Research Article, J Womens Health Vol: 14 Issue: 3
The Psychosocial Impact of Infertility Due to Endometriosis: A Narrative Synthesis of Dimensions, Effects, and Pathways to Resilience
Temitope O. Labinjo*
Department of Primary Care and Mental Health, Institute of Population Health, University of Liverpool, Liverpool, United Kingdom
- *Corresponding Author:
- Temitope O. Labinjo
Department of Primary Care and Mental Health,
Institute of Population Health, University of Liverpool,
Liverpool,
United Kingdom,
Email: Temitope.Labinjo@liverpool.ac.uk
Received date: 12 July, 2025, Manuscript No. JWHIC-25-167826;
Editor assigned date: 14 July, 2025, PreQC No. JWHIC-25-167826 (PQ);
Reviewed date: 28 July, 2025, QC No. JWHIC-25-167826;
Revised date: 17 September, 2025, Manuscript No. JWHIC-25-167826 (R);
Published date: 23 September, 2025, DOI: 10.4172/2325-9795.1000546
Citation: Labinjo TO (2025) The Psychosocial Impact of Infertility Due to Endometriosis: A Narrative Synthesis of Dimensions, Effects, and Pathways to Resilience. J Womens Health 14:3.
Abstract
Endometriosis, a chronic gynaecological condition affecting up to 10% of women of reproductive age worldwide, is a significant cause of infertility with profound emotional and social consequences that are often overlooked. This narrative synthesis analyses the psychosocial effects of infertility caused by endometriosis on women's mental health, self-identity, interpersonal connections, social life, and financial stability. Using a biopsychosocial framework, it synthesises quantitative and qualitative studies published between 2004 and 2024 to reveal how women cope with anxiety, depression, stigma, and financial difficulties, while also demonstrating resilience through support networks, therapy, faith, and reframed life goals.
Keywords: Endometriosis, Infertility, Psychosocial impact, Biopsychosocial model
Introduction
Endometriosis is not merely a medical diagnosis but a condition that profoundly alters daily life and long-term aspirations [1-16]. It induces pelvic pain, dysmenorrhea, dyspareunia, and, for numerous individuals, infertility due to the proliferation of tissue resembling endometrial tissue outside the uterus. Approximately 10% of women of reproductive age globally are affected with endometriosis [16,8]. As many as fifty percent may experience difficulties conceiving [14]. The physiological associations between endometriosis and infertility are widely recognised, although the emotional and social ramifications are often overlooked in clinical discussions. Infertility can lead to numerous mental health issues, including depression, anxiety, and feelings of inadequacy [9].
Infertility constitutes a significant strain to endure. Individuals experiencing infertility frequently endure negative self-perceptions, resulting in feelings of grief, worry, and isolation [9]. However, when infertility is coupled with endometriosis, which induces chronic pain, persistent fatigue, and intermittent flare-ups, the mental burden can be significantly exacerbated. It transforms into a multifaceted struggle that influences nearly every aspect of a woman's existence. To enhance care, it is essential to thoroughly understand these interrelated difficulties.
Research has demonstrated the prevalence of psychological discomfort among women with endometriosis. Research from an Indian reproductive clinic indicated that women with both endometriosis and infertility exhibited significantly higher rates of anxiety (42%) and depression (40%) compared to those with infertility alone [12]. Research indicates elevated rates of sadness (up to 86%) and substantial anxiety (about 29%) in women diagnosed with endometriosis [4]. Qualitative stories enhance these statistics, illustrating profound experiences of recurrent bereavement, diminished confidence, and social disengagement [2,5].
It is not solely the condition that inflict pain; it is the recurring cycles of optimism and despair that individuals experience daily. Each month may herald new optimism, yet it invariably culminates in the melancholy of yet another unsuccessful endeavour. The recurrent losses may resemble the enduring grief associated with chronic bereavement [2].
In numerous cultures especially in Africa, motherhood is essential to a woman's identity, her familial duty, and her marital relationship [5]. Individuals experiencing infertility frequently grapple with feelings of guilt, shame, or fear around the potential departure of their partner. Many avoid baby showers, christenings, or other child-centric celebrations due to the stigma associated with childlessness. This is when assistance is most crucial [11].
This conflict often occurs in the bedroom as well. The pain associated with endometriosis and the need to engage in sexual activity at specific times can transform intimacy into an experience characterised by obligation or suffering rather than connection. Such emotions can jeopardise closeness and potentially incite conflicts [3]. Although experiencing feelings of helplessness or stress, spouses seldom engage in discussions regarding their own issues. Endometriosis not only induces discomfort during sexual intercourse (dyspareunia) but also complicates intimacy [3].
Infertility resulting from endometriosis incurs significant workplace and economic consequences, including emotional repercussions. Numerous women postpone career aspirations or reduce professional engagement in anticipation of parenthood. The unpredictability of pain and frequent medical appointments can result in absenteeism, diminished productivity, or alterations in employment status. Compounding these challenges are the substantial financial burdens associated with fertility treatment, which accumulate over time [7,13].
Nevertheless, amidst these genuine adversities, numerous women exhibit remarkable resilience. They derive strength from participating in support groups, pursuing counselling or mindfulness therapy, relying on their faith, or redefining their aspirations through adoption or opting for a child-free lifestyle, thereby uncovering alternative avenues to infuse meaning and joy into their lives [9]. Acknowledging this, an increasing number of experts advocate for healthcare that extends beyond merely addressing physical symptoms. They promote care teams that incorporate gynaecologic, fertility, pain, and mental health support, delivering genuinely holistic care [1].
This study presents a narrative synthesis of the psychosocial effects of endometriosis-related infertility, structured through the biopsychosocial model to illustrate the interplay between biological disease mechanisms, significant psychological distress, and intricate social difficulties. Although endometriosis is a widespread disorder and a primary contributor to infertility, its multifaceted effects on mental health, identity, relationships, and professional life are little examined and frequently neglected in clinical treatment.
Materials and Methods
A narrative synthesis was conducted to elucidate women's lived experiences beyond clinical symptoms. Searches were performed in PubMed, Scopus, and Google Scholar using keywords such as 'endometriosis,' 'infertility,' 'psychological impact,' 'social stigma,' and 'coping.' Studies published between 2004 and 2024 that examined psychological, social, or economic effects on women with endometriosis-related infertility were included. Quantitative, qualitative, and mixed-method designs were considered. Findings were systematically categorised into psychological health, self-concept, social connections, partner relationships, employment and finances, and coping mechanisms.
This synthesis was conceptually guided by the biopsychosocial model [6], which recognises that health outcomes are shaped by the interplay of biological causes, psychological responses, and social circumstances. This methodology provided a framework to categorise and examine the complex impacts of infertility linked to endometriosis as recorded in the literature.
Results
Nine (9) peer-reviewed studies met the criteria. The reviewed studies encompassed mixed-method analyses, quantitative surveys, and qualitative interviews published between 2004 and 2024. These studies were chosen for their analysis of the psychological, social, or economic effects of endometriosis in women facing infertility. Standardised instruments, like the Hospital Anxiety and Depression Scale (HADS) and FertiQoL, were utilised in the majority of quantitative studies to record the prevalence rates of anxiety, depression, and reduced quality of life.
Substantial insights into the impact of endometriosis-induced infertility on individuals' self-perception, interpersonal connections, and social interactions were acquired through qualitative and mixedmethod research. This comprehensive literature demonstrates the illness's intricate effects on individuals, highlighting culturally pertinent issues such as emotional distress, interpersonal conflict, stigma, and professional obstacles. The objectives of this narrative synthesis were fulfilled, as a comprehensive portrayal of the psychological impact was provided through the amalgamation of quantitative prevalence data and intricate human accounts.
Women’s narratives and research outcomes consistently demonstrate a significant, complex burden. Women with endometriosis usually experience chronic pelvic pain, dysmenorrhea, dyspareunia, and anatomical alterations that complicate conception [8,14,15].
The monthly cycles of optimism and disappointment associated with treatment exacerbate sadness. The condition frequently undermines self-esteem, causing women to feel inadequate or diminished, particularly in cultures where motherhood dictates status [5].
Socially, many isolate themselves from friends and family events, especially those commemorating pregnancy or children, to protect themselves from distressing reminders [11]. Intimate relationships frequently endure hardships: sexual discomfort and the emotional burden of scheduled intercourse can hinder intimacy, while recurrent disappointments weaken connections [3]. Partners may also contend with feelings of powerlessness and distress, but their experiences are less frequently examined.
The financial and occupational landscape is also tough. Chronic discomfort and frequent medical appointments result in absenteeism and reduced productivity, while ongoing treatments deplete financial resources [13].
Despite these adversities, numerous women forge avenues to recovery, relying on peer networks, therapy, spirituality, or redefining aspirations beyond biological motherhood [1,9,10].
A theoretical framework for the psychosocial burden
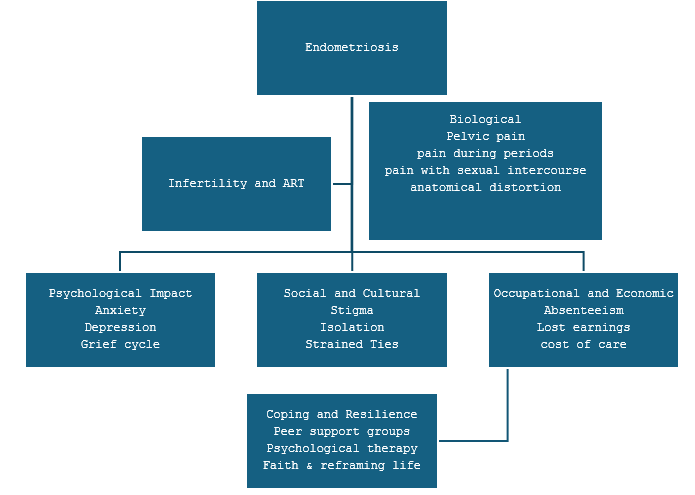
This framework physically delineates the impact of endometriosis and infertility on a woman's life, encompassing acute psychological repercussions (anxiety, despair, bereavement), strained social relationships and intimate connections, as well as financial and occupational instability. This concept is founded on coping techniques and resilience, bolstered by networks, counselling, spirituality, and reimagined futures that mitigate and occasionally transform these impacts (Figure 1).
Figure 1: Conceptual framework illustrating the domains of psychosocial impact-biological, psychological, social, occupational, and resilience pathways of endometriosis-related infertility.
Discussion
Women experiencing infertility due to endometriosis endure a significant, complex emotional cost that transcends mere medical symptoms. They often endure elevated levels of anxiety, despair, and recurring grief, coupled with a compromised sense of self-worth and identity linked to cultural expectations of parenting [4,5]. Numerous individuals retreat socially to evade shame or distressing reminders, while close relationships frequently deteriorate due to sexual discomfort, emotional turmoil, and financial burdens from continuous treatments [3,11]. Occupational issues, such as absenteeism and diminished productivity, exacerbate the economic burden. Many women exhibit notable resilience, seeking support through therapy, faith, peer groups, and by redefining life objectives beyond biological children [1,9,10]. Collectively, these findings highlight the pressing necessity for comprehensive, compassionate care that considers the psychological, social, and cultural aspects of infertility associated with endometriosis.
This study's conceptual framework demonstrates how endometriosis and its related infertility serve as fundamental catalysts that influence various interconnected psychosocial domains. Chronic pelvic pain, coupled with uncertainty and recurrent fertility setbacks, results in significantly increased rates of anxiety, depression, and cyclical grieving [4,13]. The paradigm illustrates a pathway that connects "Endometriosis" and "Infertility and ART" directly to the biological and psychological domains, highlighting the immediate and significant mental health costs that frequently arise (Table 1) [2].
| Domain | Specific impacts | Key references |
| Psychological health | Anxiety, depression, grief cycles, and catastrophizing | del Pino-Sedeño et al. [2,4] |
| Self-concept and identity | Feelings of inadequacy, guilt, and threatened femininity. | Dyer et al.; de Graaff et al. [3,5] |
| Social relationships | Isolation, avoidance of child-focused events, diminished support | Lindsey and Driskill; Fourquet et al. [7,11] |
| Partner relationships | Reduced intimacy, sexual dysfunction, partner distress | de Graaff et al. [3] |
| Occupational and economic | Absenteeism, productivity loss, and high ART costs | Simoens et al.; Fourquet et al. [14,7] |
| Coping and adaptation | Peer support, therapy, and reframing life goals | Greil et al.; As-Sanie et al.; Labinjo [1,9,10] |
Table 1: Overview of psychosocial domains impacted by endometriosis-related infertility.
The social and cultural realm illustrates how these psychological challenges are exacerbated by societal expectations that closely associate womanhood with parenting. Infertility jeopardises selfidentity and engenders stigma in several circumstances [5]. Women may disengage from social networks, eschew baby showers or family gatherings, and endure heightened isolation [9], so reinforcing the junction within the framework of internal suffering and external social demands. The strain in partner relationships illustrated in the framework indicates that sexual pain (dyspareunia), coupled with the emotional burdens of infertility treatments, often diminishes intimacy, decreases sexual satisfaction, and generates tension within relationships [3,14].
The framework's occupational and economic area acknowledges the concrete impacts of endometriosis on professional lives. Research indicates heightened absenteeism, diminished job productivity, and, in certain instances, career modifications or losses, coupled with substantial financial burdens from recurrent surgeries and fertility treatments [7,13]. By positioning these alongside the psychological and social ramifications, the framework demonstrates how the disease's burden transcends the individual's internal experience, influencing overall life stability.
The framework ultimately results in a domain for coping and resilience, acting as a vital modifying layer. Despite considerable obstacles, several women participate in peer support and psychiatric counselling, actively reconstructing their life narratives beyond biological motherhood, which can alleviate anguish and cultivate a revitalised sense of purpose [1,9]. This is depicted in the model as a downstream process leading to “Coping and Resilience,” emphasising adaptive capacities that might alleviate potential cascading psychosocial damages.
The conceptual framework established herein elucidates the progression of these conflicts. The initial repercussions of endometriosis include infertility, chronic discomfort, uncertainty, and recurrent disappointments, which contribute to emotional anguish [2-4]. The consequences extend outward from that point. Societal expectations for childbirth can transform personal suffering into public disgrace, compelling women to shun social gatherings and exacerbating their isolation [5].
The concept also emphasises how intimacy is frequently undermined. The interplay of sexual pain and the mental burden of infertility might reduce enjoyment and foster estrangement between spouses [3,14].
The occupational and financial aspect of the framework demonstrates how recurrent surgeries, continuous treatments, and persistent symptoms interfere with professional lives, resulting in absenteeism, diminished income, and challenging career decisions [7,13].
This framework does not conclude with burdens. It concludes with a domain focused on coping and resilience. Numerous women proactively reconstruct their narratives, pursue counselling, rely on peer networks, or derive comfort from spiritual beliefs. Although these tactics do not eradicate the obstacles, they can alleviate their effects and foster new opportunities for significance and connection [1,9].
This conceptual framework visually and logically integrates the core drivers of endometriosis and infertility across various life domains, highlighting the need for holistic, multidisciplinary care that concurrently addresses mental health, social identity, relational dynamics, economic support, and resilience-building strategies. The synthesis of the evidence elucidates the extensive and interrelated nature of these impacts.
Alignment of domains with the biopsychosocial model
The biopsychosocial paradigm [6] illustrates that infertility associated with endometriosis impacts more than just the physical body. It depicts a complex scenario where biological, psychological, and social factors are intricately interconnected in women's everyday experiences (Table 3).
Endometriosis is a chronic inflammatory condition characterised by the proliferation of tissue analogous to the uterine lining outside the uterus. This results in chronic pain during menstruation, sexual intercourse, and routine activities [8,16]. These physical symptoms are not merely inconvenient; they obstruct fundamental life objectives, complicate conception, and often necessitate repeated medical interventions, surgeries, and hormone therapies for women [15]. The body emerges as a source of instability and unpredictability, solidifying their challenges inside the biological realm (Table 2).
| Study | Population | Key findings on psychological impact |
| de Graaff et al. [3] | 1,418 women, global survey | Significant deterioration in social and emotional well-being |
| Simoens et al. [14] | Economic model | Reduced HRQoL and increased indirect costs in endometriosis |
Table 2: Summary of psychological impacts in women with endometriosis-related infertility.
The psychological world transcends the corporeal narrative. Significant emotional distress arose from enduring chronic pain and again confronting the same disappointments, such as monthly pregnancy tests yielding same results. Research indicates that women with endometriosis encounter anxiety and depression. This transcends mere numerical values; it pertains to surmounting fear, pain, and the scepticism of one's own worth. it was found that women with endometriosis exhibit considerable resilience by engaging in treatment, reassessing their objectives, or surrounding themselves with helpful others [9].
In the social sphere, endometriosis and infertility modify women's engagement with their environment. Some cultures perceive motherhood as a significant rite of passage, and infertility can lead women to experience profound self-doubt, strain their marriages, and foster feelings of inadequacy [3,5]. Numerous individuals abstain from family gatherings or baby showers to evade well-meaning but painful inquiries. Moreover, abrupt exacerbations or prolonged fertility treatments can complicate employment retention or acquisition [14]. These examples illustrate how social norms, cultural narratives, and economic conditions can all affect an individual's health (Table 3).
| Domain | Key findings and references |
| Biological dimension | Chronic pelvic pain, menstrual irregularities, dyspareunia, anatomical disruption [8,16] |
| Compromised fertility requiring surgeries and ART [15] | |
| Psychological dimension | Elevated anxiety, depression, grief, self-worth issues; depression up to 86% [2] |
| Coping via therapy, support groups, cognitive reframing [9] | |
| Social dimension | Stigma around menstruation and infertility, fears of marital instability [3,5] |
| Occupational disruptions: Absenteeism, reduced productivity, ART costs [14] |
Table 3: Mapping the psychosocial impacts of endometriosis-related infertility onto the biopsychosocial model.
Examining endometriosis-related infertility via a biopsychosocial lens demonstrates that it transcends mere medical concerns; it is a deeply personal experience that affects both psychological well-being and social dynamics. This underscores the significance of delivering care that goes beyond mere physical healing. Addressing women's needs necessitates psychological support and societal understanding. Comprehensive supportive care must be holistic, encompassing mental health, social identity, relationships, economic circumstances, and methods of fostering resilience. Only then can care teams aspire to engage women in their current circumstances and assist them in constructing fulfilling lives, regardless of the pathways they choose.
Conclusion
The convergence of endometriosis and infertility constitutes a distinct biopsychosocial burden marked by increased anxiety, sadness, social isolation, strained relationships, and vocational disruption. Due to the widespread and complex effects, there is an urgent necessity for thorough care pathways that integrate mental health assessments and customised biopsychosocial therapies with medical treatment.
By explicitly situating these experiences within a biopsychosocial framework, the synthesis underscores the necessity for comprehensive care strategies that extend beyond the mere treatment of physical symptoms. This study possesses global significance due to the widespread impact of endometriosis across many healthcare systems and cultural contexts, and it presents multidisciplinary interest by integrating perspectives from public health, reproductive medicine, psychology, sociology, and health services research. These viewpoints are crucial for promoting comprehensive care models that genuinely reflect the experiences of women facing endometriosis-related infertility globally.
Infertility associated with endometriosis permeates all aspects of a woman's existence, encompassing her mental health, identity, relationships, career, and aspirations. This highlights the necessity for health services to address more than the illness, to listen to women's narratives, alleviate emotional distress, and assist them in cultivating meaningful lives, regardless of their motherhood status. Future research should prioritise longitudinal studies to clarify the changing psychosocial trajectories of women with endometriosis-related infertility, integrate multiple cultural perspectives, and broaden the investigation to encompass partner and family experiences.
Finally, healthcare providers should integrate resilience-building strategies such as peer support, psychological therapy, and life-goal reframing into their care plans to provide holistic support that addresses both physical and psychosocial needs.
Strengths
This synthesis integrates diverse qualitative and quantitative evidence across two decades, offers a biopsychosocial framework that connects clinical, psychological, and social dimensions, and highlights culturally relevant perspectives often underrepresented in existing literature.
Limitations
As a narrative synthesis, this study is inherently prone to potential selection bias and may lack the methodological rigor of systematic reviews. The findings are also limited in their generalisability, as included studies vary in methodology, cultural context, and sample characteristics. Future research should employ longitudinal and crosscultural designs to validate and extend these observations.
Statement of Disclosure
The author declares that there are no conflicts of interest.
Funding
No funding was generated during the execution of this study.
References
- As-Sanie S, Black R, Giudice LC, Valbrun TG, Gupta J, et al. (2019) Assessing research gaps and unmet needs in endometriosis. Am J Obstet Gynecol 221: 86–94.
[Crossref] [Google Scholar] [PubMed]
- Culley L, Law C, Hudson N, Denny E, Mitchell H, et al. (2013) The social and psychological impact of endometriosis on women’s lives: A critical narrative review. Hum Reprod Update 19: 625–639.
[Crossref] [Google Scholar] [PubMed]
- de Graaff AA, van Lankveld J, Smits LJ, van Beek JJ, Dunselman GAJ (2016) Dyspareunia and depressive symptoms are associated with impaired sexual functioning in women with endometriosis, whereas sexual functioning in their male partners is not affected. Hum Reprod 31: 2577–2586.
[Crossref] [Google Scholar] [PubMed]
- del Pino-Sedeño T, Cabrera-Maroto M, Abrante-Luis A, González-Hernández Y, Ortíz Herrera MC (2024) Effectiveness of psychological interventions in endometriosis: A systematic review with meta-analysis. Front Psychol 15: 1457842.
[Crossref] [Google Scholar] [PubMed]
- Dyer SJ, Abrahams N, Mokoena NE, van der Spuy ZM (2004) ‘You are a man because you have children’: experiences, reproductive health knowledge and treatment-seeking behaviour among men suffering from couple infertility in South Africa. Hum Reprod 19: 960–967.
[Crossref] [Google Scholar] [PubMed]
- Engel GL (1977) The need for a new medical model: A challenge for biomedicine. Science 196: 129–136.
[Crossref] [Google Scholar] [PubMed]
- Fourquet J, Báez L, Figueroa M, Iriarte RI, Flores I (2011) Quantification of the impact of endometriosis symptoms on health-related quality of life and work productivity. Fertil Steril 96: 107–112.
[Crossref] [Google Scholar] [PubMed]
- Giudice LC (2010) Clinical practice. Endometriosis. N Engl J Med 362: 2389–2398.
- Greil A, McQuillan J, Slauson-Blevins K (2011) The social construction of infertility. Sociol Compass 5: 736-746.
- Labinjo T (2024) Faith, pain, and healing: A journey with Stage Four Endometriosis through the lens of practical theology. Practical Theology Hub.
- Lindsey B, Driskill C (2013) The psychology of infertility. Int J Childbirth Educ 28.
- Mori LP, Zaia V, Montagna E, Vilarino FL, Barbosa CP (2024) Endometriosis in infertile women: an observational and comparative study of quality of life, anxiety, and depression. BMC Women’s Health 24: 251.
[Crossref] [Google Scholar] [PubMed]
- Rajkhowa M, McConnell A, Thomas GE (2006) Reasons for discontinuation of IVF treatment: A questionnaire study. Hum Reprod 21: 358–363.
[Crossref] [Google Scholar] [PubMed]
- Simoens S, Dunselman G, Dirksen C, Hummelshoj L, Bokor A, et al. (2012) The burden of endometriosis: Costs and quality of life of women with endometriosis treated in referral centres. Hum Reprod 27: 1292–1299.
[Crossref] [Google Scholar] [PubMed]
- Vercellini P, Viganò P, Somigliana E, et al. (2014) Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol 10: 261–275.
[Crossref] [Google Scholar] [PubMed]
- Zondervan KT, Becker CM, Missmer SA (2020) Endometriosis. N Engl J Med 382: 1244–1256.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi