Research Article, J Womens Health Issues Care Vol: 7 Issue: 4
Single Incision Vaginal Tape for Lateral Detachment Repair: A Pilot Study and Description of the Method
Christian Goepel1, Miklos Szakacs1, Nelli Farkas2 and Balint Farkas1*
1Vivantes Humboldt Clinic, Pelvic Floor and Incontinence Centre, Berlin, Germany
2University of Pecs, Institute of Bioanalysis, Pecs, Hungary
*Corresponding Author : Balint Farkas, MD, Med. habil.
Vivantes Humboldt Clinic, Pelvic Floor and Incontinence Centre, 2 Am Nordgraben Str. 13509, Berlin, Germany
Tel: +49-(030)-120-121-873
Fax: +49-(030) 130-121-082
E-mail: dr.balint.farkas@gmail.com
Received: June 11, 2018 Accepted: July 06, 2018 Published: July 13, 2018
Citation: Goepel C, Szakacs M, Farkas N, Farkas B (2018) Single Incision Vaginal Tape for Lateral Detachment Repair: A Pilot Study and Description of the Method. J Womens Health, Issues Care 7:4. doi: 10.4172/2325-9795.1000317
Abstract
niques are aimed to stabilize the lost integrity at DeLancey Level II, none of them seemed to be optimal. Despite vaginal surgical approaches utilizing synthetic meshes has been well established, and widely debated, our aim was to establish an optimal surgical procedure to decrease the size of the implanted vaginal grafts. Methods: In a prospective preliminary study, 43 patients with lateral cystoceles were enrolled, and have been implanted a partially absorbable polypropylene/polyglycholic acid vaginal tape. The two endpoints of the tapes were administered above the ATFP, providing lateral support. In 53% of the cases (23/43) the patients also received a TVT, due to co-existing SUI. Follow up examination were carried out six month after the operation. Results: We observed significant shift in the Aa points (-0.86 cm ± 0.56 SD to -2.95 cm ± 0.30 SD) and in the Ba points (-0.42 cm ± 0.59 SD to -2.65 cm ± 1.04 SD) pre and postoperatively. Those patients who had dual tape implanted 95% (22/23) were found to continent. During the six month follow up period no mesh extrusion, no dyspareunia and no recurrence were noted. Conclusions: The implantation of a vaginal tape is a relatively easily and quickly executed surgical technique, which is able to bypass laparoscopic approaches. The method can be combined with simultaneous TVT implantation in SUI patients. Although further studies with more participants, are required to assess the effectiveness of the approach.
Keywords: Pelvic organ prolapse; Lateral cystocele; Surgical treatment; Pelvic reconstructive surgery
Introduction
Pelvic organ prolapse (POP) is a relatively common disorder, which is described as a loss of anatomical support of the pelvic organs that lead to impairment of normal function and diminished quality of life [1]. It may occur in up to 50% of parous women [2], and only in the United States alone, the lifetime risk of undergoing surgery for symptomatic POP or stress urinary incontinence (SUI) has newly been reported to be 20% [3], with a 30% risk of reoperation within a period of 4 years [4].
Anterior and middle zone defects are responsible for 80% of POP procedures [5]. Middle zone defects include apical, median (pulsion), and lateral (traction) cystoceles. The pathophysiology of a lateral cystocele is multifactorial. Obstetric related injuries, menopause, genetic factors, chronically increased intraabdominal pressure, pelvic floor trauma and spina bifida are proved to be key risk factors of the disease. It is explained with the loss of midvaginal lateral attachment, which is normally achieved by the anchorage of the vaginal wall to arcus tendineus fascia (ATFP) and levator ani muscle fascia [6]. The condition can be uni-or bilateral in appearance, and often (80-90%) combined with median cystocele or stress urinary incontinence (SUI) [7]. The typical symptoms of the disease are the sensation of vaginal bulging or protrusion, feeling of pelvic or vaginal pressure and heaviness in pelvis or vagina, and can be combined with frequency, urgency, weak prolonged urinary stream, hesitency feeling of incomplete emptying, manual reduction of prolapse to start or complete voiding, and the need of position change to start or complete voiding.
The treatment of symptomatic middle zone defects can be conservative or surgical, through pelvic reconstructive surgery. Although, several abdominal, laparoscopic and vaginal surgical techniques are aimed to stabilize the lost integrity at DeLancey Level II, none of them seemed to be optimal. Vaginal surgical approaches utilizing four arm synthetic meshes for middle zone prolapse repair has been established, and debated in the last decade [2,8]. Due to the recent findings about the mesh related complications in the literature, we had to satisfy the need to decrease the size of the implanted vaginal grafts. Our aim was to establish an optimal surgical technique to treat lateral cystoceles, achieved by reinforced lateral middle zone suspension, with the use of partially absorbable polypropylene vaginal tape.
Materials and Methods
Study population and data collection
This study was approved by the Institutional Ethical Review Board. In a prospective cohort study, 43 women suffering from symptomatic POP-Q stage II-III lateral cystocele, who were intended to be treated with vaginal surgery, were included. In 53% of the participants patients (n=23) co-existing SUI has been diagnosed by the demonstration of positive stress test and urodynamic studies. Participants underwent diagnosis, therapy and follow up at the Vivantes Humboldt Clinic’s Pelvic Floor and Incontinence Centre (Berlin, Germany) from January 1st 2017 to September 30th 2017. All patients provided their written informed consent to participate. All patients reported sensation of a bulge in the vagina with symptoms of urinary (urgency, hesitency, frequency, prolonged urinary stream and feeling of incomplete emptying) and sexual dysfunction (dyspareunia, decreased lubrication and decreased sensation, arousal or orgasm). The SUI patients complained about involuntary loss of urine associated with activities increase physical stress and pressure in the abdomen and bladder (laughing, coughing, heavy lifting, and sexual intercourse). Patients with active infections of the pelvis or vagina, such as vaginitis, urinary tract infection or pelvic inflammatory disease, and patients who were noncompliant or unlikely to participate in the follow up (they did not attend their check-ups) were excluded. Baseline demographic data, age, parity, medical history, and BMI were recorded. On the first postoperative day haemoglobin and haematocrit levels were determined. Follow up examinations were carried out 6 months after surgery, which time participants were re-examined by the same investigator in a same way as preoperatively.
Evaluation of POP
All women were examined according to the International Urogynecological Association (IUGA) guidelines, and all terminology currently used refers to the recommendations of the International Continence Society (ICS). The level of altered pelvic anatomy was assessed by using the pelvic organ quantification system (POP-Q) [9]. All examinations were carried out in an outpatient setting, where patients were positioned in standard lithotomy position, physicians were utilizing anterior and posterior vaginal retractors, while patients performed Valsalva manoeuvres, in order to reveal the predominant compartment of prolapse. The POP-Q stage, the level of prolapse in each compartment, the genital hiatus, the vaginal length, and the vaginal introitus size (measured by fingerbreadths) were examined. The paravaginal defects were identified in participants with significant urethral and anterior vaginal wall hypermobility on stress maneuvers during physical examination. On examination with a half speculum directed posteriorly reducing the posterior vaginal wall, those patients have hypermobility of the entire anterior vaginal wall on stress with laxity of support for the anterolateral vaginal wall with preserved rugae vaginales and shallowed paravaginal sulcus. Involuntary loss of urine was assessed by stress test in lithothomy and upright positions, and with the demonstration of urethral funnelling with ultrasound (US). Pelvic floor US also revealed the urethral length, level of prolapse and the pelvic anatomy. Post voiding residual volume was objectively assessed through catheterisation pre-and postoperatively, moreover urine culture was carried out preoperatively.
Description of the surgical methods
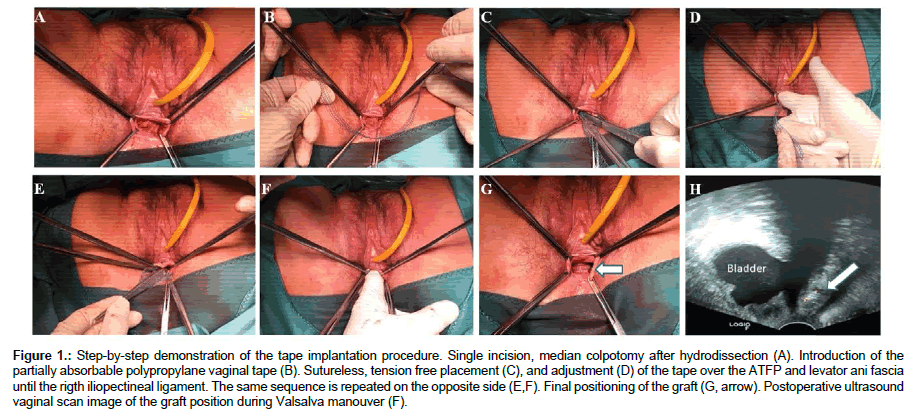
Vaginal tape implantation: The development of the method was based on the description of a nonanchored vaginal mesh by Carey et al. [10]. After infiltrating the anterior vaginal wall with epinephrine containing physiological saline (1 ampulla epinephrine in 500 ml in isotonic Ringer’s lactate solution) a single midline epithelial incision was carried out. The vaginal epithelium was then dissected bilaterally from the underlying pre-vesical tissue in a manner of hydrodissection, fine scissor preparation (push-spread technique), and digital separation until reaching the ATFP. The inner surface of the pubic bone was palpated at the level of the mid-vagina and the lateral dissection was continued through the ATFP and Levator ani muscle fascia for approximately 3 cm until the iliopectineal ligament. In the created tunnel a 2.5 cm wide and 25 cm long cross-shaped piece of partially absorbable polypropylene/polyglycholic acid vaginal tape (SERATEX® A6PA, ref# STA014016, Serag-Wiessner, Germany) was placed without fixing sutures over the pre-vesical tissue, with the endpoint of the tape overlying the previously formed tunnel in each paravaginal space. The mesh extension arms abutted the inner aspect of the pubic bone on each side. The vaginal epithelium was closed with a nonlocking continuous everting mattress suture (Figure 1). After the intervention a routine cystoscopy was performed to exclude potential bladder injury.
Figure 1: Step-by-step demonstration of the tape implantation procedure. Single incision, median colpotomy after hydrodissection (A). Introduction of the partially absorbable polypropylane vaginal tape (B). Sutureless, tension free placement (C), and adjustment (D) of the tape over the ATFP and levator ani fascia until the rigth iliopectineal ligament. The same sequence is repeated on the opposite side (E,F). Final positioning of the graft (G, arrow). Postoperative ultrasound vaginal scan image of the graft position during Valsalva manouver (F).
Tension free vaginal tape implantation: For SUI patients Advantage Fit Blue System® (UPN# M0068502120, Boston Scientific, USA) tension free vaginal tape (TVT) was implanted as described by Ulmsten at al. [12].
Statistical analysis
Statistical analyses were performed by using IBM SPSS Statistic 20 (IBM Corporation, Armonk, NY, USA) at the University of Pecs, Institute of Bioanalysis. Continuous measurements are summarized and presented as averages and standard deviations (SD), categorical data is presented as observed or as percentages. For the independence analysis between the categorical variables Mann-Whitney and Independent Student’s t-test performed. To determine whether there is a significant difference between the expected frequencies and the observed frequencies in one or more categories Chi-square test was used. Statistical significance was set at p<0.05.
Results
Demographic data
The average age was 59 years ± 13 SD (min: 41, max: 84), and the mean parity was 2.38 ± 1.96 SD per patient (min: 0, max: 12) (Table 1). The study population had average weight of 75.77 kg and height of 1.64 m, resulting in a mean BMI of 28.32 ± 5.56 kg/m2 (min: 21.01, max: 46.10). A total of 30 patients (69%) had neither reconstructive pelvic surgery nor hysterectomy in their history (Table 1). All together 11 women (25%) underwent previous hysterectomy, 11% (5/43) had anterior, and 9% (4/43) had prior posterior colporraphy due prolapse indication in their history. In 53% of the cases (23/43) the patients also received a transvaginal tape (TVT), due to co-existing SUI.
| Variables | Tape only (n=20) | Tape + TVT† (n=23) | p value |
|---|---|---|---|
| Age (years ± SD) | 64.10 ± 13.55 | 55.57 ± 11.87 | 0.033 |
| Parity (n ± SD) | 2.63 ± 2.75 | 2.17 ± 0.14 | 0.723 |
| Height (m) | 1.64 ± 0.07 | 1.64 ± 0.05 | 0.953 |
| Weight (kg) | 71.75 ± 13.45 | 79.26 ± 16.52 | 0.113 |
| BMI§ (kg/m2 ± SD) | 26.83 ± 4.69 | 29.61 ± 6.03 | 0.103 |
| Prior POP* surgeries | |||
| Hysterectomy (n) | 8 | 3 | 0.043 |
| Anterior colporraphy (n) | 3 | 2 | 0.650 |
| Posterior colporraphy (n) | 4 | 0 | 0.039 |
| TVT (n) | 1 | 1 | 1.000 |
Table 1: Demographic summary of the participated patients at the Pelvic Floor and Incontinence Centre in Berlin. The P values are representing the results of Mann- Whitney test analysis between “tape only” and “tape+TVT” groups.
Evolution of POP-Q scores after tape implantation surgeries
We experienced major improvement in the lateral cystocele after surgery in all patients. We managed to observe significant shift in the Aa points (-0.86 cm ± 0.56 SD to -2.95 cm ± 0.30 SD) and in the Ap points (-1.14 cm ± 1.46 SD to -2.37 cm ± 0.76 SD). Moreover a major significant development was also observed in the Ba point (-0.42 cm ± 0.59 SD to -2.65 cm ± 1.04 SD) and in the Bp point (-0.58 cm ± 1.78 SD to -2.16 cm ± 0.90 SD) positions. In the further POP-Q variables (C, D points, GH, PB and TVL) no significant differences were calculated before and after the surgery (Table 2).
| POP-Q variable | Preoperatively (cm ± SD) | Postoperatively (cm ± SD) | p value |
|---|---|---|---|
| “Aa” point | -0.86 ± 0.56 | -2.95 ± 0.30 | **<0.001 |
| “Ba” point | -0.42 ± 0.59 | -2.65 ± 1.04 | **<0.001 |
| “Ap” point | -1.14 ± 1.46 | -2.37 ± 0.76 | **<0.001 |
| “Bp” point | -058 ± 1.78 | -2.16 ± 090 | **<0.001 |
| “C” point | -5.44 ± 2.85 | -5.93 ± 2.47 | 0.030 |
| “D” point | -6.18 ± 3.51 | -6.76 ± 3.28 | 0.017 |
| “GH”* | 3.74 ± 0.58 | 3.53 ± 0.55 | 0.030 |
| “PB”§ | 3.58 ± 0.78 | 3.61 ± 0.82 | 0.356 |
| “TVL”† | 8.35 ± 0.92 | 8.37 ± 0.93 | 0.317 |
Table 2: Improvement of POP-Q score variables before and after the intervention.
Subjective and objective outcomes
Out of those individuals who had dual tape implanted (vaginal tape+TVT) 95% (22/23) of them were found to be continent 6 months after the operation. All patients were subjectively satisfied after the intervention. No major blood loss was observed during the interventions (Haemoglobin pre.op.: 136.0 g/L ± 1.00 SD, post. op.: 127.7 g/L ± 1.26 SD, p=0.546; Haematocrit pre.op.: 0.40 L/L ± 0.09 SD, post.op.: 0.36 L/L ± 0.08 SD, p=0.773) and no patient needed to receive blood transfusion. The mean close-to-cut time was 56.02 min ± 20.99 SD. The mean hospital stay was 2 days. No intraoperative, neither minor, nor major 30 days complications were observed. During the six months follow up period no mesh extrusion, no dyspareunia and no prolapse recurrence (defined as prolapse extending halfway to the hymen with straining; POP-Q points Aa, Ap, ≥ -1.5, or repeat treatment for prolapse with either pessary or surgery) were noted.
Discussion
To our knowledge, this is the first study which demonstrates a surgical technique utilizing a partially absorbable polypropylene/ polyglycholic acid vaginal tape self-restraining vaginal tape, in order to successfully treat lateral middle zone detachment. In the current study, 43 women with symptomatic stage II-III traction cystoceles underwent single incision vaginal tape implantation, and after 6 month all of them were referred themselves to be symptomless.
The justification of synthetic mesh materials in vaginal POP surgeries are widely debated since the mounting evidence reported in the literature about mesh related complications [12], and the US Food and Drug Administration (FDA) safety warning regarding transvaginal mesh complications [13]. Despite the obvious and unquestionable dilemma of the use of transvaginal mesh in POP, and especially anterior vaginal wall surgeries, our study group is not intending to discard the vaginal route from the operative inventory, more likely we are looking for alternative surgical approaches and try to use innovative grafts to decrease the volume of implanted allograft material. Although our results seem to be promising, we could review a relatively small sample during a short follow-up period.
One of the contradictory views against synthetic allograft implantation into the anterior vaginal wall is the high risk of mesh exposure, of which a woman undergoing a native tissue repair has no risk to develop [14]. Although in recent studies this complication is reported to range between 7.7%-10.1% [15-17], in our current study we found no tape exposure during the follow up period. Another common reason against mesh is the rising number of de novo SUI after mesh repair of the middle zone defects, with an incidence between 8.6%-13.3% [14-16]. We found a remarkable 96% cure rate in the 47 per cent of patients, who had pre-existing SUI and lateral cystocele when received dual tape (vaginal tape+TVT), and we experienced no de novo stress appearance, confirmed by negative cough stress tests, in the study group. Further issue is that vaginal mesh surgeries are resulting increased rate of intraoperative bladder injuries. Despite some studies are suggesting that this is a real threat, with intensive hydrodissection and careful preparation we are able to minimize the occurrence of such complications. During our 43 interventions, including 22/23 simultaneously TVT implantation, we observed no bladder injury, confirmed by routine cystoscopy. Further misbelief is that anterior vaginal wall mesh operations are correlated with increased blood loss compared with native tissue repair, or laparoscopic approaches. Although in a metaanalysis including 631 patients with substantial heterogeneity, who underwent anterior vaginal wall mesh implantation great blood loss was found, with a mean difference of 45.98 ml (CI=9.72-82.25) [18], we managed to demonstrate no significant alteration in haemoglobin and haematocrit levels.
On the other hand there are several undoubted advantages of synthetic allograft use in the operative management of middle zone defects compared to other approaches. First of all the high objective and subjective cure rates, ranging around 90% [19-21], are making it a considerable alternative to other operative techniques. We were able to achieve similar results with the use of an optimally placed vaginal tape (Table 2). The above described method, and even vaginal surgeries in general, are considered to be real minimal invasive techniques, with a preferred cosmetic result. While a recent study failed to report significant differences in cost between laparoscopic sacrohysteropexy and vaginal mesh correction for the treatment of POP (mean 5985.7 €, CI 95% : 5613.14 versus mean 6534.31€, CI 95%: 6290.36), we found an average cost of 3783€ / mean 2 days hospital stay per single tape implantation, and 4175€ / mean 2 days for dual tape procedure. Despite no cost effectiveness analysis was carried out the single incision vaginal tape implantation is likely to be a cost sparring surgical approach to treat lateral cystoceles.
The limitation of our study is the relative low number of participants, and the relative short duration of follow up, therefore further studies with more participants, and furthermore postoperative magnetic resolution scan verifications of the mesh position are required to assess the effectiveness of the approach.
The strongpoint of our study is the demonstration of new and innovative operative technique in order to overcome middle zone anterior vaginal wall defects. The implantation of a vaginal tape in case of lateral cystoceles comes with short operation time, therefore it is a relatively easily and quickly executed surgical technique, which is might be able to bypass abdominal or laparoscopic approaches. With the use of less graft material, the mesh related complications are considered to appear minimally. The method can be easily combined with simultaneous TVT implantation in SUI patients, with respectable results.
Acknowledgements
We thank the medical assistants and station and OP nurses working at the Vivantes Humboldt Clinic, Berlin, Germany, for their help and dedicated contributions towards the study and our patients. We are also grateful for Mrs. Veronika Goepel, for her help in the data collection and archiving process.
Conflict of Interest
The corresponding author has multiple affiliations and has received financial support from the Hungarian Academy of Sciences (MTA), Budapest, Hungary. The remaining authors report no conflicts of interest with the present study.
References
- Mouritsen L (2005) Classification and evaluation of prolapse. Best Pract Res Clin Obstet Gynaecol 19: 895-911.
- Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4: CD004014.
- Boyles SH, Weber AM, Meyn L (2003) Procedures for pelvic organ prolapse and urinary incontinence in the United States, 1979-1997. Am J Obstet Gynecol 188: 108-115.
- Brincat CA, Larson KA, Fenner DE (2010) Anterior vaginal wall prolapse: assessment and treatment. Clin Obstet Gynecol 53: 51-58.
- Petros P (2011) The integral system. Cent European J Urol 64: 110-119.
- Delancey JO (2002) Fascial and muscular abnormalities in women with urethral hypermobility and anterior vaginal wall prolapse. Am J Obstet Gynecol 187: 93-98.
- Lensen EJ, Withagen MI, Kluivers KB, Milani AL, Vierhout ME (2013) Surgical treatment of pelvic organ prolapse: a historical review with emphasis on the anterior compartment. Int Urogynecol J 24: 1593-1602.
- Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, et al. (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J Obstet Gynecol 175: 10-17.
- Carey M, Higgs P, Goh J, Lim J, Leong A, et al. (2009) Vaginal repair with mesh versus colporrhaphy for prolapse: a randomised controlled trial. BJOG 116: 1380-1386.
- Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7: 81-86.
- Maher C (2013) Anterior vaginal compartment surgery. Int Urogynecol J 24:1791-1802.
- Food and Drug Administration Safety Communication (2011) Safety communications-UPDATE on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse.
- Kontogiannis S, Goulimi E, Giannitsas K (2017) Reasons for and against use of non-absorbable, synthetic mesh during pelvic organ prolapse repair, according to the prolapsed compartment. Adv Ther 33: 2139-2149
- Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, et al. (2016) Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev 2: CD012079.
- Rudnicki M, Laurikainen E, Pogosean R, Kinne I, Jakobsson U, et al. (2016) A 3-year follow-up after anterior colporrhaphy compared with collagen-coated transvaginal mesh for anterior vaginal wall prolapse: a randomised controlled trial. BJOG 123: 136-142.
- Dias MM, Castro AR, Bortolini MA, Delroy CA, Martins PC, et al. (2016) Two-years results of native tissue versus vaginal mesh repair in the treatment of anterior prolapse according to different success criteria: A randomized controlled trial. Neurourol Urodyn 35: 509-514.
- Juliato CR, Santos LC, Haddad JM, Castro RA, Lima M, et al. (2016) Mesh surgery for anterior vaginal wall prolapse: a meta-analysis. Rev Bras Ginecol Obstet 38: 356-364.
- Nguyen J, Burchette RJ (2008) Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol 111: 891-898.
- Amrute KV, Eisenberg ER, Rastinehad AR, Kushner L, Badlani GH (2007) Analysis of outcomes of single polypropylene mesh in total pelvic floor reconstruction. Neurourol Urodyn 26: 53-58.
- Jo H, Kim JW, Park NH, Kang SB, Lee HP, et al. (2007) Efficacy and outcome of anterior vaginal wall repair using polypropylene mesh(Gynemesh). J Obstet Gynaecol Res 33: 700–704.
- Cervigni M, Natale F, La Penna C, Panei M, Mako A (2008) Transvaginal cystocele repair with polypropylene mesh using a tension-free technique. Int Urogynecol J Pelvic Floor Dysfunct 19: 489-496.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi