Case Report, J Surg Clin Pract Vol: 2 Issue: 2
Secondary Acute Myocardial Infarction in a Young Man with Systemic Lupus Erythematosus
Zhirui Zhu, Juntao Wang, Yongen Shi, Haijia Yu, Huihui Song and Yingjie Chu*
Departement of Cardiology, Zhengzhou University People’s Hospital, Zhengzhou, Henan,China
*Corresponding Author : Yingjie Chu
Department of Cardiology, Henan Province People’s Hospital, Zhengzhou, Henan, China
Tel: +86 13937199780
E-mail: hnqbdsl@126.com
Received: December 06, 2017 Accepted: March 17, 2018 Published: March 24, 2018
Citation: Zhu Z, Wang J, Shi Y, Yu H, Song H, et al. (2018) Secondary Acute Myocardial Infarction in a Young Man with Systemic Lupus Erythematosus. J Surg Clin Pract 2:2.
Abstract
We describe the case of a young man with systemic lupus erythematosus (SLE) who suffered secondary acute myocardial infarction (AMI). Before primary acute myocardial infarction, the patient had a history of a large dose of hormone application. Then he has been taking hydroxychloroquine treatment. Eventually, it occurred in unexplained acute myocardial infarction for the second time.
Keywords: Myocardial Infarction; Lupus Erythematosus
Introduction
Primary myocardial infarction with SLE is rare, secondary myocardial infarction is exceedingly rare, while other cardiac manifestations like pericarditis and myocarditis are more frequent [1]. We report the case of a 34-year-old man with SLE who developed secondary acute myocardial infarction.
Case Report
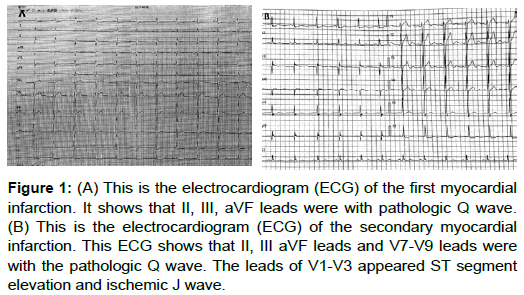
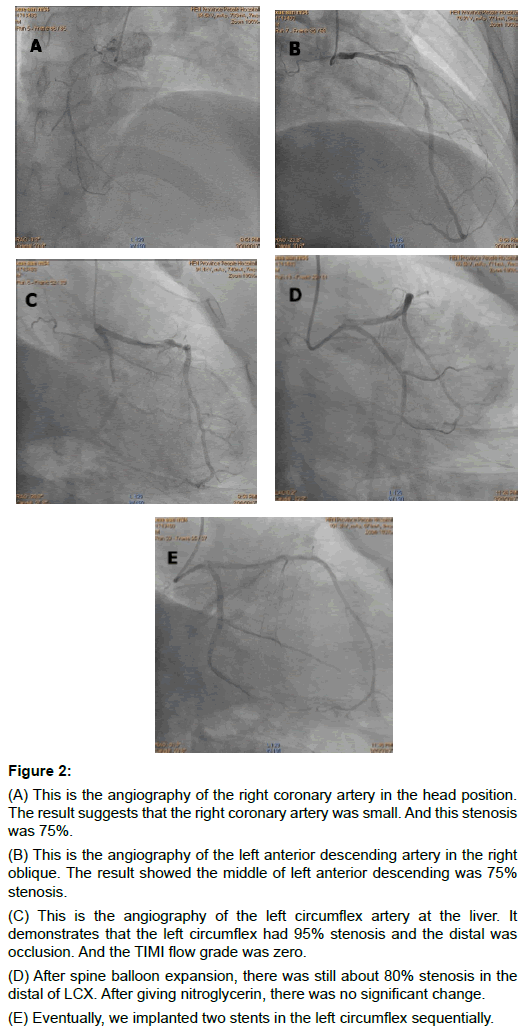
A 34-year-old man with the 21-year history of SLE had a longterm use of prednisone treatment. He suffered a sudden chest tightness one year ago. Then he conducted Electrocardiogram(ECG) showing: IIã€ÂIIIã€ÂaVF leads with pathologic Q wave. At the same period, he conducted 64-row of coronary CTA inspection showing: no abnormal coronary artery. Five hours before admitting the hospital, the patient appeared unrelieving chest distress while he had a rest. Next then he conducted ECG showing: II IIIã€ÂaVF leads and V7-V9 leads with the pathologic Q wave. The leads of V1-V3 appeared ST segment elevation and ischemic J wave. There are the results of auxiliary examination. The urine protein was positive (+++); the antinuclear antibodies (IF) was negative (-). The 24-hour urinary protein was 3.70g. The blood sedimentation was 44mm/h. The double-stranded DNA antibodies (IF) was 1:32 resistance. The cTnI enzyme peak was 2.70ug/L. The level of pro-BNP was 1380ng/L. On the seventh day after admission, he carried out the coronary angiography in the basic treatment of ant ithromboticã€Âanticoagulationã€Âlipid adjusting. It demonstrated that left circumflex had 95% stenosis and the distal was occlusion, TIMI flow grade 0; the middle of left anterior descending was 50% stenosis. Right coronary artery stenosis was 75%. In the left circumflex, we implanted two stents sequentially.
Discussion
SLE is a systemic and immune-mediated disease with the outstanding performance of immune inflammation diffuse connective tissue [2], often involving multiple systems. The main pathological changes of SLE are inflammatory reaction and vascular abnormalities, small and medium vessels by immune complex deposition or antibodies directly affect the inflammation and necrosis of the tube wall, subsequent thrombus lumen narrowing, resulting in local tissue ischemia and dysfunction [3].
Currently, SLE is an independent risk factor of coronary atherosclerosis. And SLE is prominent with immune inflammation, which could cause endothelial dysfunction, involving the coronary arteries, angina pectoris and ECG changes, even appearing AMI. That ECG showed ST-T change and ischemic J wave formation of the urgent period. The pathogenesis of SLE complicated with AMI is that caused by long-term use of hormones. Besides coronary arteritis, that could cause the lipid metabolism disorders which could accelerate atherosclerosis and secondary high coagulation state for antiphospholipid antibodies. These conditions could cause arterial thrombosis and contribute to AMI. In addition to these circumstance, it may also be related to coronary artery aneurysms and coronary artery spasm (Figure 1).
Figure 1: (A) This is the electrocardiogram (ECG) of the first myocardial infarction. It shows that II, III, aVF leads were with pathologic Q wave. (B) This is the electrocardiogram (ECG) of the secondary myocardial infarction. This ECG shows that II, III aVF leads and V7-V9 leads were with the pathologic Q wave. The leads of V1-V3 appeared ST segment elevation and ischemic J wave.
Bruce etc. [4] found that coronary artery lesions may be from the original non-obstructive coronary artery occlusive events or thrombosis inflammation to coronary atherosclerosis, along with the development of SLE. The incidence of SLE with primary AMI is very rare and of SLE with secondary AMI is extremely rare. Literature reported that the main cause of death in the acute phase of SLE is the multiple organ failure and infection. The forward phase of SLE is mainly the cardiovascular diseases. Now the cardiovascular diseases are the important factors of death in patients with SLE. There is a high incidence of this disease in young people and these patients do not possess traditional coronary heart disease risk factors. Clinical chest tightness, chest pain and discomfort in the first time to these patients, it’s liable to missed diagnosis or misdiagnose easily.
Analyzing this example of secondary AMI, it may be associated with long-term use of hormone. Obesity, hyperlipidemia, the history of myocardial infarction (MI) and other traditional risk factors for coronary heart disease (CHD), lead to the coronary atherosclerosis, non-obstructive vasospasm, even coronary occlusion lesions. Manager [5] found that these factors in young woman with SLE, such as smoking, renal impairment, high levels of C3, hormone, accumulative total more than 30 g, are the most important risk factors for vascular atherosclerosis. Compared with female, male SLE patients are comparatively rare. The imaging results of this reported patient showed the occlusive lesion of the distal of left circumflex (LCX). After spine balloon expansion, there is still about 80% stenosis in the distal of LCX. After giving nitroglycerin, there is no significant change. It shows that the narrow may be the result of coronary atherosclerosis. According to the activity index of SLE, it does not consider disease activity temporarily. It indicates that secondary AMI may be related to coronary atherosclerosis, leading to obstructive coronary lesions (Figure 2).
Figure 2: (A) This is the angiography of the right coronary artery in the head position. The result suggests that the right coronary artery was small. And this stenosis was 75%.
(B) This is the angiography of the left anterior descending artery in the right oblique. The result showed the middle of left anterior descending was 75% stenosis.
(C) This is the angiography of the left circumflex artery at the liver. It demonstrates that the left circumflex had 95% stenosis and the distal was occlusion. And the TIMI flow grade was zero.
(D) After spine balloon expansion, there was still about 80% stenosis in the distal of LCX. After giving nitroglycerin, there was no significant change.
(E) Eventually, we implanted two stents in the left circumflex sequentially.
From the diagnosis and treatment of the patient, that primary AMI may be on the basis of SLE triggering coronary inflammation of non-obstructive myocardial infarction which was caused by coronary artery spasm. Contrasting the ECG of primary AMI, the fixed leads in ECG of this secondary AMI are the pathologic Q wave which have no obvious change. ST-segment elevation is not obvious, but the new appearance is obvious ischemic J wave. Ischemic J wave is presented in recent years. It is a kind of super urgent issue of ECG findings about myocardial ischemia. This ECG is not stable, easily causing ventricular fibrillation and sudden death. Once receiving such patients in the clinical practice, even if the symptoms are not typical and myocardial enzymes increasing is not up to standard, we should attach great importance to the history of inquiry, the dynamic monitoring of myocardial enzymes and the ECG recognition. The early identification and intervention are necessary.
Although no evidence of SLE activity, the patients of AMI with SLE should carry out the reperfusion therapy as soon as possible. At the same time, it is necessary that full anti-thrombotic and anticoagulation are preventing the occurrence of cardiovascular events and delaying the development of coronary atherosclerosis.
The SLE patients with coronary stenting on the basis of anticoagulant therapy plus steroid drugs have not been reported at home and abroad. But how to anticoagulant therapy on the basis of anti-inflammatory treatment has no experience, it is recommended for patients with SLE and other connective tissue disease, early postoperative anticoagulation therapy on the basis of strengthening anti-inflammatory treatment.
Conclusion
Before the primary acute myocardial infarction, the patient had a history of a large dose of hormonal application. Then he took the treatment with hydroxychloroquine. Eventually, acute myocardial infarction was unexplained for the second time.
References
- Estes D, Christian C L (1971) The natural history of systemic lupus erythematosus by prospective analysis. J Medicine 50: 85-95.
- (2010) Guide to diagnosis and treatment of systemic lupus erythematosus (SLE) Chinese J Rheum 342-346.
- Junbo Ge, yongjian Xu (2013) Internal medicine. Eight edition, People's medical publishing house.
- Nikpour M, Urowitz MB, Gladman DD (2005) Premature atherosclerosis in systemic lupus erythematosus. Rheum Dis Clin North Am 31: 329-354.
- Manger K, Kusus M, Forster C, et al. (2003) Factors associated with coronary artery calcification in young female patients with SLE. Ann Rheum Dis 62: 846-850.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi