Research Article, J Surg Clin Pract Vol: 2 Issue: 2
The Surgical Management of Colorectal Cancer Liver Metastases in the Elderly: A Retrospective Study in the UK
Robinson S1, Jalal Q2*, Allen H2, Al-Mukhtar A2, Gardner-Thorpe J2, Majeed A2 and Peterson M2
1School of Health and Related Research, University of Sheffield, Sheffield, United Kingdom
2Hepatopancreaticobiliary Unit, Northern General Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom
*Corresponding Author : Qaiser Jalal
Hepatopancreaticobiliary Unit, Northern General Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom
E-mail: Qaiser.jalal@sth.nhs.uk
Received: March 14, 2018 Accepted: April 23, 2018 Published: April 30, 2018
Citation: Robinson S, Jalal Q, Allen H, Al-Mukhtar A, Gardner-Thorpe J, et al. (2018) The Surgical Management of Colorectal Cancer Liver Metastases in the Elderly: A Retrospective Study in the UK. J Surg Clin Pract 2:2.
Abstract
Introduction: The number of elderly patients with colorectal cancer (CRC) liver metastases is increasing. Due to their historic exclusion from clinical trials, evidence for the benefit of hepatic resection in this population is limited. The present study aimed to assess the safety and efficacy of hepatic resection for CRC liver metastases in elderly patients.
Methods: A 5-year retrospective analysis of all patients who underwent hepatic resection for CRC liver metastases at a single UK centre was performed to compare outcomes for young (<75 years old), and elderly (>75 years old) patients.
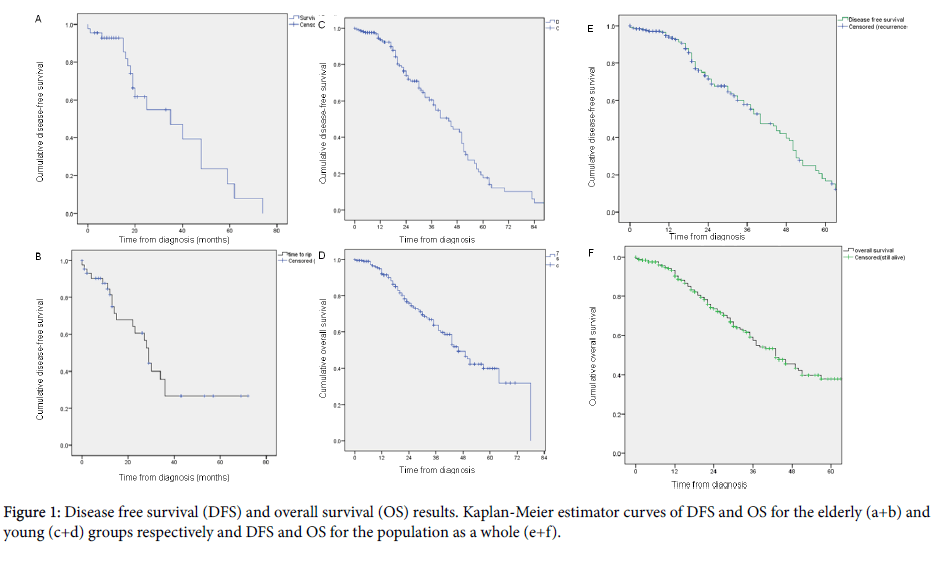
Results: Of 248 patients identified, 44 were elderly and 204 were young. The majority of patients were male (71%), underwent a minor resection (64%) and had a complete resection (87%). There was no significant difference in demographic or surgical characteristics other than age. The 5- year disease-free survival (DFS) and overall survival (OS) for all groups combined was 28.8% and 37.9%, respectively. Between the elderly and young groups there was no significant difference in median DFS (27 months vs. 32 months) but a significant difference in OS (29 months vs. 46 months). Tumour recurrence was identified to significantly predict OS for both elderly and young patients, whilst gender, type of resection, and residual tumour classification status had no statistically significant predictive value.
Conclusion: The results of the current study indicate that hepatic resection for CRC liver metastases is a safe and effective procedure in all age groups, with non-inferior outcomes in patients >75 years old.
Keywords: Colorectal cancer; Liver metastases; Elderly; Hepatic resection; Safety; Efficacy
Introduction
Colorectal cancer (CRC) is the fourth most common cancer in the United Kingdom and the second most frequent cause of cancer mortality [1]. The majority of new CRC cases (58%) occur in those >70 and with increasing life expectancy worldwide the total number of elderly patients with CRC is expected to rise markedly [2]. In the last 40 years there has been a 14% increase in CRC incidence and the majority of these additional cases have been in patients >70 years old [3]. This population of elderly patients with CRC represents an increasing priority for clinical oncology research. In total ~25% of patients with CRC present with synchronous liver metastases as their only site of metastatic disease [4] and 17% of patients with CRC develop metachronous liver metastases <10 years [5] as their only site of metastatic disease, and all these patients remain potentially curable. Therefore, hepatic resections performed by specialist hepatopancreaticobiliary surgeons are the primary treatment for synchronous and metachronous CRC liver metastases [6]. As long as the patient is physically fit and their metastases allow for a technically feasible resection, this procedure is safe and effective, with patients achieving an overall median survival of 3.6 years post-hepatic resection [7]. Historically, the extremely old have been excluded from clinical trials and so this population has frequently been overlooked for potentially curative therapies, as clinicians lacked sufficient evidence to support that the benefits of such treatments outweighed the risks. In recent years, there has been a trend towards including older patients in clinical trials; however, the weight of evidence for this population remains poor in CRC. In regards to hepatic resections for CRC liver metastases in the elderly, no consistent benefit has been observed following this treatment, in addition to variable rates of postoperative complications, morbidity and mortality [8-12]. The present study compared the demographics, treatments and outcomes for young (<75 years old), and elderly (>75 years old) patients with CRC liver metastases who underwent hepatic resection.
Materials and Methods
Study participants
All patients who underwent resection for CRC liver metastases in a 5-year period, between January 1st 2009 and December 31st 2014, at Sheffield Teaching Hospital NHS Foundation Trust (Sheffield, United Kingdom) were identified retrospectively from a patient database. For this type of study formal consent is not required. Patients were divided into two groups based upon their age as follows: ≥ 75 years old (elderly group); and <75 years old (young group). The following data was collected for each patient: age; gender; type of hepatic resection (major/minor); residual tumour classification (R classification) according to the Union for International Cancer Control [13]; and follow-up data, including the date and type of recurrence, and length of survival.
Statistical analysis
Statistical analyses were performed using SPSS software (version 22; IBM Corporation, Armonk, NY, USA). Patient demographics are expressed as numbers with percentages for categorical variables and as medians with ranges for continuous variables. Demographic and surgical characteristics were compared between the age groups. Categorical variables were compared using Fisher’s exact test and continuous variable were compared using the Mann-Whitney U test. Disease-free survival (DFS) was defined as the time between computerized tomography (CT) scan diagnosis (or surgery if unknown) and disease recurrence (or last follow-up). Overall survival (OS) was defined as the time between CT scan diagnosis (or surgery if unknown) and mortality (all causes; or last follow-up). Peri-operative deaths were defined as death from any cause within 1 month from surgery. Survival rates were determined using the Kaplan-Meier estimator and compared using the log-rank test. The Cox regression model was used to identify factors that significantly predicted survival. All tests were two-tailed and p<0.05 was considered to indicate a statistically significant difference.
Results
A total of 248 patients with CRC who underwent liver resection for liver metastases were identified in the present study. Of these patients, 44 (17.7%) were classified as elderly and 204 (82.3%) as young. Table 1 details the demographic and surgical characteristics of the patients and subgroups. As demonstrated in Table 1, there was a significant difference in the ages of patients in the two groups (p<0.000). The elderly group had a median age of 77 years old compared with the young group, which had a median age of 65 years old. In addition, the majority of patients in the present study were male (70.6%). The elderly group were 75.0% male compared with 69.6% in the young group, although this difference was not statistically significant (p=0.585). The majority of patients included in the current study underwent a minor hepatic resection (64.1%) and had a completely resected tumour (R0, 87.1%) (Table 1). There was minimal difference in the type of tumour resection between the age groups, with 61.4% of the elderly group undergoing a minor hepatic resection compared with 64.7% in the young group (Table 1). In addition, 93.2% of the elderly group had their tumour completely removed (R0) compared with 85.8% in the young group (Table 1). Neither of these comparisons were statistically significant (p=0.730 and p=0.223, respectively). Figure 1 demonstrates the DFS and the OS of the groups separately and combined. As such in Figure 1, the elderly group had a median DFS of 27 months [95% confidence interval (CI), 21.1-32.9 months] compared with the young group, which had a median DFS of 32 months (95% CI, 27.0-37.0 months). This was not a statistically significant difference with a p value of 0.234. In addition, the 5-year DFS for the elderly group was 20.9% compared with 20.2% for the young group. For all groups combined, the median DFS was 30 months (95% CI, 25.9-34.1 months) (Figure 1). The 1- and 5-year DFS rates for all groups combined were 93.5% and 28.8%, respectively (Figure 1). As shown in (Table 2), for both elderly and young patients no variable was a statistically significant predictor for DFS. The gender (p=0.672 vs. 0.065), type of resection (p=0.727 vs. 0.200), and residual tumour classification status (p=0.334 vs. 0.930) of the patient had no statistically significant predictive value (Table 2). Figure 1 demonstrates the OS for the elderly group compared with the young group. The elderly group had a median OS of 29 months [95% confidence interval (CI), 25.9-32.1 months] compared with the young group, which had a median OS of 46 months (95% CI, 39.7-52.3 months). This was a statistically significant difference with a p value of 0.006. The 5-year OS for the elderly group was 26.7% compared with 39.9% for the young group. For all groups combined, the median OS was 43 months (95% CI, 35.4-50.6 months) (Figure 1). The 1- and 5-year OS rates were 93.5% and 37.9%, respectively (Figure 1). There was 1 perioperative death in each age group (Figure 1). As shown in Table 3, tumour recurrence was a statistically significant predictor of OS for both elderly (p=0.005) and young patients (p=0.000). Elderly patients who had not had their tumour recur were 7.8 times more likely to be alive compared with patients who had their tumour recur at the last point of data collection. Whilst young patients who had not had their tumour recur were 6.0 times more likely to be alive compared with patients who had their tumour recur. The gender of the patient, whether it was a major or minor resection, and whether they had a complete or incomplete resection had no statistically significant predictive value.
| Patient characteristic | All Patients | Elderly (≥75 years old) |
Young (<75 years old) |
p-value | |
|---|---|---|---|---|---|
| Age median (range) |
67 (39-83) | 77 (75-83) | 65 (39-74) | <0.000 | |
| Gender number (%) |
Male | 175 (70.6) | 33 (75.0) | 142 (69.6) | 0.585 |
| Female | 73 (29.4) | 11 (25.0) | 62 (30.4) | ||
| Type of Resection number (%) |
Major | 89 (35.9) | 17 (38.6) | 72 (35.3) | 0.730 |
| Minor | 159 (64.1) | 27 (61.4) | 132 (64.7) | ||
| R classification number (%) |
R0 | 216 (87.1) | 41 (93.2) | 175 (85.8) | 0.223 |
| R1 | 32 (12.9) | 3 (6.8) | 29 (14.2) | ||
Table 1: Demographic and surgical characteristics for all patients and separate groups.
| Patient characteristic | Comparison | Age group | p-value | Hazard ratio |
|---|---|---|---|---|
| Gender | Female vs. male | Elderly | 0.672 | 0.759 |
| Young | 0.065 | 0.608 | ||
| Type of resection | Major vs. minor resection | Elderly | 0.727 | 1.198 |
| Young | 0.200 | 0.714 | ||
| R classification | R1 vs. R0 | Elderly | 0.334 | 2.525 |
| Young | 0.930 | 1.036 |
Table 2: Results of Cox regression model analysis assessing the predictiveness of patient characteristics for disease-free survival.
| Patient characteristics | Comparison | Age group | p-value | Hazard ratio | ||
|---|---|---|---|---|---|---|
| Gender | Female vs. male | Elderly | 0.063 | 0.295 | ||
| Young | 0.642 | 0.883 | ||||
| Type of resection | Major vs. minor resection | Elderly | 0.838 | 1.098 | ||
| Young | 0.102 | 1.505 | ||||
| R classification | R1 vs. R0 | Elderly | 0.147 | 5.952 | ||
| Young | 0.286 | 1.505 | ||||
| Tumour recurrence | Yes vs. no | Elderly | 0.005 | 7.759 | ||
| Young | 0 | 6.006 | ||||
Table 3: Results of Cox regression model analysis assessing the predictiveness of patient characteristics for overall survival.
Discussion
As the average age has increased worldwide, there has been a corresponding increase in the number of elderly patients developing CRC and CRC liver metastases [1]. This represents a major challenge to clinicians, as this patient group has frequently been excluded from clinical trials, directly due to their age or indirectly due to comorbidities. At present there is no definitive consensus in regards to whether hepatic resection is a safe and effective treatment in elderly patients with CRC liver metastases [8]. A number of previous studies have investigated this area, with conflicting results [9-11]. Various studies have observed that hepatic resection increases morbidity and mortality in elderly patients compared with younger patients [9,10] whilst other studies have identified that elderly populations have noninferior outcomes compared with younger patients [11,12]. The results of the present study indicate that hepatic resection is beneficial in elderly patients with CRC liver metastases, and therefore age should be no barrier for this potentially curative operation. With a 2:1 patient ratio of males: females and a median patient age of 66 years old, the results of the current study are comparable with previously published data in regards to the demographic characteristics of patients with CRC liver metastases [14]. In addition, data from the present study is comparable to previously published data from other centres regarding rates of R1 resection [15]. Therefore, the present study is well placed to evaluate the benefit of liver resection in elderly patients with CRC liver metastases and allows better extrapolation of the results to the wider population. The present study identified no significant differences in the proportion of males: females, type of resection performed (major or minor) or surgical outcome (R0 or R1 tumour resection) between the groups. Therefore, any difference, or lack of difference, in patient outcome was due to age alone or other inherent biases in patient selection. Whilst not statistically significant, there was a trend towards patients >75 years old having a complete tumour resection compared with those <75 in the present study. This likely represents a selection bias inherent to the surgeon’s clinical judgement. Hepatic resection for CRC liver metastases is high risk and so for the surgeon to consider that the benefits outweigh the risks for an elderly patient they are likely to select patients with smaller lesions, a smaller number of lesions or more well-defined lesions. Whilst this bias may skew the results, it suggests that the surgeon’s judgement is an important factor in predicting the resectability of CRC liver metastases. The results of the present study indicate that hepatic resection is a safe and effective treatment for CRC liver metastases in all age groups, including those >75 year olds. Following this treatment, there were only 2 perioperative deaths, and good long-term outcomes in regards to DFS and OS. In addition, there were no significant difference in DFS, although there was a significant difference in OS. This difference was not associated with gender, type of resection, or residual tumour classification status. Whilst disease-specific survival was not recorded, the difference in OS is possibly due to co-morbidities which the elderly patients suffered from and not directly related to their cancer. As expected, disease recurrence was significantly associated with OS. The 5-year DFS and OS rates following hepatic resection for CRC liver metastases identified in the present study, 28.8% and 37.9%, respectively, match well with recent published results that have reported 5-year outcomes of up to 24% for DFS and 34-52% for OS [15]. These results suggest that the patients analysed in the present study were carefully selected for this complex and high-risk operation. The primary limitation of the current study was the small sample size, which limits the power of the statistical analyses. Nevertheless, the results of the present study suggest that, elderly patients who undergo hepatic resection for CRC liver metastases have good long term outcomes and any reduced survival rates compared with younger patients is probably due to co-morbidities.
Conclusions
The results of the present study indicate that hepatic resection is a safe and effective treatment for the management of CRC liver metastases in all age groups, including the >75 year olds. These results support those of previous reports, which suggest that age should not be a barrier to this potentially life-saving operation. In future, these results should be validated by conducting a statistically well-powered prospective study to demonstrate non-inferiority for elderly patients compared with younger patients.
References
- Cancer Research UK, Bowel Cancer Incidence Statistics, UK.
- McMilan DC, McArdle CS (2007) Epidemiology of colorectal liver metastases. Surg Oncol 16: 3-5.
- Landreau P, Drouillard A, Launoy G, Ortega-Deballon P, Jooste V, Lepage C, et al(2005)Incidence and survival in late liver metastases of colorectal cancer. J Gastroenterol Hepatol 30: 82-85.
- Garden OJ, Rees M, Poston GJ, Mirza D, Saunders M, et al. (2006) Guidelines for resection of colorectal cancer liver metastases. Gut 55: iii1–iii8.
- Kanas GP, Taylor A, Primrose JN, Langeberg WJ, Kelsh MA, et al. (2012) Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol 4: 283–301.
- Papamichael D, Audisio R, Horiot JC, Glimelius B, Sastre J, et al. (2009) Treatment of the elderly colorectal cancer patient: SIOG expert recommendations. Ann Oncol 20: 5-16.
- Nachmany I, Pencovich N, Zohar N, Goykhman Y, Lubezky N, et al. (2016) Resection of colorectal liver metastases in the elderly - Is it justified? J Surg Oncol 113: 485-488.
- Booth CM, Nanji S, Wei X, Mackillop WJ (2015) Management and outcome of colorectal cancer liver metastases in elderly patients: a population-based study. JAMA Oncol 1: 1111-1119.
- Nomi T, Fuks D, Kawaguchi Y, Mal F, Nakajima Y (2015) Laparoscopic major hepatectomy for colorectal liver metastases in elderly patients: a single-centre, case-matched study. Surg Endosc 29: 1368-1375.
- Tie M, Zhu J, He X, Yang Z, Chen X, et al. (2015) Liver metastasis from colorectal cancer in the elderly: Is surgery justified? Dig Dis Sci 60: 3525-3535.
- Herman P, Wittekind C (1994) The pathologist and the residual tumour (R) classification. Patrol Res Pract 190: 115-123.
- Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, et al. (2006) Epidemiology and management of liver metastases from colorectal cancer. Ann Surg 244: 254-259.
- Brudvik KW, Bains SJ, Seeberg LT, Labori KJ, Waage A, et al. (2013) Aggressive treatment of patients with metastatic colorectal cancer increases survival: a scandinavianan single-centre experience. HPB Surg 2013: 727095.
- Kuo IM, Huang SF, Chiang JM, Yeh CY, Chan KM, et al. (2015) Clinical features and prognosis in hepatectomy for colorectal cancer with centrally located liver metastasis. World J Surg Oncol 13: 92.
- Chan KM, Wu TH, Cheng CH, Lee WC, Chiang JM, et al. (2014) Prognostic significance of the number of tumours and aggressive surgical approaching colorectal cancer hepatic metastasis. World J Surg Oncol 12: 155.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi