Review Article, J Obes Ther Vol: 1 Issue: 2
The Effect of Vitamin D Supplementation on the Treatment of Overweight and Obesity: A Systematic Review of Randomized Controlled Trials
Stavri Chrysostomou1* and Evgenia Saranti2
1Department of Life Sciences, European University Cyprus, Cyprus
2Department of Health Sciences, European University Cyprus, Cyprus
*Corresponding Author : Stavri Chrysostomou
Lecturer, Department of Life Sciences, School of Science, European University Cyprus, 6, Diogenis Str., Engomi, P.O. Box: 22006, 1516 Nicosia-Cyprus
Tel: 22713293
E-mail: s.chrysostomou@euc.ac.cy
Received: September 22, 2017 Accepted: October 12, 2017 Published: October 19, 2017
Citation: Chrysostomou S, Saranti E (2017) The Effect of Vitamin D Supplementation on the Treatment of Overweight and Obesity: A Systematic Review of Randomized Controlled Trials. J Obes Ther 1:2.
Abstract
Numerous studies indicate that obese individuals have lower levels of vitamin D than humans with normal weight. Moreover, some in vitro studies demonstrated the role of vitamin D in weight reduction. However, both, obesity and vitamin D deficiency are major problems afflicting public health. The main purpose of this systematic review was to investigate the effect of vitamin D supplementation in decreasing the excessive body weight in overweight and obese patients, as evidenced in randomized controlled trials (RCTs). PubMed and EBSCO host were searched for articles. RCTs including overweight and adult participants supplemented with
vitamin D were eligible for inclusion in the current study. The outcome measures related to the body weight changes were considered (body weight [BW], Body Mass Index [BMI], waist circumference [WC], body fat [BF], muscle mass [MM]). The search strategy and study selection processes were performed according to the “PRISMA” guidelines. Seven studies were deemed as eligible for inclusion in the current study. One study showed that vitamin D treatment had a statistically
significant reduction in BW and WC. Also, three studies showed that BF was significantly reduced in the treatment group compared to the control group. Additionally, one study showed that the MM significantly increased in the treatment group compared to the control group whereas one other study showed that FFM was
significantly increased in the treatment group compared to the control group. The findings of the current analysis are still controversial since it is still difficult to determine which effects are due to vitamin D itself and which are mediated via calcium or other factors. The overall an impression is that vitamin D alone may affect fat mass and body mass distribution when supplement in overweight and obese people.
Keywords: Obesity; Overweight; Randomized control trial; Supplement; Systematic review; Vitamin D
Introduction
Obesity is a growing public health matter associated with the burden of several chronic diseases [1]. Obesity is a major risk factor for non-communicable diseases such as cardiovascular diseases, diabetes, musculoskeletal disorders and some types of cancers [2-7]. According to the World Health Organization [6], obesity rates have been over-doubled since 1980. In 2014, more than 1.9 billion adults were overweight, of whom 600 million were obese.
Vitamin D, also called calciferol, refers to a group of fat-soluble pro-hormones, which exist in two forms, vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Cholecalciferol can be synthesized endogenously in the skin under the influence of solar ultraviolet radiation [8] while it is also found in animal foods. On the other hand, ergocalciferol is derived mainly from plant foods and dietary supplements (National Institute of Health, 2015) [9]. However, both forms of calciferol are converted to 25-hydroxyvitaminD, 25 (OH) D or calcidiol, the inactive storage form of the vitamin, in the liver, and thereafter, calcidiol is converted to the active form of the vitamin, i.e. 1,25-dihydroxyvitamin D or calcitriol, in the kidneys [10]. Based on the International Health Institute, the daily recommended intake (RDAs) for vitamin D for people between 1-70 years is 600IU (15mg) while for people more than 70 years old, the RDA is increased to 800IU (20mg) [9]. However, current recommendations of this vitamin only considered the effects of vitamin D on skeletal tissue [11].
Recently, there has been an epidemic scientific interest about the other, non-skeletal, properties of vitamin D and the potential role of vitamin D on mental, physical health and well-being. Some studies have shown that vitamin D deficiency occurs in obese people [12]. Findings from a recent meta-analysis showed that vitamin D is inversely associated with Body Mass Index (BMI) [13] and that vitamin D deficiency is frequently observed among overweight and obese people compared to normal-weight population [14].
Hence, it is still unknown whether vitamin D deficiency is the causative agent for obesity or the opposite [15]. Notably, obesity affects the biochemical and physiological functions of vitamin D probably due to its deposition in body fat and due to its fatty solubility [16]. In particular, people with high levels of BMI usually have a high body fat content that accumulates part of the fat-soluble vitamin D, leading to increased vitamin D binding, low availability and low vitamin D blood levels [17]. Thus, low levels of vitamin D in obese are likely to be the result and not the cause of obesity as it is blocked by the adipose tissue [18]. However, in animal models, it was shown that the body fat mass can accumulate about 10-12% of the total vitamin D supplementation while at the same time the release of vitamin D from the fat mass is extremely slow and proportional to the vitamin’s D content [16].
Results of a previous systematic review do not clearly demonstrate the benefit of vitamin D in the treatment of obesity [19]. A previous study by Mason et al. [20] reported that the evidence regarding the effect of vitamin D on weight loss and fat loss in obese people remain insufficient. Therefore, the main purpose of this systematic review was to investigate the effect of vitamin D supplementation in decreasing the excessive body weight in overweight and obese patients, as evidenced in randomized controlled trials (RCTs). Specific objectives were to determine the most appropriate dosage, formulation and duration of vitamin D supplementation that are necessary to provide positive outcomes and possibly an effective treatment for overweight and obesity.
Methodology
Search strategy
A systematic review was undertaken using PubMed and EBSCO host databases. The search strategy is shown in Table 1. Only RCTs without chronological limit were considered. Secondary searching of the reference lists of retrieved papers was undertaken, to identify any other RCTs that met the inclusion criteria, as outlined under study selection. When searching in PubMed «Text word» was used as a filter, while in the EBSCO database «AB Abstract» was the only filter.
| Keywords | EBSCO | PubMed | |
|---|---|---|---|
| vitamin d or calciferol or vitamin d3 or cholecalciferol or vitamin d2 or ergocalciferol or 25(OH)D or 25-hydroxyvitamin d or supplement* | #1 | 126870 | 32437 |
| obes* or morbid obes* or waist circumference or sagittal abdominal diameter or waist to hip ratio or waist-to-hip-ratio or waist-to-hip or WHR or BMI or Increas*BMI | #2 | 235261 | 64884 |
| randomized controlled trial or random control trial or random control or RCTs or RCT | #3 | 80478 | 354309 |
| #1 AND #2 AND #3 | 501 | 516 | |
Table 1: Search results per keyword and keyword combination.
Study selection
This review article was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA). PRISMA is an evidence-based set of items for reporting in systematic reviews and meta-analyses, and can be used as a basis for reporting systematic reviews of research evaluations of interventions [21]. A structured approach was used to formulate the research question for this review, using five components commonly known as the Participants, Interventions, Comparators, Outcomes, and Study design approaches (PICOS) [22]:
Participants: Overweight and obese adults (BMI ≥ 25 kg/m2; age ≥ 18 years), no restrictions were placed on gender, race and geographical distribution of the individuals enrolled in the study.
Interventions: vitamin D oral supplementation; the supplements used were either vitamin D or Vitamin D3 or ergocalciferol or Vitamin D2 or cholecalciferol or 25-hydroxyvitamin D or 25 (OH) D3 with or without other co-interventions such as hypocaloric diet, exercise, other supplements such as calcium, proteins, aminoacids.
Comparisons: placebo and other non-vitamin D interventions.
Outcome: changes in Body Weight (BW, kg); changes in Body Mass Index (BMI, kg/m2); changes in circumferences (WC, cm); changes in Body Fat (BF, kg or %); changes in Fat Free Mass (FFM) [lean mass (LM) and muscle mass (MM), both in kg].
Study design: RCTs.
Studies excluded from the selection were: non-RCTs in overweight and obese patients; animal studies; RCTs in adults with BMI<25kg/m2; RCTs in overweight and obese children and adolescent. A p-value of <0.05 was considered statistically significant for all included studies.
Assessment of methodological quality and data extraction
Two authors (C.S. and S.E.) independently extracted the detailed information from the selected trials. Qualitative and quantitative information from each study were extracted, including author and year of study, geographic study location, the study size and age of participants, type of exposure such as the formula, and duration as well as dosage of vitamin D supplementation.
The methodological quality of the included RCTs was assessed by means of 11 predefined categories based on the updated Cochrane Collaboration Back Review Group (CCBRG) method (Table 2) [23]. The internal validity criteria that refer to the characteristics of the study are related to selection bias (criteria 1 and 2), performance bias (criteria 4-8), attrition bias (criteria 9 and 11) and detection bias (criteria 6 and 10) (Table 2). The above criteria were characterized as: “Yes”, “No” or “Don’t know”. Two authors (C.S. and S.E.) used the assessment instrument independently to evaluate the quality of each study. Whenever there was a disagreement between the two investigators, a third author (M.I.) provided an additional evaluation. Accordingly, each study was assessed as of high quality if the total score of positive responses was ≥8 out of 11 and of low quality if the total score of positive responses was ≤ 7 out of 11.
| Randomized C ontrolled Trials | Adequate randomization | Concealed treatment allocation | Similarity of groups at baseline | Patient blinded to the intervention | Care provider blinded to the intervention | Outcome assessor blinded to the intervention | Cointerventions avoided or similar | Acceptable compliance | Acceptable drop-out rate | Similar timing of the outcome assessment | Intention-to treat analysis | Overall score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mason et al., [5] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 / 11 |
| Verreijen et al., [4] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | 10 / 11 |
| Zhu et al., [25] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 10 / 11 |
| Shapses et al., [31] | DK | Y | Y | Y | Y | Y | Y | Y | Y | Y | DK | 9 / 11 |
| Salehpour et al., [26] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | DK | 10 / 11 |
| Major et al., [24] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | N | 9/11 |
| Sneve et al., [18] | DK | Y | Y | Y | Y | Y | Y | Y | Y | Y | DK | 9 / 11 |
Table 2: Quality assessment of seven randomized controlled trials by using the 11 criteria of Van Tulder (Van Tulder et al., 2013).
Results
Search strategy and study selection
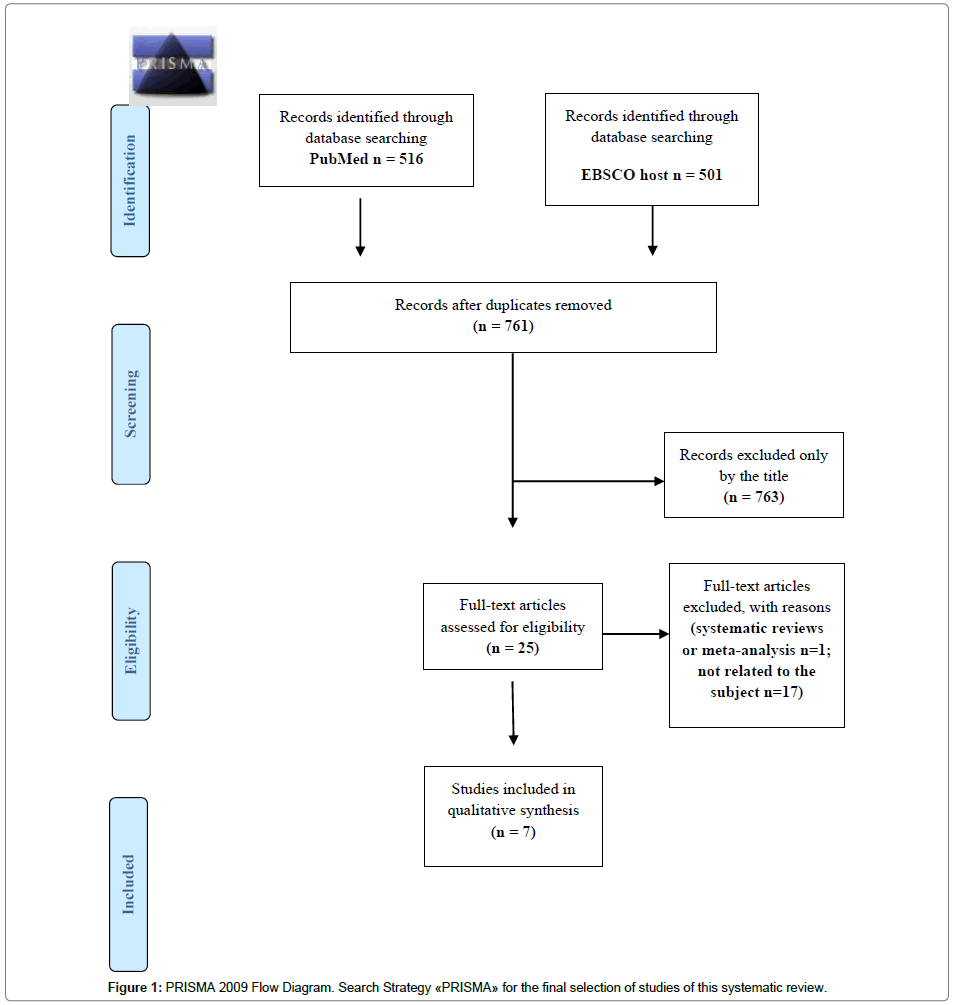
The search strategy and study selection processes were performed according to the “PRISMA” guidelines, as described above. The flow chart of the included studies is presented in Figure 1. Overall, 7 studies were deemed eligible for inclusion in the current analysis.
The quality assessment of the included studies revealed that all 7 studies are of high methodological quality ( ≥ 8/11 validity criteria). Table 2 shows the result of the quality assessment of the included studies.
Description of study characteristics
The information of the study characteristics is summarized in Table 3. The geographic location of each study was different and dispersed worldwide. Notably, cholecalciferol was the only form of vitamin D supplementation used by the researchers. In the studies, the duration of vitamin D supplementation varied between 6 weeks to 12 months.
| First author/ year of publication/country | Subjects (treatment vs. control) | Age (years) | Vitamin D treatment | Treatment duration (weeks/months) | Outcomes |
|---|---|---|---|---|---|
| Mason et al., [5] USA |
Treatment group (n = 109) | 50-75 (postmenopausal women) |
2000 IU/d vitamin D3 PLUS Hypocaloric diet (-500-1000 kcals) +exercise (225 min/wk) |
12 months | BW, BMI, BF, FFM (lean mass) |
| Control group (n = 109) | |||||
| Verreijen et al., [4] Netherlands |
Treatment group (n = 30) | >55 (males and females) |
High whey protein–, leucine-, and vitamin D–enriched Supplement (200μg/wk) PLUS hypocaloric diet (-600kcals) and exercise |
13 weeks | BW, BMI,WC, BF FFM (muscle mass) |
| Control group (n = 30) | |||||
| Zhu et al., [25], CHINA | Treatment group (n = 22) | 18-25 ετÃÂŽν (males and females) |
600 mg Ca + 125 IU vitamin D3/d + hypocaloric diet (-500 kcals) | 12 weeks | BW, BMI, BF, FFM (lean mass) |
| Control group (n = 20) | |||||
| Shapses et al., [31] USA |
Treatment group (n = 40) | 50-70 (postmenopausal women) |
62.5 mg vitamin D3 from a vitamin D3 supplement + 10 mg/d from a multivitamin PLUS hypocaloric diet (500-600 kcals) +exercise |
6 weeks | BW |
| Control group (n = 43) | |||||
| Salehpour et al., [26], IRAN | Treatment group (n = 39) | 18-50 (females) |
25 μg/d vitamin D3 | 12 months | BW, BMI,WC, BF FFM |
| Control group (n = 38) | |||||
| Major et al., [24], USA | Treatment group (n =30 ) | 43 (mean) (females) |
10 μg vitamin D3/d + ≤600 mg Ca /d PLUS hypocaloric diet (–2900 KJ/d). | 15 weeks | BW, BMI,WC, BF |
| Control group (n = 33 ) | |||||
| Sneve et al., [18], NORWAY |
Treatment group (n = 116) | 21-70 (males and females) |
40000 IU vitamin D3/w +500 mg Ca/d | 12 months | BW, BMI, BF |
| Control group (n = 106) |
Table 3: Basic characteristics of the included studies.
Effect of treatment on BW, BMI and WC
In the study by Major et al. [24], showed a statistically significant reduction in BW in the treatment group compared to the control group (-5.8 ± 2.6 kg vs 1.4 ± 2.4 kg, p <0.01). Furthermore, none of the studies showed a statistically significant reduction in BMI between the two groups. In regards to the WC, in the study by Major et al. [24] showed a statistically significant reduction in the treatment group compared to the control group (-5.6 ± 3.3 cm vs 3.5 ± 2.9 cm, p = 0.03). Results of vitamin D supplementation on the above parameters are listed in Table 4.
| Study Outcome |
Mason et al., [20] | Verreijen et al., [4] | Zhu et al., [25] | Shapses et al., [31] | Salehpour et al., [26] | Major et al., [24] | Sneve et al., [18] |
|---|---|---|---|---|---|---|---|
| BW (kg) | -7.1 kg vs -7.4 kg, p = 0.41 |
-3.4 ± 3.6 kg vs -2.8 ± 2.8 kg, p = 0.57 |
-4.1 ± 1.8 kg vs -3.5 ± 1.9 kg, p = 0.25 |
-0.3 ± 1.2 kg vs -3.3 ± 1.2 kg, p = 0.646 |
-0.3 ± 1.5 kg vs -0.1 ±1.7 kg, p = 0.71 |
-5.8 ± 2.6 kg vs -1.4 ± -2.4 kg p < 0.01 |
0.1 ± 3.8 kg vs 0.3 ±3.2 kg vs 0.5 ± 3.9 kg, p > 0.05 |
| BMI (kg/m2) | -2.8 kg /m2 vs -2.8 kg/m, p = 0.58 |
-1.2 ± 1.3 kg /m2 vs -1.0 ± 0.9 kg /m2, p = 0.49 |
-1.8 ± 0.2 kg /m2 vs -1.5 ± 0.5 kg /m2, p = 0.86 |
ND | -0.13 ± 0.6 kg/m2 vs -0.04 ± 0.6 kg/m2, p = 0.5 |
-2.2 ± 0.9 kg/m2 vs -0.5 ± 0.9 kg/m2 p = 0.12 |
0.0 ± 1.3 kg /m2 vs 0.1 ±1.1 kg /m2 vs 0.2 ± 1.4 kg /m2, p > 0.05 |
| WC (cm) | ND | -4.4 ± 4.0 cm vs -3.7 ± 5.1 cm, p = 0.50 |
ND | ND | -0.3 ± 4.3 cm vs 0.4 ± 4.1 cm, p = 0.38 |
-5.6 ± 3.3 cm vs -3.5 ± 2.9 cm p = 0.03 |
ND |
| BF | -4.1 % vs -3.5 %, p = 0.70 |
-3.2 ± 3.1kg vs -2.5 ± 2.4kg, p = 0.32 |
-2.8 ± 1.3 kg vs -1.8 ± 1.3 kg, p = 0.02 |
ND | -2.7 ± 2.1 kg vs -0.47 ± 2.1 kg, p < 0.001 |
-4.7 ± 2.3 kg vs -1.2 ± 2.4 kg p = 0.0009 |
-0.3 ± 2.1% vs -0.4 ± 1.9% vs -0.5 ± 2.1%, p > 0.05 |
| FFM (kg) | -0.8 kg vs -1.1 kg, p = 0.53 |
+0,4 ± 1,2 kg vs -0.5 ± 2.1 kg, p = 0.03 |
-1.1 ± 1.1 kg vs -1.4 ± 1.2 kg, p = 0.31 |
ND | +1.8 ± 2.1 kg vs +0.4 ± 2.1 kg, p < 0.001 |
ND |
ND |
Table 4: The effect of Vitamin D treatment on the main study outcomes as examined in the current analysis.
Effect of treatment on BF and FFM
In the study by Zhu et al. [25], showed that BF was significantly reduced in the treatment group compared to the control group (-2.8 ± 1.3 kg vs 1.8 ± 1.3 kg, p = 0.02). Furthermore, in the study by Salehpour [26], BF also showed a significant reduction in the treatment group compared to the control group (-2.7 ± 2.1 kg vs 0.47 ± 2.1 kg, p <0.01). In addition, the same results were shown in the study by Major et al. [24] (treatment group vs control group: -4.7 ± 2.3 kg vs 1.2 ± 2.4 kg, p = 0.009). Results of vitamin D supplementation on BF are listed in Table 4.
In regards to the FFM (LM and MM), in the study by Verreijen et al., the MM significantly increased in the treatment group compared to the control group (+0.4 ± 1.2 kg vs 0.5 ± 2.1 kg, p=0.03). Moreover, in the study by Salehpour et al.[26], FFM was significantly increased in the treatment group compared to the the control group (+1.8 ± 2.1 kg vs + 0.4 ± 2.1 kg, p <0.001). Results of vitamin D supplementation on FFM are listed in Table 4.
Discussion
The current review aimed to assess the effect of vitamin D treatment on overweight and obesity. 7 studies were eligible for inclusion and all studies have used the same type of supplementation (cholecalciferol). Notably, only one study (Salehpour et al.) [26] has used cholecalciferol as a single treatment whereas all the other studies used a combined treatment with other substitutes. 4 studies [4,24-26] out of 7 have shown significant changes on fat distribution (BF, FFM) and only one study [24] has shown changes on anthropometric markers (BW, WC).
Effect of treatment on anthropometric parameters (BW, BMI, WC)
In regards to the effect of vitamin D on the anthropometric markers (BW, BMI and WC) significant findings were limited in only one study [24]. In the particular study, vitamin D was administered with calcium and a hypocaloric diet. Indeed, Vitamin D is critical for calcium metabolism, and it is difficult to separate the effects of vitamin D [27]. Thus, it is still unclear whether vitamin D alone may has any additional effects on the examined anthropometric markers. However, the above evidence is not yet complete enough to be compelling, and further research is needed.
Effect of treatment on BF and FFM
On the other hand, the findings related to fat distribution are more intense compared to those related on anthropometric markers. In particular, 4 studies [4,24-26] have shown significant positive effects of vitamin D treatment on BF and FFM. However, the different co-interventions among the studies complicate the interpretation and credibility of our findings. Particularly, in the studies by Zhu et al. [25] and Major et al. [24], vitamin D supplementation was combined with calcium and hypocaloric diet. However, it could be assumed that both co-interventions may have enforced for the loss of BF and thus, made our findings more controversial. However, in the study by Salehpour, et al. [26], vitamin D was administered alone indicating a clear positive effect of vitamin on BF and FFM. Thus, the particular treatment (25 μg/day/cholecalciferol/12 months) seems to be more effective compared to the other treatment combinations. However, this is the only study, and even though is a high quality study there is still a need to conduct more similar studies in order to identify the best treatment combination (dose, duration) for overweight and obesity. Notably, in the studies by Verreijen, et al. [4] and Salehpour, et al. [26] significant positive effects were shown on MM and FFM, respectively. Notably, in the study by Verreijen [4], vitamin D was administered with other proteins and amino acids (leucine) supplements. However, it is well documented that branched chain amino acids (BCAA) such as leucine, can promote muscle protein synthesis and increase muscle growth over time [28]. Therefore, the increase in muscle mass or part of it may be due to the BCAA and not due to the real action of vitamin D on muscles. In contrary, a recent study by Kouskoukis [29] showed that administration of vitamin D may improve muscle strength and body balance while vitamin D deficiency can cause muscle weakness. Notably, in the study by Verrejen et al. [4] exercise was also included and this might have affected the findings. Exercise is well correlated with the development of muscle mass. In particular, aerobic exercise increases energy expenditure leading to fat loss, increases muscular strength and muscle mass and prevents the loss of muscle mass [30]. In contrary, in the study by Salehpour et al. [26], vitamin D was supplemented alone, without exercise, indicating, once again the potential effect of vitamin D on FFM.
The current analysis found that 2 of the included studies [20,31] have shown no significant effect on any of the examined parameters. It worth to mention that both studies have included postmenopausal women. Thus, it could be assumed that menopause may reduce vitamin D activity. However, it is well documented that vitamin D absorption and biosynthesis is significantly reduced among older people (usually 65 and over) [32]. Therefore, based on the above findings it could be assumed that vitamin D may has potential effect on the treatment of overweight and obesity among young people while its effects among the elderly are diminished.
Limitations and strengths
The limitations vary according to the studies included. Vitamin D was not administered on its own but rather as a combination treatment with other factors (hypocaloric diet, the exercise and other supplements such as calcium, amino acids etc.) that are indicated for weight loss. This may also altered the effect of vitamin D in weight loss. Also, RCTs were limited, while heterogeneity (ethnicity, gender, age of participants, duration and amount of the included studies vitamin D supplementation) was evident in measures of exposure and outcomes. Finally, a meta-analysis could not be performed since the outcomes were not measured in a similar enough manner to be mathematically combined. Strengths of this review include the exclusive inclusion of RCTs, as well as the high methodological quality of all the included studies. Moreover, all studies have used the same form of supplementation (cholecalciferol) making the current findings much more comparable and credible.
Conclusions
This systematic review provides suggestions and impetus for determining whether vitamin D has a positive effect on overweight and obesity. There are plausible mechanisms and some in vitro evidence supporting a role for vitamin D in weight reduction but it remains difficult to determine which effects are due to vitamin D itself and which are mediated via calcium or other factors. Clinical trials have not been conclusive. Some studies showed no effects of vitamin D supplementation on weight parameters while some other studies demonstrated more effects on BF and FFM. The overall impression is that vitamin D alone or not appears not to have a definite effect on the examined anthropometric markers, but it may affect fat mass and distribution. Nonetheless, there is a clear need for more, high quality studies-interventions in order to clarify the effects of vitamin D on overweight and obesity. To date, there is not enough scientific evidence to support the use of vitamin D as a pathway to prevent and/or treat obesity.
References
- Guh D, Zhang W, Bansback N, Amarsi Z, Birmingham C et al. (2009) The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public health 9: 1-20.
- Plessas T, Kidziou, E (2007) Obesity and cellulitis. Farmakon, Athens.
- Panagi Z (2008) Estimation of levels of fat-soluble vitamins in blood serum of hyper-obese patients who have undergone a Roux-en-Y gastric bypass surgery with cholecogranial deflection. Postgraduate dissertation, University of Patras.
- Verreijen A, Verlaan S, Engberink M, Swinkels S, Bosch J, et al. (2015) A high whey protein-, leucin-, and vitamin D- enriched supplement preserves muscle mass during intentional weigh loss in obese older adults: a double-blind randomized controlled trial. Am J Clin Nutr 101: 279-286.
- Duggan C, Tapsoba J, Mason C, Imayama I, Korde L, et al. (2015) Effect of Vitamin D3 supplementation in combination with weight loss on inflammatory biomarkers in postmenopausal women: a randomized controlled trial. Cancer Prev Res 8: 628-635.
- World Health Organization, 2016. Obesity and Overweight.
- Bouaziz W, Schmitt E, Kaltenbach G, Geny B, Vogel T (2015) Health benefits of endurance training alone or combined with diet for obese patients over 60: a review. Int J Clin Pract 69: 1032-49.
- Lazzeroni M, Serrano D, Pilz S, Gandini S (2013) Vitamin D supplementation and cancer: review of randomized controlled trials. Anticancer Agents Med Chem 13: 118-25.
- National Institute of Health, 2015.
- Nair R, Maseeh A (2012) Vitamin D: The “sunshine” Vitamin. J Pharmacol Pharmacother 3: 118-126.
- Ross AC, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. (2011) Dietary reference intakes for vitamin D and calcium. In Dietary Reference Intakes for Calcium and Vitamin D. National Academies Press.
- Shantavasinkul CP, Phanachet P, Puchaiwattanon O, Chailurkit L, Lepananon T, et al. (2014) Vitamin D status is determinant of skeletal muscle mass in obesity according to body fat percentage. Nutrition 31: 801-806.
- Saneei P, Salehi-Abargouei A, Esmaillzadeh A (2013) Serum 25-hydroxy vitamin D levels in relation to body mass index: a systematic review and meta-analysis. Obesity Reviews 4: 393-404.
- Pereira - Santos PM, Costa FRP, Assis OMA, Santos TSAC, Santos BD (2014) Obesity and Vitamin D deficiency: a systematic review and meta-analysis. Obes Rev 16: 341-349.
- Almazroea A (2016) Is Vitamin D deficiency a cause or result of childhood obesity? Saudi Journal for health Sciences 5: 1-5.
- Rani K, Memon RA, Akram M, Memon LP (2016) Obesity; Association of serum vitamin D levels. The Professional Medical Journal 23: 665-668.
- Lagunova Z, Porojnicu CA, Lindberg F, Hexeberg S, Moan J (2009) The Dependency of Vitamin D Status on Body Mass Index, Gender, Age and Season. Anticancer Res 29: 3713-3720.
- Jorde R, Sneve M, Emaus N, Figenschau Y, Grimnes G (2010) Cross-sectional and longitudinal relation between serum 25-hydroxyvitamin D and body mass index: the Tromso study. Eur J Nutr 49: 401-407.
- Zuk A, Fitzpatrick T, Rosella C.L (2015) Effect of Vitamin D3 Supplementation on Inflammatory Markers and Glycemic Measures among Overweight or Obese Adults: A systematic Review of Randomized Controlled Trials. Plos One 11: 1-23.
- Mason C, Xiao L, Imayama I, Duggan C, Wang C, et al. (2014) Vitamin D3 Supplementation during weight loss: a double-blind randomized controlled trial. Am J Clin Nutr 99: 1015-1025.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: 1-6.
- O'Connor D, Green S, Higgins JPT (2008) Defining the review question and developing criteria for including studies. In Cochrane Handbook for Systematic Reviews of Interventions John Wiley & Sons, Ltd. 81-94.
- Van Tulder M, Furlan A, Bombardier C, Bouter L (2003) Update method guidelines for systematic reviews in the Cochrane Collaboration Back Review group. Spine 28: 1290-1299.
- Major G, Alarie F, Dore J, Tremblay A (2009) Calcium plus vitamin D supplementation and fat mass loss in female very low-calcium consumers: potential link with calcium-specific appetite control. British Journal of nutrition 101: 656-663.
- Zhu W, Cai D, Wang Y, Lin N, Hu Q, et al. (2013) Calcium plus Vitamin D3 supplementation facilitated Fat loss in overweight and obese college students with very-low calcium consumption: a randomized controlled trial. Nutr J 12: 1-8.
- Salehpour A, Hosseinpanah F, Shidfar F, Vafa M, Razaghi M, et al. (2012) A 12-week double-blind randomized clinical trial of vitamin D3 supplementation on body fat mass in healthy overweight and obese women. Nutr J 11: 1-8.
- Vanlint S (2013) Vitamin D and obesity. Nutrients 5: 949-956.
- Sfakianaki E (2015) Protein supplements and muscle growth. Graduate thesis, Technological Educational Institute of Crete.
- Kouskoukis E A (2016) Diagnostic and prognostic evaluation of vitamin D levels in systemic diseases. Doctoral thesis, Democritus University of Thrace.
- Nicolaou I (2013) Nutrition and exercise for weight control. Graduate thesis, Higher Technological Educational Institute of Crete.
- Shapses S, Sukumar D, Schneider S, Schlussel Y, Sherrell R, et al. (2013) Vitamin D supplementation and calcium absorption during caloric restriction: a randomized double-blind trial. Am J Clin Nutr 97: 637-645.
- Papapetrou D (2002) The treatment of osteoporosis. Society and Health: Current Health Problems and Treatment 3: 215-226.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi