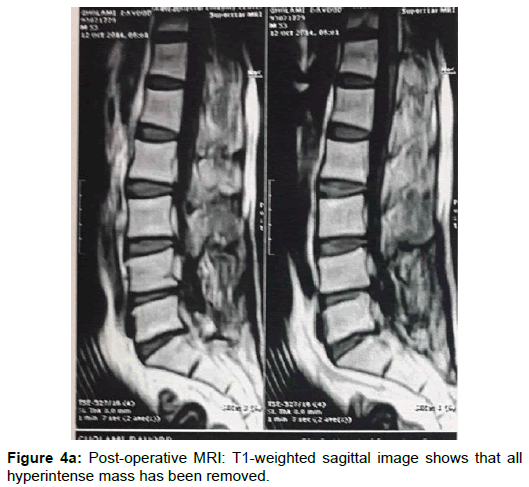
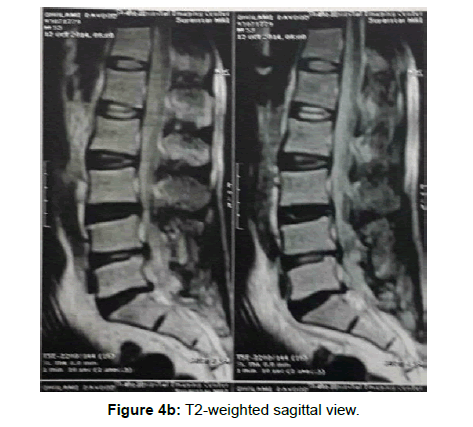
Exploration and decompressive surgery was proposed, being accepted by the patient and his family. Therefore, urgent intervention was started after general anesthesia and the patient in prone position. Via a midline incision, fascia was opened where on the left, side immediately after facial opening, an adipose mass was demonstrated. Initially, the adipose mass was dissected from the surrounding paravertebral muscles. In order to ease surgery, the posterior aspect of the mass was removed (Figure 3). Subsequently, the remaining fat tissue was removed in piece meal fashion till the dural and the corresponding roots at the depth of the field were demonstrated. With the aid of the microscope, its adhesions to the dura and L5 roots were meticulously detached as much as was possible. Thereafter, the wound was closed in three layers. Post-operative course was uneventful and motor function, sensory disturbances, voiding problems and sphincter control improved steadily within two months. Post-operative MRI obtained 3 months later showed no more adipose mass (Figure 4a,b) (Supplementary Figures 1-4).
Discussion
With popularity of lumbar disc surgery worldwide, the number of the cases being affected by failed back scenario or harboring unusual and rare complications have increased dramatically [25-29]. Postoperative epidural fibrosis is regarded as a major cause of failed back and recurrence of radiculopathy after lumbar discectomy. In the last two decades of the 20th century, the use of autogenous subcutaneous fat grafts in an attempt to prevent epidural and perineural fibroses after lumbar laminectomy became popular [1-9]. It was postulated that epidural fat graft can preserve epidural space from fibrosis, with positive effect in reducing the chance of failed back syndrome or making redo surgeries technically easier [1-9]. These effects were over emphasized to such an extent the many surgeons used it routinely after laminectomy. Subsequently, once it was shown that free fat graft (FFG) works well than other materials studied for reducing epidural fibrosis, its application became more accepted [10].
Parallel to these studies the natural fate of FFG regardless of the territory that it is used was assessed and this showed that transplanted adipose tissue survives despite its primary shrinkage [30-35]. In epidural space, based on animal surveys, the fat globules remains alive and are reshaped along the dura mater where its quality remains unchanged overtime. According to Kanamori et al. the size of the grafted fat is reduced to approximately 57% after 42 days, and to about 33% after 1 year [20-35]. This means that although fat grafts remain alive, but they lose approximately 70% of its original size with time retaining the characteristic features of normal fat.
Viability and durability of transplanted free fat graft has been assessed both with CT scan and MRI [33-35].
Accordingly, in the early stage and within 6 weeks after surgery, the signal intensity of the grafted fat remains lower than that of normal subcutaneous fat tissue, but its intensity recovers by 1 year after surgery. Increasing experience has showed that free fat graft might be visible in MRI up to 18 years after utilization [35,36].
As was described earlier free fat graft has been used worldwide for about three decades, till one prospective double blind study and one prospective triple blind study found no significant clinical differences between the free fat-graft group and a control group [19-22].
With respect to the results of these studies, some surgeons proposed its abundance, relying on the increasing reports of serious early post-operative complications resulting from the compressive effect of free fat graft on the nerve roots and cauda equina [11-18]. With consideration of these facts which had stressed on postoperative neurological deficit and its inefficacy of in prevention of postlaminectomy fibrosis, application of FFG has become modified and limited to the defect of fenestration not exceeding than 4 mm in thickness.
Furthermore, with regard to our present case report, overgrowth of free fat graft should be added to the previously described complications [23,24]. It has been observed that transplanted free fat might continuously grow instead of shrinkage, a scenario that has been demonstrated clinically in plastic and ENT surgery where fat is used as a filler . In such circumstances, re-growth of the free fat graft is postulated to be due to its revascularization, the scenario that might be need periodic evaluation, both clinically and with repeat MRI. Otherwise, MRI should be done whenever new signs and symptoms of root compression appear and in particular urgently if cauda equina syndrome exist. In MRI a large pear-shape mass, with hyperintensity both in T1 a T2-weighted image is a clue and indicative of hypertrophied fat tissue.
Excision of such adipose pathology can be achieved with meticulous microsurgical piece meal removal of the mass and release of its attachments from the dura and affected nerve roots.
In conclusion, the complications of free fat graft placed over the dura should not be confined to early post-operative period. But, with regard to the current case, remote neurological deficit due to a considerable overgrowth of free fat graft should be regarded as another rare complication of lumbar disc surgery. The outcome might be satisfactory, if the surgical decision is made soon after appearance of new neurological deficit.
Ethical approval
Written informed consent was obtained from the patient for publication and corresponding images.
Consent
Written informed consent was obtained from the patient for publication and corresponding images.
Contribution
The steps of this article from design to writing were made by A. Rahimizadeh, S Rahimizadeh, Ava Rahimizadeh and Valliolah Hassani retrospectively.
References
- LaRocca H, Macnab I (1974) The laminectomy membrane: studies in its evolution, characteristics, effects, and prophylaxis in dogs. J Bone Joint Surg 56: 545-550
- Langenskiold A, Kiviluoto O (1976) Prevention of epidural scar formation after operations on the lumbar spine by means of free fat transplants: a preliminary report. Clin Orthop115: 92-95.
- Kiviluoto O (1976) Use of free fat transplants to prevent epidural scar formation. An experimental study.Acta Orthop Scand 164: S3-S75.
- Barber J, Gonzalez J, Esquerdo J (1978) Prophylaxis of the laminectomy membrane: an experimental study in dogs. J Neurosurg 49: 419-424
- Keller JT, Dunsker SB, McWhorter JM (1978) The fate of autogenous grafts to the spinal dura: An experimental study. J Neurosurg 49: 412-418.
- Jacobs RR, McClain O, Neff JR (1980) Control of postlaminectomy scar formation: an experimental and clinical study. Spine 5: 223-229.
- Gill GG, Sakovich L, Thompson E (1979) Pedicle fat grafts for the prevention of scar formation after laminectomy: an experimental study in dogs. Spine 4: 176-186.
- Bryant MS, Bremer AM, Nguyen TQ (1983) Autogeneic fat transplants in the epidural space in routine lumbar spine surgery. Neurosurgery 13: 367-370.
- Gill GG, Schck M, Kelley ET (1985) Pedicle fat grafts for the prevention of scar in low-back surgery: a preliminary report on the first 92 cases. Spine 7: 662-667
- Quist JJ, Dhert WJA, Meij BP, Visser WJ, Oner FC, et al. (1998) The prevention of peridural adhesions: a comparative long-term histomorphometric study using biodegradable barrier and fat graft.J Bone Joint Surg 80B: 520-526
- Cabezudo JM, Lopez A, Bacci F (1985) Symptomatic root compression by a free-fat transplant after hemilaminectomy. J Neurosurg 63: 633-635
- Cobanoglu S, Imer M, Ozylmaz F, Memis M (1995) Complication of epidural fat graft in lumbar spine disc surgery: case report. Surg Neurol 44: 479-481.
- Israel Z, Constantini S (1995) Compressive autologous free fat graft in a patient with failed back syndrome: case report. J Spinal Disord 5: 240-242.
- Ohmori K, Kanamori M, Ishihara H (2000) Cauda equina syndrome caused by a free-fat graft after decompressive surgery of the lumbar spine: Report of two cases. Neuro-orthopedics 27: 1-5.
- Prusick VR, Lint DS, Bruder WJ (1988) Cauda equina syndrome as a complication of free epidural fat grafting. J Bone Joint Surg 70: 1256-1258.
- Henriques T, Olerud C, Petren-Mallmin M, Ahl T (2001) Cauda equina syndrome as a postoperative complication in five patients operated for lumbar disc herniation. Spine 26: 293-297.
- Imran Y, Halim Y (2005) Acute cauda equina syndrome secondary to free fat graft following spinal decompression. Singapore Med J 46: 25-27.
- Israel Z, Constantini S (1995) Compressive autologous free fat graft in a patient with failed back syndrome: case report. J Spinal Disord 5: 240-242.
- Martin-Ferrer S (1989) Failure of autologous fat grafts to prevent postoperative epidural fibrosis in surgery of lumbar spine. Neurosurgery 24: 718-721.
- Bernsmann K, Krämer J, Ziozios I, Wehmeier J, Wiese M (2001) Lumbar micro disc surgery with and without a autologous fat graft. A prospective randomized trial evaluated with reference to clinical and social factors. Arch Orthop Trauma Surg 121: 476-480.
- Gorgulu A, Simsek O, Cobanoglu S, Imer M, Parsak T (2004) The effect of epidural free fat graft on the outcome of lumbar disc surgery. Neurosurg Rev 27: 181-184.
- Jensen TT, Asmussen K, Berg-Hansen EM, Lauritsen B, Manniche C, et al. (1996) First-time operation for lumbar disc herniation with or without free fat transplantation. Prospective triple blind randomized study with reference to clinical factors and enhanced computed tomographic scan 1 year after operation. Spine 21: 1072-1076
- Miller JJ, Popp JC (2002) Fat hypertrophy after autologous fat transfer. Ophthal Plast Reconstr Surg 18: 228-231.
- Dejonckere PH, van Wijngaarden HA (2001) Retropharyngeal autologous fat transplantation for congenital short palate: a nasometric assessment of functional results. Ann Otol Rhinol Laryngol 110: 168-172.
- Teixeira R, Reid JA, Greensmith A (2011) Fatty hypertrophy cause obstructive sleep apnea after fat Injection for velopharyngeal incompetence. Craniofacial Journal 48: 473-477.
- Rahimizadeh A, Habibi GR, Sharifi G (2012) Intraspinal retained cotton patty: Report of an extremely rare case and review of the literature. World Spinal Column J 3: 24-28.
- Rahimizadeh A, Kaghazchi M, Rahimizadeh A (2014) Post-Laminectomy Lumbar Pseudomeningocele; Report of Three Cases and Review of the Literature. World Spinal Column J 4: 103-108.
- Rahimizadeh A, Hadadi K (2016) Is transforaminal retrieval of intradiscal deeply seated broken surgical knife all times pars sparing. International J surg case Reports 19: 131-133.
- Rahimizadeh A, Ghorbani E, Rahimizadeh S (2013) Transformational retrieval of intradiscal retained broken surgical knife blade. Spine 38: E1278-E1281.
- Rahimizadeh A, Rahimizadeh S, Amirzadeh M (2017) intradiscal retained broken blade of a disc rongeur. J Spine & Neurosurg 6: 3.
- Saunders MC, Keller JT, Dunsker SB (1981) Survival of autologous fat grafts in humans and in mice. Connect Tissue Res 8: 85-89.
- Weisz GM, Gal A (1986) Long-term survival of a free-fat graft in the spinal canal. Clin Orthop Res 205: 204-206.
- Sommer B, Sattler G (2000) Current concept of free fat graft survival: Histology of aspirated adipose tissue a nd review of literature. Dermatology Surgery 26: 1156-1166.
- Langenskio¨ ld A, Valle M (1985) Epidurally placed free-fat grafts visualized by CT scanning 15–18 years after discectomy. Spine 10: 97-98.
- Van Akkerveeken PF, Van De Kraan W, Muller JW (1986) The fate of the free-fat graft: a prospective clinical study using CT scanning. Spine 11: 501-504.
- Kanamori M, Kawaguchi Y, Ohmori K, Kimura T, Tsuji H, et al. (2001) The fate of autogenous free-fat grafts after posterior lumbar surgery: part 2. Magnetic resonance imaging and histologic studies in repeated surgery cases. Spine 26: 2264-2270.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi