Case Report, J Womens Health Issues Care Vol: 7 Issue: 2
Successful Treatment of Robert’s Uterus by Two Different Ways: Laparotomy or Hysteroscopy: Case Report and Literature Review
Yi Wang*, Qing-Shan Deng, Xiu-Hong Peng and Li-Qin Zeng
Department of Gynaecology, Guangdong Women and Children Hospital, Guangzhou, 510010, China
*Corresponding Author : Yi Wang
Department of Gynaecology, Guangdong Women and Children Hospital, Guangzhou, 510010, China
Tel: +86 15915778379
E-mail: wangyi000924@163.com
Received: February 24, 2018 Accepted: March 05, 2018 Published: March 12, 2018
Citation: Wang Y, Deng Q, Peng X, Zeng L (2018) Successful Treatment of Robert’s Uterus by Two Different Ways: Laparotomy or Hysteroscopy: Case Report and Literature Review. J Womens Health, Issues Care 7:2. doi: 10.4172/2325-9795.1000304
Abstract
Robert’s uterus is unique malformation described as a septate uterus with non-communicating hemicavity; i.e. a blind uterine horn usually with unilateral hematometra, contralateral unicornuate shaped uterine cavity and normal external shape of the uterine fundus. Pelvic pain intensified near the menses in young women is the main symptom and recurrent pregnancy loss and infertility are the main questions when they grow up. In this study, we described two cases of Robert’s uterus: one was Excised of the septum on laparotomy and then successfully became pregnant and gave birth, the other was treated with hysteroscopy and 1 month later, another hysteroscopy showed the uterine cavity shape was closer to the normal. And we also summarized the diagnosis and treatment from the current reports.
Keywords: Müllerian anomaly; Robert’s uterus; Septate uterus
Case Report
Case one
A 19-year-old woman, G1P0, was admitted to our Department with suspected uterine malformation due to Mullerian duct anomaly on 21 June 2013. 3 months ago, ultrasound indicated double uteri with left-side rudimentary horn, and right-side unicornuate uterus which had a dead early Embryo inside. She had a past history of dysmenorrhoea relieved only with analgesics since menarche at 15 years of age. Her menstrual cycles were regular at a 30-day interval for 4 days.
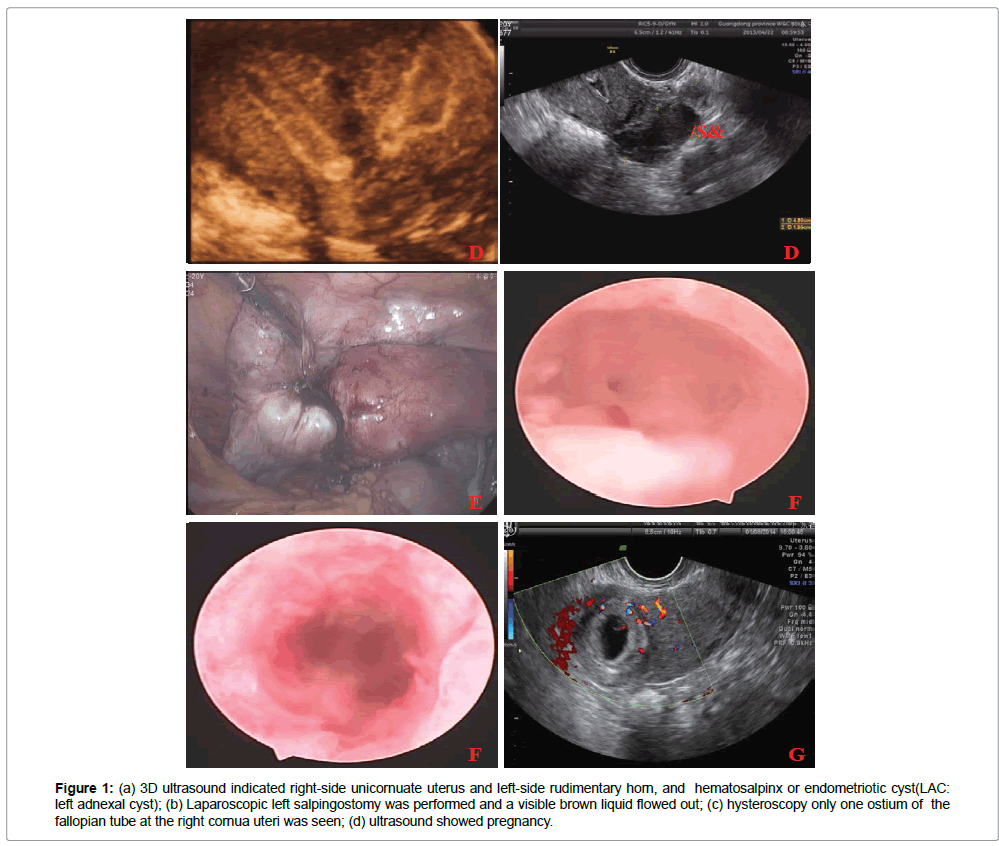
Gynecologic examination showed anatomically normal vagina and cervix. Three-dimensional ultrasound indicated double uteri with right-side unicornuate uterus and left-side rudimentary horn (53 mm×35 mm×37 mm) and haematometra in the left uterine horn (23 mm×6 mm) and left uterine intramural cysts (5 mm×5 mm). And a distended left fallopian tube (48 mm×19 mm) with echogenic fluid was seen, suggestive of hematosalpinx or endometriotic cyst. The right annexa was normal (Figure 1a). Urinary tract ultrasound showed the left renal agenesis. A provisional diagnosis of unicornuate uterus with noncommunicating functional rudimentary horn with haematometra and left hematosalpinx or endometriotic cyst was made.
Figure 1: (a) 3D ultrasound indicated right-side unicornuate uterus and left-side rudimentary horn, and hematosalpinx or endometriotic cyst(LAC: left adnexal cyst); (b) Laparoscopic left salpingostomy was performed and a visible brown liquid flowed out; (c) hysteroscopy only one ostium of the fallopian tube at the right cornua uteri was seen; (d) ultrasound showed pregnancy.
Then laparoscopy and hysteroscopy were done. On laparoscopy the following was noted: the basilar part of the uterus was wide and slightly hollow and a double corpus uteri was suspected; the left side of the uterine body was normal, and the right side was dilated. We observed extensive adhesions along the peritoneum, the left fallopian tube and intestinal wall, and tortuous and thickened adhesions of the left fallopian tube and the ovaries. We also observed the left fallopian tube fimbria was atresic and greatly dilated, the size of left tube increased to 5 cm×3 cm (Figure 1b). Laparoscopic left salpingectomy was performed and a visible brown liquid flowed out. Using a hysteroscopy, we observed that the uterine cavity had a small-diameter narrow channel. Only one ostium of the fallopian tube at the right cornua uteri was seen, and a uterine septum (Figure 1c). Robert’s uterus was confirmed.
Hysterotomy incision was performed on the left uterine swelling surface and a visible brown viscous liquid flowing out of the left hemicavity. A uterine septum with the size of 1.5×2 cm was found between the two uterine cavities which made the left horn noncommunicating. We resected the septum,and the endometrium was identified. The myometrial tissue was repaired in two levels using the continuous locked suture technique. Foley’s catheter inflated with 7mL normal saline was placed in the uterine cavity for 72 h to facilitate drainage and prevent adhesion. She recovered well after the operation without any complication.
The woman returned to our hospital 6 months later due to missed menstruation. The transvaginal ultrasound showed a 1.7 cm gestational sac indicative of a 6-week embryo (Figure 1d). She became pregnant 6 months after the surgery and delivered a healthy baby by caesarean section in the 38th week of gestation.
Case two
A 22-year-old woman, G3P0A3, was admitted to our Department with suspected uterine malformation on 1 July 2015. Her menstrual cycles were regular at a 30-34 days interval for 4 days and had no symptoms related to dysmenorrhoea, endometriosis or pelvic pain. She had a disturbing history of adverse pregnancy outcomes: two spontaneous abortions and one missed abortion. When she last miscarriage, uterine anomaly was suspected on ultrasonographic examination.
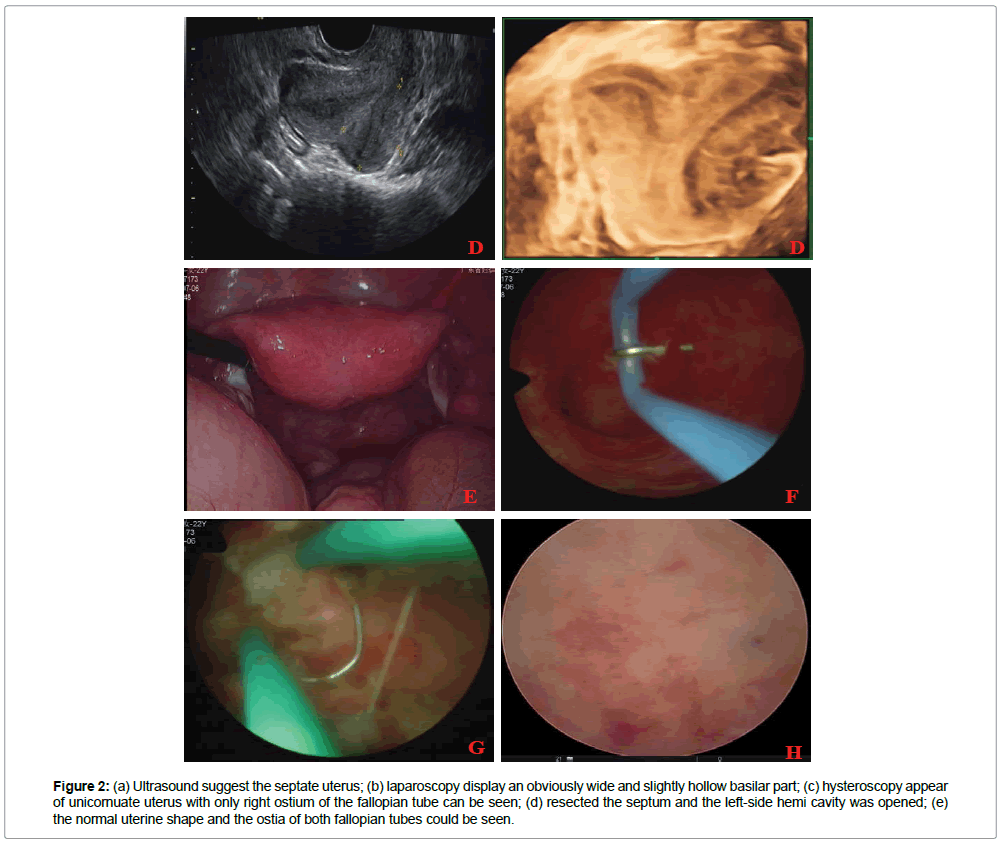
Gynecologic examination showed anatomically normal vagina and cervix. The result of Chromosome examinat was 46, XX, 21pss, and her husband’s result of Chromosome examinant of was normal. Three-dimensional ultrasound display a septate uterus with septate cervix: a fundal contour has a small indentation with internal isoechoic septum. The septum divides the endometrial cavity toward the level of the internal os. The endometrium inside both cavity was normally identified.The both annexa were normal (Figure 2a). Urinary tract ultrasound showed that the kidneys, the bladder and the ureters were normal. With these findings, a diagnosis of septate uterus was made.
Figure 2: (a) Ultrasound suggest the septate uterus; (b) laparoscopy display an obviously wide and slightly hollow basilar part; (c) hysteroscopy appear of unicornuate uterus with only right ostium of the fallopian tube can be seen; (d) resected the septum and the left-side hemi cavity was opened; (e) the normal uterine shape and the ostia of both fallopian tubes could be seen.
On laparoscopy we visualized a uterus with a obviously wide and slightly hollow basilar part. The both fallopian tubes and ovaries were normal (Figure 2b). At the same time, a diagnostic hysteroscopy was performed. On hysteroscopy, the following was noted: the uterine cavity had a small-diameter narrow channel. Only one ostium of the fallopian tube at the right was vaguely seen, the left side of cornua uteri cannot be exposed and completely (Figure 2c). An asymmetric fibrous septum extended from the central fundus of uterus to the upper two-third of the uterine wall on the left side, which was consistent with the diagnosis of Robert’s uterus.
We opened the septum with a needle electrode under ultrasonic monitoring starting at the weakest location in the right uterine cavity. we resected the septum to 3 cm in length until the left-side hemi cavity (3×3×2 cm)was opened, and then the endometrial dysplasia in the left uterine cavity was identified (Figure 2d). After the intervention, both corneas of the opened inverted triangle-shaped cavity could be seen,but the ostia of the right and left fallopian tubes could not be seen clearly. Foley’s catheter inflated with 7mL normal saline was placed in the uterine cavity for 72 h to facilitate drainage and prevent adhesion.
For clinical evaluations, another hysteroscopy was performed 1 month after the surgery, the two hemi-cavities were connected widely, and the uterine cavity shape was closer to the normal inverted triangle-shape. And both ostia of the right and left fallopian tubes could be seen (Figure 2e). The patient reported that the menstruation ceased to be painful but was still not pregnant.
Discussion
The septate uterus (class V, American Society for Reproductive Medicine Classification ASRM) results from a lack of septum resorption after successful Mullerian fusion and is the most commonly diagnosed Mullerian duct anomaly, occurring in about 55% of anomalies. But Robert’s uterus is a rare type of Mullerian duct anomalies and a variant of septate uterus [1]. It was first described by Robert in 1970 [2] and with only a few cases reported so far. However, the ESHREâ€ÂESGE classification describes this anomaly as complete septate uterus with partial cervical aplasia (ClassU2bC3V0), without explanation on which grounds ‘unilateral cervical aplasia’ is diagnosed [3]. Robert’s uterus is characterized by uterine septum dividing the endometrial cavity asymmetrically with non communicating hemi uterus due to obstruction by the septum. As a result there is obstruction to menstrual flow in one cavity, resulting in haematometra, haematosalpinx and sometimes endometriosis. Haematometra and dysmenorrhoea can be associated with a progressive increase in the diameter of the distended blind cavity. Theoretically, the absence of a communication with the ipsilateral fallopian tube would aggravate symptoms. Contrary to the typical presentation, our two cases did not complain of seriously previous dysmenorrhoea, especially case 2.They were suspected müllerian duct anomalies for the histroy of disturbing adverse pregnancy outcomes.
Robert’s uterus is difficult to diagnose preoperatively and is often misdiagnosed. Diagnostic modalities may include ultrasound, hysterosalpingography (HSG) and magnetic resonance imaging. Ultrasound sensitivity for diagnosis of Robert’s uterus is not high and frequently misdiagnosed as unicornuate uterus with noncommunicating rudimentary horn, as our case one. While HSG is usually suspected unicornuate uteri, with a typical fusiform or ‘‘banana’’ shape on imaging and visualization of only 1 fallopian tube. Unfortunately, septate uteri cannot be fully differentiated with HSG given the absence of external fundal imaging.MRI is the best modality to demonstrate the uterine septum, normal external fundal contour, haematometra and haematosalpinx, but is unfortunately expensive. In cases of Robert’s uterus the coronal T2W images of MRI are ideal for demonstrating the uterine septum dividing the endometrial cavity asymmetrically along with the blind ending cavity and haematometra. T1W images show the haematometra and haematosalpinx as bright fluid in the endometrial cavity and dilated fallopian tube [4].
3D ultrasound is as good as MRI in providing a correct diagnosis. Although both methods require an experienced operator and interpretation by an experienced practitioner, hysteroscopy in combination with laparoscopy is the gold standard for the diagnosis of Robert’s uterus. The features include discordance due to laparoscopic appearance of normal uterine shape (normal external fundal contour or slightly hollow/protrusion, with or without hematometra and hematosalpinx) and hysterographic appearance of unicornuate uterus with only one ostium of the fallopian tube can be seen.
In the differential diagnosis, unicornuate uterus with noncommunicating rudimentary horn should be considered. Which usually present after menarche with progressive abdominal pain and dysmenorrhoea due to haematometra, haematosalpinx and endometriosis. Rudimentary horn is 26% and diagnosis before symptom presentation is made in only 14% cases [5]. The surgery to excising the rudimentary horn and ipsilateral fallopian tube is the main treatment method. The main point to differentiate accurately Robert’s uterus from rudimentary uterine horn is laparoscopic appearance: the former usually has normal uterine shape (a fundal contour that is convex, flat, or has a small indentation (<1 cm) ), but the latter has the fundal cleft be greater than 1 cm like bicornuate uterus [6].
The only effective treatment of Robert’s uterus is surgical operation. Robert’s uteruswere managed via laparotomy and total horn resection or endometrectomy of blinded cavity, abdominal metroplasty, or by combining hysteroscopy/laparoscopy. Irreversible surgeries (horn resection/endometrectomy of blinded cavity) with loss of the potential were performed to improve uterine cavity shape and volume for this condition. A complete endometrectomy of the blind hemi-cavity is suitable for the cases. There is no communication between the blind cavity and the ipsilateral fallopian tube, it can be effective in preventing recurrence of hematometra. Vural, et al. [7] performed hysterotomy incision and endometrectomy for a Robert’s uterus. And the patient had a successful pregnant and delivered a healthy baby by cesarean section in the 39th week of gestation. Capito, et al. [8] performed a surgery of an endometrectomy of the blind cavity for a 15-year-old patient complaining of recurrent abdominal cramps.
Hysterotomy and ipsilateral tubal ligation: In 2003, Singhal [9] reported a rare case that a women with 26 weeks gestation in asymmetric blind hemi cavity of Robert’s uterus, hysterotomy followed by extraction of stillborn fetus of 500g was done, and ipsilateral tubal ligation were performed successfully. This case also suggested possible transfer of the sperm between fimbria across the pouch of Douglas.
Excision of the septum with unification of the endometrial cavity on laparotomy or hysteroscopy. Hysteroscopy and laparoscopy combined with ultrasound may be a better method for the diagnosis and treatment of Robert’s uterus. Li et al. [10] performed a septum resection with hysteroscopy under ultrasonic surveillance. And then the patient successfully became pregnant and gave birth. A. Ludwin, et al. [11] first reported treatment of Robert’s uterus used 3D sonohysterography without laparoscopy or laparotomy. The 3D sonohysterography performed a hysteroscopic metroplasty guided by transrectal ultrasound, avoiding laparotomy/laparoscopy. The treatment result was satisfactory: the menstruation ceased to be painful and a normalized uterine cavity of 3.6 cm3 from a communicating hemi cavity of 0.3 cm3 after two hysteroscopic procedures.
Conclusion
Robert’s uterus as a rare type of Mullerian duct anomalies was illustrated and discussed in the paper. Our paper not only describes of two rare cases but also highlight the diagnosis and treatment process of Robert’s uterus. Its diagnosis remains a challenge to the clinicians, and hysteroscopy in combination with laparoscopy is still the gold standard for the diagnosis of Robert’s uterus..Ultrasound combined with hysteroscopy is considered a practical and safe choice for asymmetric septal ablation therapy for Robert’s uterus. By using laparoscopy for monitoring purposes, additional information is obtained for guiding the surgery.
References
- Ludwin A, Ludwin I (2015) Comparison of the ESHREâ€ÂESGE and ASRM classifications of Mullerian duct anomalies in everyday practice. Hum Reprod 30: 569â€Â580.
- Robert H (1970) Asymmetrical bifidities with unilateral menstrual retention. Chirurgie 96: 796-799.
- Sardo AS, Campo R, Gordts S, Spinelli M, Cosimato C, et al. (2015) The comprehensiveness of the ESHRE/ESGE classification of female genital tract congenital anomalies: a systematic review of cases not classified by the AFS system. Hum Reprod 30: 1046â€Â1058.
- Maddukuri SB, Karegowda LH, Prakashini K, Kantipudi S (2014) Robert's uterus: a rare congenital müllerian duct anomaly causing haematometra. BMJ Case Rep.
- Jayasinghe Y, Rane A, Stalewski H, Grover S (2005) The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol 105: 1456-1467.
- Berger A, Batzer F, Lev-Toaff A, Berry-Roberts C (2014) Diagnostic imaging modalities for müllerian anomalies: the case for a new gold standard. J Minim Invasive Gynecol 21: 335-345.
- Vural M, Yildiz S, Cece H, Camuzcuoglu H (2011) Favourable pregnancy outcome after endometrectomy for a Robert’s uterus. J Obstet Gynaecol 31: 668-669.
- Capito C, Sarnacki S (2009) Menstrual retention in a Robert's uterus. J Pediatr Adolesc Gynecol 22: e104â€Âe106.
- Singhal S, Agarwal U, Sharma D, Sirohiwal D (2003) Pregnancy in asymmetric blind hemi cavity of Robert's uterus--a previously unreported phenomenon. Eur J Obstet Gynecol Reprod Biol 107: 93-95.
- Li J, Yu W, Wang M, Feng LM (2015) Hysteroscopic treatment of Robert's uterus with laparoscopy. J Obstet Gynaecol Res 41: 1491-1494.
- Ludwin A, Ludwin I, Martins WP (2016) Robert’s septate uterus: modern imaging techniques and ultrasound-guided hysteroscopic treatment without laparoscopy/laparotomy. Ultrasound Obstet Gynecol.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi