Research Article, J Womens Health Issues Care Vol: 6 Issue: 6
The Prevalence of Maternal Depression in a Primary Care Setting, in a Small Island State with a High GNI per Capita
Persad Varsha*, Peters Arrianna, Pheerangee Michael, Peter Sabrina, Phakira Amy, Phillips Anton, Pinder Alphonette and Mungrue Kameel
University of the West Indies, FMS, Department of Paraclinical Sciences, St Augustine, Trinidad and Tobago
*Corresponding Author : Varsha Persad
University of the West Indies, FMS, Department of Paraclinical Sciences, St Augustine, Trinidad and Tobago
Tel: (868) 645 2018
E-mail: varsha.a.persad@gmail.com
Received: October 09, 2016 Accepted: November 06, 2017 Published: November 10, 2017
Citation: Varsha P, Arrianna P, Michael P, Sabrina P, Amy P, et al. (2017) The Prevalence of Maternal Depression in a Primary Care Setting, in a Small Island State with a High GNI per Capita. J Womens Health, Issues Care 6:6. doi: 10.4172/2325-9795.1000288
Abstract
Objective: The aim of this study is to measure the prevalence of maternal depression in a primary care setting in North-Central Trinidad a small island developing country and to determine its socioeconomic, geographic and health-related risk factors.
Methods: A cross sectional observational study to determine the point prevalence of maternal depression in women attending primary care facilities in North Central Trinidad was conducted. The population consisted of all pregnant women attending primary care facilities. The systematic sample of 400 women was taken. A two part questionnaire was administered after informed verbal consent. The questionnaire collected demographic data and the nine item PHQ questionnaire was administered.
Results: Six hundred and two patients were entered into the study, consisting of 441 antenatal women and 161 postnatal women. The point prevalence of post partum depression was 38.5(95% CI 31.046.5), and prenatal depression 49.7%.
Conclusion: The study provides evidence that MD is common in the developing world, detection and treatment therefore must be a priority as children born to mothers with depression have more behavioral problems, more psychiatric illness, more visits to pediatricians, lower IQ scores, and attachment issues.
Keywords: Maternal depression; Primary care; Pregnant women
Introduction
The prevalence and determinants of mental health problems in women during pregnancy and in the year after giving birth in developed countries have been extensively investigated [1]. On the other hand women living in low-income and middle-income countries have only recently become the subject of research [2]. Several reasons have been advanced for this discrepancy such as the greater need to provide adequate services to prevent both infant and maternal mortality, and women are protected from experiencing perinatal mental problems through the influence of social and traditional cultural practices during pregnancy and in the postpartum period [3]. Notwithstanding depression and anxiety are both prevalent and disabling mental health disorders, contributing not only to human suffering and loss of health, but also lost of economic output. In 2010 worldwide, an estimated $2.5-8.5 trillion (USD) in lost economic output was attributed to mental, neurological and substance use disorders [4,5].
In view of this emerging burden, the promotion of mental health and wellbeing previously addressed in Millennium Development Goal-5 (improving maternal mental health), have been explicitly included in the United Nations 2015–30 Sustainable Development Goals (SDG), which provides the foundation for the urgent global response to this massive public health and economic challenge [6]. A search revealed no studies devoted to measuring the prevalence of maternal depression (MD) in Trinidad and Tobago (TTO) a country with a high ($17640 USD) gross national income per capita (GNI) hence the critical need for this study.
MD is a range of conditions that can affect women during pregnancy and up to one year postpartum. The spectrum of conditions includes prenatal depression (PD), the „baby blues,” postpartum depression (PPD) and postpartum psychosis. MD is associated with higher rates of adverse pregnancy outcomes such as preterm birth, low birth weight, operative delivery, and longer pre-delivery hospital stay [7]. MD is also associated with prenatal hypertension [8], gestational diabetes, [9] preeclampsia [10], the haemolysis elevated liver enzymes and low platelet count syndrome (HELP) [11], poorer infant attachment and an overall unfavorable impact on infant and child development [12]. Changes in sleep pattern, appetite, lethargy, complications of delivery all associated with pregnancy, as well as the demands of caring for a newborn adversely impacts on MD [13]. In the postpartum period, women are particularly vulnerable to a major depressive episode, whether a first episode or a recurrence.
In one review during the first three months of the postpartum period the estimated prevalence of a depressive episode was as high as 19.2% [14], ranking PPD the most common complication of childbearing [15], yet it is largely under recognized and undertreated [16]. Both PD and PPD if left untreated can be devastating for mother, infant, and family [17]. MD is associated with poorer overall health status, patients are more likely to engage in behaviours that pose risk to the developing foetus such as smoking [18], alcohol consumption, and substance use [19], have poor nutrition and inadequate weight gain [20,21], and tend to miss more prenatal appointments [22,23]. Mothers with PPD are more likely than mothers without to have impaired bonding, and to be less responsive to their infant’s needs [24]. PPD affects maternal-infant interactions including maternal withdrawal, disengagement, intrusion and hostility, and can lead to long term effects on child development, including poor cognitive functioning, emotional maladjustment, and behavioral inhibition [25,26]. Infants and children of mothers with untreated postpartum depression have been shown to exhibit a higher incidence of colic, excessive crying, sleep problems, and irritability [27,28]. Women with postpartum depression may be less likely to initiate or maintain breastfeeding, and depressive symptoms have been noted to precede the discontinuation of breastfeeding [29]. Evidence suggests that depressed pregnant women are less attached to the developing baby and more likely to have elective terminations [30]. PPD in particular and its link to infant mortality [31] is an important international health indicator.
Risk factors for depression during pregnancy include past episodes of depression, current anxiety, poor social support, unintended pregnancy, life stress, being single and domestic violence [32]. There is converging evidence of a subset of women particularly sensitive to dramatic fluctuations in levels of estradiol and progesterone that occur during childbirth [33]. There is also evidence that dysregulation of the hypothalamic-pituitary-adrenal axis contributes to the development of PPD in certain women [5].
In 2016, the US Preventive Services Task Force issued a recommendation that all pregnant and postpartum women be screened for depression [34-36], highlighting the need for all medical providers to be alert to the potentially serious consequences of unrecognized and untreated mental health disorders. The American College of Obstetricians and Gynecologists (ACOG) recommends screening for depression and anxiety at least once during the peripartum period [37], and the American Academy of Paediatrics recommends screening mothers for depression at 1-month, 2-month, and 4-month postnatal visits [38]. The detection and treatment of mental health disorders in childbearing have been shown to be cost effective [39,40].
Therefore, the aim of this study is to measure the point prevalence of PD and PPD in a primary care setting in North-Central Trinidad a small island high GNI per capita and to determine its socioeconomic, geographic and health-related risk factors.
Methods
A cross sectional design was used. The population consisted of pregnant women attending primary care facilities in North-Central Trinidad. We calculated a sample size of 500 based on a prevalence rate of 12% with a 95% confidence interval. Data were collected using a pretested structured questionnaire. The questionnaire consisted of two parts, the first part collected sociodemographic data which included age, ethnicity, geographical location, marital status, employment status, as well as obstetrical data such as gravidity, parity, occurrence of anaemia and gestational diabetes (GD), obesity, the use of contraceptives, and gestational age. In TTO a 2-h 75 g OGTT at 24-28 weeks of gestation is the method used to determine GD as recommended both by the European Association for the Study of Diabetes, International Association of Diabetes and Pregnancy Study Group (IADPSG), ADA and World Health Organization (WHO) [41]. For postpartum participants, data on birth weight and complications during delivery were also collected. Obesity was identified by self-reporting based on patients’ perception of their weight, as opposed to BMI.
The second part of the questionnaire was a replication of the Patient Health Questionnaire-9 (PHQ-9) an instrument designed to screen for depression in primary care. The American College of Obstetricians and Gynaecologists (ACOG), the American Academy of Pediatrics, and the US Preventive Services Task Force recommend a standardized validated tool and cite both the Edinburgh Postnatal Depression Scale (EPDS) and the Patient Health Questionnaire-9 (PHQ-9) as appropriate to screen for MD depression [42]. We choose the PHQ-9 as the study was conducted in a primary care setting, having been validated in primary care obstetric patients. The PHQ-9 is a multipurpose instrument for screening, diagnosing, monitoring and measuring the severity of depression [43]. The PHQ-9 incorporates DSM-IV depression diagnostic criteria with other leading major depressive symptoms into a brief self-report tool [44]. The diagnostic validity of the PHQ-9 was established in studies involving 8 primary care and 7 obstetrical clinics where PHQ scores ≥10 has a sensitivity of 88% and a specificity of 88% for major depression. Advantages of the publicly accessible PHQ-9 include its self-reporting format, rapid scoring and interpretation, availability in multiple languages, suitable for remote administration and sensitivity to treatment-associated change. For the purposes of this study MD was defined only as PD assessed in antenatal clinics (AC) and PPD assessed in postnatal clinics (PNC).
The questionnaire was administered to mothers by interview after informed verbal consent while attending AC and PNC on a single point time cluster sampling. These clinics have high attendance rates annually about 56 000 pregnant mothers visited the primary care facilities for antenatal care and return after delivery where both mother and baby are assessed together and is representative of the population. The population of Trinidad consists of two major diaspora Africans and East Indians (EI) both representing approximately 40% of the population. AC participants were assessed throughout the pregnancy to 38 weeks gestation; thereafter patients were referred to the main tertiary center for delivery while postpartum participants were interviewed from 2-12 months after giving birth.
The PHQ-9 was scored 0-27, 0-4 indicates no depression or PHQ (-), all scores ≥5 were defined as PHQ-9 (+). A score on the PHQ-9 ranging from 5-10 indicates mild depression, 11-14 moderate depression, 15-19 moderate to severe depression, and ≥20 severe depression. Screened patients with a score of ≥5 were given a referral letter addressed to their health care physician stating their provisional diagnosis based on their PHQ-9 score. Patients with blindness, deafness, or impaired locomotion were excluded from the study. As our primary focus was on measuring prevalence, we did not investigate women who experienced difficulties such as having a partner who rejected paternity, who was unsupportive and uninvolved, or critical and quarrelsome, and who used alcohol to excess, abusive or suffered intimate partner violence or had conflicts with in-laws. The internal validity of the instrument was assessed using Cronbach α. The DSM-V was also administered as a gold standard to 100 randomly selected participants to determine sensitivity and specificity in this setting to ensure diagnostic validity of the PHQ-9. A Pearson’s Chi squared test was used to establish association between categorical variables.
Bivariate logistic regression was first fitted to identify potential significant risk factors and variables with a p-value greater than 0.05 were removed from the multiple logistic regression model using backward selection method to identify associated factors with depression. Adjusted odds ratio with its 95% confidence interval was calculated to report the strength and significance of the association. We used ARC GIS (ESRI) vs. 10.0 to map the location of women with PPD. Ethical approval for the study was obtained from the University of the West Indies Ethics Committee.
Results
Overall 602 patients were recruited for the study, 441 prenatal patients between 2-37 weeks gestation and 161 postnatal patients. Only 55 patients refused to participate in the study giving a response rate of 91.6%. The mean age of postnatal patients was (29.6 yr., interquartile range of 25-33) marginally higher than prenatal patients (28.1 yr., interquartile range 24-32). The predominant age group of study participants was 26-30 yrs., and represented 28% of the sample while younger (15-20 yrs.) and older women (>36 yrs.) represented approximately 12% of the sample (Table 1).
| Characteristic | PHQ-9 (+) n (%) | PHQ-9 (-) n(%) | Sample n (%) | Characteristic | PHQ-9 (+) n (%) | PHQ-9 (-) n(%) | Sample n (%) |
|---|---|---|---|---|---|---|---|
| Age (yrs.) | Ethnicity | ||||||
| 15-20 | 26(5.9) | 25(5.7) | 51(11.6) | African | 63(14.3) | 72 (16.3) | 135(30.6) |
| 21-25 | 73(16.6) | 42(9.5) | 115(26.1) | East Indian | 72 (16.3) | 70 (15.9) | 142(32.2) |
| 26-30 | 67(15.2) | 57(12.9) | 124(28.1) | Mixed race | 81(18.4) | 79(17.9) | 160(36.3) |
| 31-35 | 34 (7.7) | 63(14.3) | 97(22.0) | Other | 3 (0.7) | 1 (0.2) | 4(0.9) |
| >35 | 19 (4.3) | 35(7.9) | 54(12.2) | - | |||
| Total | 219 (49.7) | 222 (50.3) | 441(100) | Total | 219(49.7) | 222(50.3) | 441(100) |
| Anaemia | Employment | ||||||
| Anaemia (P) ζ | 93 (21.1) | 92(20.9) | 185(42.0) | Employed | 122(27.7) | 134 (30.4) | 256(58.0) |
| Anaemic (A) ξ | 126(28.6) | 130(29.5) | 256(58.0) | Unemployed | 97 (22.0) | 88 (20.0) | 185(42.0) |
| Total | 219(49.7) | 222(50.3) | 441(100) | Total | 219(49.7) | 222(50.3) | 441(100) |
| Pt. Perception of Wt. | Marital Status | ||||||
| Underweight | 7(1.6) | 6(1.4) | 13(2.9) | Single | 36(8.2) | 32(7.3) | 68(15.4) |
| Normal | 171(38.8) | 176(39.9) | 347(78.7) | Married | 67(15.2) | 83(18.8) | 150(34.0) |
| Overweight | 40(9.1) | 37(8.4) | 77(17.5) | Common law | 70(15.9) | 74 (16.8) | 144(32.7) |
| Obese | 1(0.2) | 3(0.7) | 4(0.9) | Other | 13(2.9) | 10(2.3) | 23(5.2) |
| Total | 219(49.7) | 222(50.3) | 441(100) | Non-response | 33(7.5) | 23(5.2) | 56(12.7) |
| Gestational Diabetes | Total | 219(49.7) | 222(50.3) | 441(100) | |||
| Yes | 8(1.8) | 23(5.2) | 31(7.0) | Contraceptive use | |||
| No | 209(47.8) | 196(45.1) | 410(93.0) | Yes | 27(6.1) | 29(6.6) | 56(12.7) |
| Total | 219(49.7) | 222(50.3) | 441(100) | No | 192(43.5) | 193(43.8) | 385(87.1) |
| Parity | Total | 219(49.7) | 222(50.3) | 441(100) | |||
| Primigravida | 86(19.5) | 85(19.3) | 171(38.8) | Gest. Age (wks.) | |||
| 1+ | 66(15.0) | 72(16.3) | 138(31.3) | <13 | 15(3.4) | 10(2.3) | 25(5.7) |
| 2+ | 40(9.1) | 35(7.9) | 75(17.0) | 13-27 | 76(17.2) | 92(20.9) | 168(38.1) |
| 3+ | 12(2.7) | 17(3.9) | 29(6.6) | >28 | 128(29.0) | 120(27.2) | 248(56.2) |
| 4+ | 8(1.8) | 4(0.9) | 12(2.7) | Total | 219(49.7) | 222(50.3) | 441(100) |
| 5+ | 7(1.6) | 9(2.0) | 16(3.6) | Gravidity | |||
| Total | 219(49.7) | 222(50.3) | 441(100) | 1 | 72(16.3) | 75(17.0) | 147(33.3) |
| Complications | 2 | 56(12.7) | 56(12.7) | 112(25.4) | |||
| Yes | 13(2.9) | 21(4.8) | 34(7.7) | 3 | 44(10.0) | 42(9.5) | 86(19.5) |
| No | 206(46.7) | 201(45.6) | 407(92.3) | 4 | 25(5.7) | 24(5.4) | 49(11.1) |
| Total | 219(49.7) | 222(50.3) | 441(100) | 5+ | 22(5.0) | 25(5.7) | 47(10.7) |
| Total | 219(49.7) | 222(50.3) | 441(100) |
Table 1: Distribution of PD measured by PHQ (+) score, no depression PHQ-9 (-) among a sample of patients attending antenatal primary care facilities by age, ethnicity, anaemia, marital status, employment, gestation diabetes and contraceptive use.
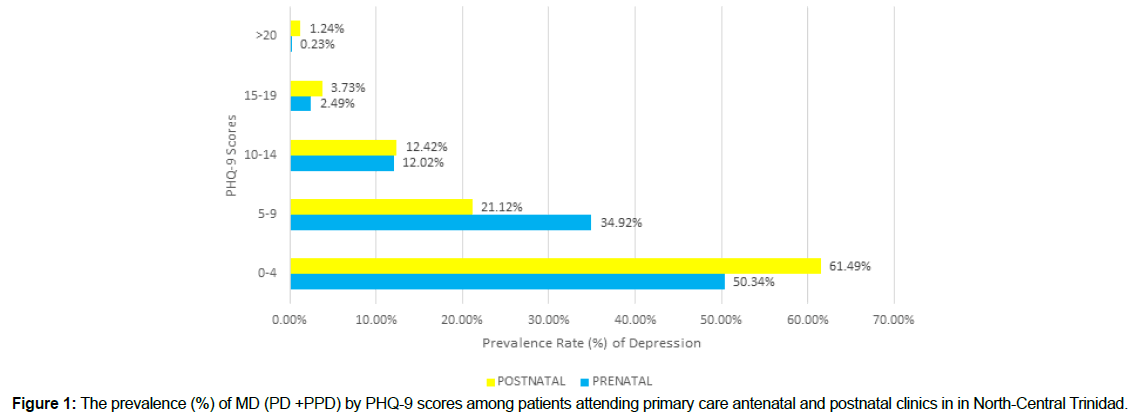
The point prevalence of PD was 49.7% (95% CI 44.9 – 54.4) and PPD was 38.5% (95% CI 31.0 – 46.5). Thus the prevalence of PD (49.7%) was significantly (p<0.001) higher than PPD (38.5%). A total 61.5% of postnatal and 50.3% of prenatal patients scored 0-4 and therefore did not meet the criteria for MD. Among patients with minimal symptoms (a score of 5-9), there were more prenatal women (34.9%) than postnatal (21.1%), (Figure 1). However, for PHQ-9 scores, 10-14, 15-19 and >20, there were more postpartum women than preterm women, although the differences were not significant (p>0.05), Figure 1. Overall as the degree of depression increased as reflected by increasing PHQ- 9 scores i.e. from 5 -27 the prevalence of depression decreased.
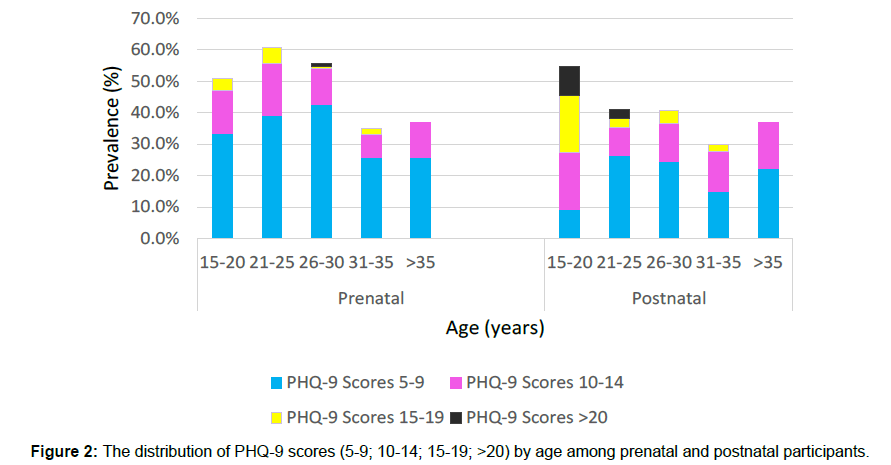
The age group 21-25 among prenatal patients had the highest proportion of PHQ-9 positive scores (60.9%, 115), similarly the age group 15-20 among postnatal patients had the highest proportion of PHQ-9 positive scores (54.6%, 11) (Figure 2). Subsequently with increasing age (21-25 to >36) there was a decline in the proportion of patients with positive PHQ-9 scores (Figure 2). The proportion of prenatal patients with minimal symptoms of MD (PHQ-9 scores 5-9) increased with increasing age until the age range 26-30, thereafter a decline was observed with increasing age. A similar pattern however was not seen among postnatal patients. The age range of 26-30 was the only one that showed the presence of severe PD, i.e. a PHQ-9 score of 20 or greater.
The prevalence of PPD decreased with increasing age, except for the age group of >35 which showed an increase of 7.0% from the prevalence of the previous age range (31-35).
The prevalence of PPD (in scores >5) decreased with age such that the 15-20 age group had the highest prevalence (53%) as compared to women >35.
The age group 15-20 showed the highest proportion of PHQ-9 positive scores for PPD, i.e. scores of 5 and above. Additionally, this age group represented the highest proportion of moderately severe PPD, where 33.3% of the total number of PHQ-9 positive patients for that age range scored 15-19.The presence of patients with severe PPD (scores 20 and above) within the youngest two age groups (15-20 and 21-25), with none in older age groups, was not significant (p>0.05). Thus, it did not represent a pattern of severe PPD declining with increasing age (Figure 3).
There were 48 patients with gestational diabetes (GD) resulting in a prevalence of 8%. A third of patients (29.4%) presented with MD in the postpartum period and one-quarter (25.8%) prenatal patients had PD.
Therefore, this was considered a significant difference. Anaemia however is not correlated to PD (p=0.237) as the occurrence of maternal depression among women who had anaemia compared to women who did not was 50.3% and 49.2% respectively Table 2.
| Characteristics | PHQ-9 (+) n (%) | PHQ-9 (-) n (%) |
Sample n (%) | Characteristic | PHQ-9 (+) n (%) | PHQ-9 (-) n (%) | Sample n (%) |
|---|---|---|---|---|---|---|---|
| Age (yrs) | Ethnicity | ||||||
| 15-20 | 6(3.7) | 5(3.1) | 11(6.8) | African | 15(9.3) | 34(21.1) | 49(30.4) |
| 21-25 | 14(8.7) | 20(12.4) | 34(21.1) | East Indian | 16(9.9) | 28(17.4) | 44(27.3) |
| 26-30 | 20(12.4) | 29(18.0) | 49(30.4) | Mixed race | 31(19.3) | 36(22.4) | 67(41.7) |
| 31-35 | 12(7.5) | 28(17.4) | 40(24.9) | Other | 0(0.0) | 1(0.6) | 1(0.6) |
| >35 | 10(6.2) | 17(10.6) | 27(16.8) | - | |||
| Total | 62(38.5) | 99(61.5) | 161(100) | Total | 62(38.5) | 99(61.5) | 161(100) |
| Anaemia | Employment | ||||||
| Anaemia (P) ζ | 21(13.0) | 37(23.0) | 58(36.0) | Employed | 30(18.6) | 61(37.9) | 91(56.5) |
| Anaemic (A) ξ | 41(25.5) | 62(38.5) | 103(64.0) | Unemployed | 32(19.9) | 38(23.6) | 70(43.5) |
| Total | 62(38.5) | 99(61.5) | 161(100) | Total | 62(38.5) | 99(61.5) | 161(100) |
| Pt Perception of Wt. | Marital Status | ||||||
| Underweight | 3(1.9) | 1(0.6) | 4(2.5) | Single | 10(6.2) | 10(6.2) | 20(12.4) |
| Normal | 44(27.3) | 87(54.0) | 131(81.3) | Married | 18(11.2) | 39(24.2) | 57(35.4) |
| Overweight | 14(8.7) | 11(6.8) | 25(15.5) | Common law | 15(9.3) | 29(18.0) | 44(27.3) |
| Obese | 1(0.6) | 0(0.0) | 1(0.6) | Other | 3(1.9) | 1(0.6) | 4(2.5) |
| Total | 62(38.5) | 99(61.5) | 161(100) | No response | 16(9.9) | 20(12.4) | 36(22.3) |
| Gestational Diabetes | Total | 62(38.5) | 99(61.5) | 161(100) | |||
| Yes | 5(3.1) | 12(7.5) | 17(10.6) | Contraceptive use | |||
| No | 57(35.4) | 87(54.0) | 144(89.4) | Yes | 12(7.4) | 14(8.7) | 26(16.1) |
| Total | 62(38.5) | 99(61.5) | 161(100) | No | 50(31.1) | 85(52.8) | 135(83.9) |
| Gravidity | Total | 62(38.5) | 99(61.5) | 161(100) | |||
| 1 | 19(11.8) | 23(14.3) | 42(26.1) | ||||
| 2 | 14(8.7) | 29(18.0) | 43(26.7) | Complications | |||
| 3 | 14(8.7) | 21(13.0) | 35(21.7) | Yes | 6(3.7) | 20(12.4) | 26(16.1) |
| 4 | 5(3.1) | 13(8.1) | 18(11.2) | No | 44(27.3) | 61(37.9) | 105(65.2) |
| 5+ | 10(6.2) | 13(8.1) | 23(14.3) | C-sections | 12(7.5) | 18(11.2) | 30(18.7) |
| Total | 62(38.5) | 99(61.5) | 161(100) | - | |||
| Parity | Total | 62(38.5) | 99(61.5) | 161(100) | |||
| Primigravida | 0(0) | 0(0) | 0(0) | Birth weight (g) | |||
| 1+ | 24(14.9) | 31(19.3) | 55(34.2) | <2500 (low) | 10(6.2) | 18(11.2) | 28(17.4) |
| 2+ | 17(10.6) | 30(18.6) | 47(29.2) | 2500-4000(normal) | 43(26.7) | 73(45.3) | 116(72.0) |
| 3+ | 12(7.5) | 23(14.3) | 35(21.7) | >4000(high) | 6(3.7) | 4(2.5) | 10(6.2) |
| 4+ | 6(3.7) | 10(6.2) | 16(9.9) | Data unavailable | 3(1.9) | 4(2.5) | 7(4.3) |
| 5+ | 3(1.9) | 5(3.1) | 8(5.0) | Total | 62(38.5) | 99(61.5) | 161(100) |
| Total | 62(38.5) | 99(61.5) | 161(100) |
Table 2: Distribution of PPD among patients attending primary care facilities by age, ethnicity, anaemia, marital status, employment, gestation diabetes and contraceptive use.
The combined effect of several variables related to PPD (ethnicity, employment, marital status, gravidity, use of contraceptives and complications of pregnancy) was investigated using logistic regression analysis. We found no association between PD and ethnicity (OR=0.871; 95% CI 0.697-1.090; p=0.048), employment (OR=0.766; 95% CI 0.525-1.120; p=0.169), marital status (OR=0.913; 95% CI 0.779-1.070; p=0.261), gravidity (OR=0.995; 95% CI 0.895- 1.105; p=0.921), use of contraceptives (OR=1.102; 95% CI 0.629- 1.932; p=0.474) or complications during pregnancy (OR=0.761; 95% CI 0.360-1.607; p=0.474).
Using ARC GIS we mapped all cases of PPD, fig 3. In this instance we used the population of childbearing women age 15-45 years as the denominator to estimate the prevalence of PPD by community. The highest prevalence of PPD (>57%) occurred in urban areas (Arima, Mt Hope Chaguanas and Cunupia). We report a sensitivity and specificity of 0.98 and .80 and a Cronbach’s α of 0.8.
Discussion
An important finding of the study is the estimated point prevalence of PPD is 38.5% (95% CI 31.0-46.5). A similar study in Jamaica reported a prevalence of 47.7% and concluded that the prevalence of postpartum depressive symptoms in the Jamaican population of postpartum women was higher than previous estimates and higher than the World Health Organization estimates of 2015 [45]. Other studies show a varying pattern of PPD both among developed and developing countries such as Nepal 4.9%, Hungary 10.8, Guyana 50.0, Barbados 16%, Brazil 24.1% and Australia 11.2% [42]. Hence we conclude that the prevalence of PPD in TTO is high for a country with a high GNI per capita. Thus, underscoring the need for the detection and treatment PPD in the delivery of perinatal care is in accordance with SDG. Consequently we strongly recommend that structured programs to detect and treat depression during pregnancy and especially postpartum form part of the overall care and support for all women during childbearing.
Currently all pregnant women are screened for anaemia, gestational diabetes (GDM), HIV, hypertension, syphilis and sickle cell anaemia, in accordance with the Maternal and Child Health Manual 2015 of the Ministry of Health and PAHO. In addition preeclampsia toxaemia of pregnancy and other maternal and foetal abnormalities are routinely screened using laboratory and ultrasonography during the antenatal period. However there is no screening for depression. Further Clapperton et al in 2009 reported the incidence of GDM as 4.31% (95% C.I. 2.31%, 6.31%) [46]. In a recent study Mungrue reported the prevalence of HIV positive mothers in Trinidad in a primary care setting was 1.6% [47]. In regard to anaemia, Uche-Nwachi et al found that the prevalence of anaemia in pregnant women was 15.3% (95% CI 13.4%, 16.6%) [48]. In Trinidad among 46 381 deliveries over a 10-year study period, only 102 patients (0.2%) had early-onset severe preeclampsia [49]. Also10% of women have high blood pressure during pregnancy, and preeclampsia complicates 2% to 8% of pregnancies [50]. Although the early detection and management of all these conditions are necessary we provide evidence that depression has a higher prevalence yet it is not part of the routine assessment of mothers especially in the vulnerable postpartum period. Therefore we strongly recommend interventions to detect and manage depression to improve the mental health of mothers. This is supported by considerable evidence from high-income countries of the consequences of prenatal maternal depression and other forms of stress associated with a range of adverse mental health outcomes for the child, including an increased risk of anxiety, depression, attention deficit hyperactivity disorder, and conduct disorder [51].
We found that younger women between the ages 15-20 and 21-25 had the highest prevalence of depression both among prenatal (60.9%) and postnatal women (54.6%). Melville and colleagues also showed that as age increases, the prevalence of PD depression decreases, [52]. Similarly Falci and colleagues showed that parent females have higher levels of depressive symptoms (12.84) in young adulthood compared to later parent females (10.63, p<.01) or non-parent females (10.37, p < 0.001) which was explained by lower levels of personal control and heightened exposure to financial strain [53]. Troutman, et al. showed that adolescent childbearing mothers (ages 14 to 18) showed similar rates of depression to non-childbearing adolescents of the same age group [54]. In another study from Portugal, it was found that adolescent mothers presented more depressive symptoms as well as more EPDS>12 scores than adult mothers, both in pregnancy (25.9% versus 11.1%) and in the postpartum period (25.9% versus 9.3%) [55]. Further analysis of PHQ-9 scores, showed that scores of 5-9 for prenatal patients (34.9%) was significantly higher (p<0.05) when compared to that of postnatal (21.2%). Sidebottom, et al. demonstrated similar finding in which depression in the prenatal period measured using the PHQ-9 questionnaire was 15% compared to 6% in the postpartum period [56].This observed difference can be accounted for by the fact that depression in early pregnancy is determined mainly by psychosocial factors [57,58]. These include unwanted pregnancies which occur in approximately 60% of pregnancies in Trinidad [59]. In addition poor maternal care, higher public self consciousness, high paternal overprotection especially common among the East Indian diaspora, poor intimacy by the husband and having been remarried all common in this setting maybe other factors contributing to this phenomenon.
We explored the association between anaemia a common condition in pregnancy and MD, and found no significant association (p>0.05), a finding consistent with others [60]. The prevalence of newly acquired GD in this study was 8% (48/602). This comprised of 31 of the 441 prenatal patients and 17 of the 161 postnatal patients. GD did not confer a high risk of depression in prenatal and postpartem women (OR<1, p>0.05). This is inconsistent with findings reported elsewhere in which MD was at least twice times more common in patients with GD [61]. However, a study in Chicago, Illinois concluded that there were similar rates of MD in patients with GD and than those without [62]. More importantly the prevalence of GD has approximately doubled over the 10-year period 2007-2016. Clapperton, et al. reported a prevalence of 4.1% in 2005-2007 [46] as compared to 8% of that reported in this study. This phenomenon is being reported across diverse populations. Its implications as a contributor to maternal and neonatal morbidity and mortality, is an emerging challenge for developing countries [63,64].
There was no association between employment status (χ2, p>0.05) and MD. A systematic review reported that unemployment was not significantly associated with depressive symptoms [65]. Also there was no ethnic disparity in the occurrence of MD. PD was marginally higher in East Indians (50.7%) as compared to Africans (46.7%) however this difference was not significant (p>0.05). Although high rates of depression have been recorded among African Americans [68,69]. Being married or in a stable partner relationship (common Law) was protective of MD, this finding was also demonstrated by Yim, et al. [66]. This may be attributed to better social and emotional support. Further Akincigil et al found that that married women had lower rates of PPD in comparison with cohabiting but unmarried women, who in turn, had lower rates of PPD than did women who were non-cohabiting [67].
Our study reported no significant relationship bewtween parity and gaeravididity and MD. Ji et al using four depression scales (EDPS, self-rated BDI and a 17 item and 21 item Hamilton Rating Scale for Depression (HRSD17) (HRSD21)), and across all pregnancy stages, found that gravidity status had no discernible impact of the global performance of the scales [68].
Women who experienced complications of pregnancy had a lower prevalence of PD (38.2%) than those without complications (50.6%). This finding supports the argument by Cox et al that depression may be substantially higher among postpartem women due to psychological and physiological stressful events such as labour and delivery [69]. Our study showed 60% of women with infants >4000g, that is a high birth weight, had PPD. Anderssonet al. reported in 2004 a borderline-significant bivariate association between antenatal depressive disorder and increased birth weight (birth weight <2,500 g: OR=1.20 (95 percent CI: 0.41, 3.48); birth weight ≥ 4,000 g, OR=1.45 (95% CI: 1.00, 2.10) [70].
In this study, we analyzed, for the first time in Trinidad, the spatial distribution of prevalent cases of PPD. The main finding of this analysis showed the distribution of cases of PPD was higher in urban areas than rural areas. Urban dwellers often face higher rates of crime, an adverse social environment (such as inequality and isolation), low social cohesion (that is, a lack of closeness and supportiveness between neighbors), poor housing and physical stressors (such as pollution and noise) all contributing to poor mental health all of which are common in this setting [71]. Therefore understanding demographic trends and mechanisms of PPD within these urban areas is important to developing and targeting future prevention efforts.
The major limitation of this study was the use of the PHQ-9 could overestimate the prevalence of depression through the somatic symptoms which can exist normally during pregnancy. Moreover, the instrument has not been locally validated. A strength of the study was it population based and thus more representative of the population.
In conclusion this study provides evidence that MD is common in the developing world, detection and treatment therefore must be a priority as children born to mothers with depression have more behavioral problems, more psychiatric illness, more visits to pediatricians, lower IQ scores, and attachment issues.
References
- The World Bank (2005) World development indicators.
- Hendrick V (1998) Evaluation of mental health and depression during pregnancy. Psychopharmacol Bull 34: 297-299.
- Stern G, Kruckman L (1983) Multi-disciplinary perspectives on post-partum depression: an anthropological critique. Soc Sci Med 17: 1027-1041.
- Essential Medicines and Health Products Information Portal (2011) The global economic burden of non-communicable diseases. World Economic Forum, Geneva, Switzerland.
- Hu TW (2006) Perspectives: an international review of the national cost estimates of mental illness, 1990-2003. J Ment Health Policy Econ 9: 3-13.
- United Nations Organization (2015) Transforming our world: the 2030 agenda for sustainable development. New York, USA.
- Davalos DB, Yadon CA, Tregellas HC (2012) Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch Women’s Ment Health 15: 1-14.
- Mautner E, Greimel E, Trutnovsky G, Daghofer F, Egger JW, et al. (2009) Quality of life outcomes in pregnancy and postpartum complicated by hypertensive disorders, gestational diabetes, and preterm birth. J Psychosom Obstet Gynaecol 30: 231-237.
- Katon JG, Russo J, Gavin AR, Melville JL, Katon WJ (2011) Diabetes and depression in pregnancy: is there an association? J Womens Health (Larchmt) 20: 983-989.
- Delahaije DH, Dirksen CD, Peeters LL, Smits LJ (2013) Anxiety and depression following preeclampsia or HELLP syndrome: a systematic review. Acta Obstet Gynecol Scand. 92: 746-761.
- O’Higgins M, Roberts IS, Glover V, Taylor A (2013) Mother-child bonding at 1 year; associations with symptoms of postnatal depression and bonding in the first few weeks. Arch Women’s Ment Health 16:381-389.
- Hatton DC, Harrison-Hohner J, Coste S, Dorato V, Curet LB, et al. (2005) Symptoms of postpartum depression and breastfeeding. J Hum Lact 21:444-449.
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, et al. (2005) Perinatal depression: a systematic review of prevalence and incidence. Obset Gynecol 106: 1071-1083.
- Chaudron LH, Klein MH, Remington P, Palta M, Allen C, et al. (2001) Predictors, prodromes and incidence of postpartum depression. J Psychosom Obstet Gynaecol 22: 103-112.
- Orr ST, Blazer DG, Orr CA (2012) Maternal prenatal depressive symptoms, nicotine addiction, and smoking-related knowledge, attitudes, beliefs, and behaviors. Matern Child Health J 16: 973-978.
- Flynn HA, Chermack ST (2008) Prenatal alcohol use: the role of lifetime problems with alcohol,drugs, depression, and violence. J Stud Alcohol Drugs 69: 500-509.
- Bodnar LM, Wisner KL, Moses-Kolko E, Sit DK, Hanusa BH (2009) Prepregnancy body mass index, gestational weight gain, and the likelihood of major depressive disorder during pregnancy. J Clin Psychiatry 70: 1290-1296.
- Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, et al. (2009) The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet Gynecol 114: 703-713.
- Han A, Stewart DE (2014) Maternal and fetal outcomes of intimate partner violence associated with pregnancy in the Latin American and Caribbean region. Int J associated with pregnancy in the Latin American and Caribbean region. Int J Gynecol Obstet 124: 6-11.
- McFarland J, Salisbury AL, Battler CL, Hawes K, Halloran K, et al. (2011) Major depressive disorder during pregnancy and emotional attachment to the fetus. Arch Womens Ment Health. 14: 425-434.
- Suri R, Altshuler LA, Mintz J (2004) Depression and the decision to abort. Am J Psychiatry. 161: 1502.
- Murray L, Cooper PJ (1997) Postpartum depression and child development. Psychol Med. 27: 253-260.
- Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, et al. (2010) Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 202: 5-14.
- Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, et al. (2000) Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry 157: 924-930.
- Grace SL, Evindar A, Stewart DE (2003) The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of the literature. Arch Women’s Ment Health 6: 263-274.
- Dennis CL, Ross L (2005) Relationships among infant sleep patterns, maternal fatigue, and development of depressive symptomatology. Birth 32: 187-193.
- Ip S, Chung M, Raman G, Chew P, Magula N, et al. (2007) Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep) 153: 1-186.
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, et al. (2011) Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev 14: 1-27.
- Chisholm D, Saxena S (2012) Cost effectiveness of strategies to combat neuropsychiatric conditions in sub-Saharan Africa and South East Asia: mathematical modelling study. BMJ 344: e609.
- Weobong B, Asbroek AHA, Soremekun S, Manu AA, Owusu-Agyei S, et al. (2014) Association of antenatal depression with adverse consequences for the mother and newborn in rural Ghana: Findings from the DON population-based cohort study. PLoS One 9: e116333.
- Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, et al. (2013) Mother-infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Arch Women’s Ment Health 16: 29-38.
- Farr SL, Dietz PM, Rizzo JH, Vesco KK, Callaghan WM, et al. (2013) Health care utilisation in the first year of life among infants of mothers with perinatal depression or anxiety. Paediatr Perinat Epidemiol 27: 81-88.
- Workman JL, Barha CK, Galea LAM (2012) Endocrine substrates of cognitive and affective changes during pregnancy and postpartum. Behav Neurosci 126: 54-72.
- Hyman S, Chisholm D, Kessler R, Patel V, Whiteford H (2006) Mental disorders. Disease control priorities in developing countries, World Bank Publications, London, UK.
- O’Connor E, Rossom RC, Henniger M, Groom HC, Burda BU (2016) Primary care screening for and treatment of depression in pregnant and postpartum women: evidence report and systematic review for the US Preventive Services Task Force. JAMA 315: 388-406.
- Committee on Obstetric Practice (2015) The American College of Obstetricians and Gynecologists Committee Opinion no. 630. Screening for perinatal depression. Obstet Gynecol 125: 1268-1271.
- Earls MF (2010) Committee on psychosocial aspects of child and family health American academy of pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics 126: 1032-1039.
- Macaulay S, Dunger DB, Norris SA (2014) Gestational diabetes mellitus in Africa: a systematic review. PLoS One 9: e97871.
- Chisholm D, Lund C, Saxena S (2007) Cost of scaling up mental healthcare in low and middle-income countries. Br J Psychiatry 191: 528-535.
- Chisholm D, Burman-Roy S, Fekadu A, Kathree T, Kizza D, et al. (2016) Estimating the cost of implementing district mental healthcare plans in five low- and middle-income countries: the PRIME study. Br J Psychiatry 208: s71-s78
- Kroenke K, Spitzer R, Williams W (2001) The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 16: 606-616.
- Shury A, Harris M (2016) Risk factors for postpartum depression among women attending postnatal clinics in Kingston, Jamaica. West Indian Med J 65: 25.
- Parsons C, Young K, Rochat T, Kringelbach M, Stein A (2011) Postnatal depression and its effects on child development: a review of evidence from low and middle income countries. Br Med Bull 101: 57-79.
- Clapperton M, Jarvis J, Mungrue K (2009) Is gestational diabetes mellitus an important contributor to metabolic disorders in Trinidad and Tobago? Obstet Gynecol Int 289329: 6.
- Mungrue K (2016) Monitoring the effectiveness of prevention of mother-to-child (MTCT) HIV transmission in Trinidad a small middle income country, 2013-2016. Journal of Prevention & Treatment of HIV/AIDS 2: 1-4.
- Uche-nwachi EO, Odekunle A, Jacinto S, Burnett M, Clapperton M, et al. (2010) Anaemia in pregnancy: associations with parity, abortions and child spacing in primary healthcare clinic attendees in Trinidad and Tobago. Afr Health Sci 10: 66-70.
- Perinatol S (2009) The global impact of pre-eclampsia and eclampsia. Semin Perinatol 33: 130-137.
- Bassaw B, Khan A, Ramjohn M, Ramoutar V, Bassawh L (2012) Pregnancy outcome in early- onset severe pre-clampsia in Trinidad. Int J Gynaecol Obstet 116: 78-80.
- Falci CD, Mortimer JT, Noel HJ (2010) Parental timing and depressive symptoms in early adulthood. Adv Life Course Res 15: 1-10.
- Troutman BR, Cutrona CE (1990) Nonpsychotic postpartum depression among adolescent mothers. J Abnorm Psychol 99: 69-78.
- Figueiredo B, Pacheco A, Costa R (2007) Depression during pregnancy and the postpartum period in adolescent and adult Portuguese mothers. Arch Womens Ment Health 10: 103-109.
- Sidebottom AC, Hellerstedt WL, Harrison PA, Hennrikus D (2014) An examination of prenatal and postpartum depressive symptoms among women served by urban community health centers. Arch Womens Ment Health 17: 27-40.
- Kitamura T, Shima S, Sugawara M, Toda MA, Shima S (1991) Stress and puerperal psychosis. Br J Psychiatry 158: 290-291.
- Mungrue K, Boodo S (2017) The use of oral and emergency contraception in women: Understanding the maternal contribution to survival convergence. Int J Child Health and Hum Dev 10: 1-11.
- Harris B, Othman S, Davies JA, Weppner GJ, Richards CJ, et al. (1992) Association between postpartum thyroid antibodies and depression. BMJ 305: 152-156.
- Armony-Sivan R, Shao J, Li M, Zhao G, Zhao Z, et al. (2012) No relationship between maternal iron status and postpartum depression in two samples in China. J Pregnancy 521431.
- Kozhimannil KB, Pereira MA, Harlow BL (2009) Association between diabetes and perinatal depression among low-income mothers. JAMA 301: 842-847.
- Byrn M, Penckofer J (2015) The relationship between gestational diabetes and antenatal depression. J Obstet Gynecol Neonatal Nurs 44: 246-255.
- Albrecht SS, Kuklina EV, Bansil P, Jamieson DJ, Whiteman MK, et al. (2010) Diabetes trends among delivery hospitalizations in the U.S., 1994-2004. Diabetes Care 33: 768-773.
- Sella T, Shalev V, Elchalal U, Chovel-Sella A, Chodick G (2013) Screening for gestational diabetes in the 21st century: a population-based cohort study in Israel. J Matern Fetal Neonatal Med 26: 412-416.
- Zhang F, Dong L, Zhang CP, Li B, Wen J, et al. (2011) Increasing prevalence of gestational diabetes mellitus in Chinese women from 1999 to 2008. Diabet Med 28: 652-657.
- Miller ES, Peri MR, Gossett DR (2016) The association between diabetes and postpartum depression. Arch Womens Ment Health 19: 183-186.
- Gavin AR, Melville JL, Rue R, Guo Y, Dina KT, et al. (2011) Racial differences in the prevalence of antenatal depression. Gen Hosp Psychiatry 33: 87.
- Yim IS, Stapleton TL, Guardino C, Hahn-Holbrook J, Dunkel Schetter C (2015) Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol 11: 99-137.
- Akincigil A, Munch S, Niemczyk K (2010) Predictors of maternal depression in the first year postpartum: marital status and mediating role of relationship quality. Soc Work Health Care 49: 227-244.
- Ji S, Long Q, Newport J, Na H, Knight B, et al. (2011) Validity of depression rating scales during pregnancy and the postpartum period: Impact of trimester and parity. J Psychiatr Res 45: 213-219.
- Cox J, Murray D, Chapman G (1993) A controlled study of the onset, duration and prevalence of postnatal depression. Br J Psychiatry 163: 27-31.
- Andersson L, Sundström-Poromaa I, Wulff M, Åström M, Bixo M (2004) Neonatal outcome following maternal antenatal depression and anxiety: a population-based study. Am J Epidemiol 159: 872-881.
- Hayes LJ, Goodman SH, Carlson E (2013) Maternal antenatal depression and infant disorganized attachment at 12 months. Attach Hum Dev 15: 133-153.
- March D, Hatch SL, Morgan C, Kirkbride JB, Bresnahan M, et al. (2008) Psychosis and place. Epidemiol Rev 30: 84-100.
- Field T (2011) Prenatal depression effects on early development: a review. Infant Behav Dev 34: 1-14.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi