Research Article, Int J Glob Health Vol: 6 Issue: 2
Uganda’s Model (UgaMod) towards the Rapid Control of COVID-19 Outbreak: Utilizing a Public Health Emergency Governance Mechanism
Betty Nannyonga1*, Henry Kyobe Bosa2, Irene Wanyana3, Susan Kizito3, Yonas Tegegn Woldermariam4, Pontiano Kaleebu5, John M Ssenkusu3, Tom Lutalo3, Willford Kirungi6, Fredrick Edward Makumbi3, Vincent A Ssembatya1, Henry G Mwebesa6, Diana Atwine6, Jane Ruth Aceng6 and Rhoda K Wanyenze3
1Department of Mathematics, College of Natural Sciences, Makerere University, Kampala, Uganda
2Department of Public Health, University of Oxford, Oxford, England
3Department of Public Health, Makerere University, Kampala, Uganda
4Department of Preventive Medicine, Makerere University, Kampala, Uganda
5Department of General Virology, Uganda Virus Research Institute, Entebbe, Uganda
6Department of Health Services, Makerere University, Kampala, Uganda
*Corresponding Author: Betty Nannyonga
Department of Mathematics, College of Natural
Sciences, Makerere University, Kampala, Uganda
E-mail: betty.nannyonga@mak.ac.ug
Received date: 04 January, 2023, Manuscript No. IJGH-23-85448;
Editor assigned date: 06 January, 2023, PreQC No. IJGH-23-85448 (PQ);
Reviewed date: 20 January, 2023, QC No. IJGH-23-85448;
Revised date: 03 March, 2023, Manuscript No. IJGH-23-85448 (R);
Published date: 10 March, 2023, DOI: 10.4172/IJGH.1000177
Citation: Nannyonga B, Bosa HK, Wanyana I, Kizito S, Woldermariam YT, et al. (2023) Uganda’s Model (UgaMod) towards the Rapid Control of COVID-19 Outbreak: Utilizing a Public Health Emergency Governance Mechanism. Int J Glob Health 6:2.
Abstract
The outbreak of COVID-19 has been of global health concern since its outbreak in Wuhan China, in December 2019. It is still a global public health emergency for the entire world, and threatens human life, economic dignity and public health security. As of August 31, 2022, there have been 607,330,258 cases worldwide, 6,492,385 deaths, and 583,355,283 recoveries. There are currently 17,482,590 active cases, where 17,439,463 (99.8%) are mild while 43,127 (0.2%) are serious or critical. Of these, 169,396 cases, 100,431 recoveries, and 3,628 deaths are attributable to Uganda. To address the outbreak, Uganda undertook to implement timely and multiple prevention measures, and also incorporated effective and targeted public health emergency governance. In this paper, we present Uganda’s model (UgaMod) that was used to contain the COVID-19 outbreak from a public health emergency governance approach. This approach stemmed from standard operating procedures, mitigation strategies and measures by the Ugandan government, which included enforcement of public response and adherence, setting up multi-sectoral teams and task forces for monitoring and evaluation, scaling up emergency response capacities to respond, and engaging communities in the basic epidemic prevention, control and response.
Keywords: Public health; COVID-19; Virus disease; Human life; Leadership, Stewardship
Introduction
COVID-19, a pandemic of public health emergency and of international concern, is still a serious global threat to human life and public health security. To address the outbreak, Uganda not only undertook good prevention and treatment measures, but also set up an effective and targeted public governance mechanism in terms of provision of information, decision-making and execution [1].
The Ugandan response to the COVID-19 pandemic is laid out in the national Corona Virus Disease (COVID-19) preparedness and response plan and followed the timeline in Table 1.
| March 5th, 2020 | Airport screening introduced. |
| March 11th, 2020 | Institutional quarantine for passengers travelling from category 1 countries. |
| March 18th, 2020 | Public gatherings suspended for 32 days with immediate effect; ban for Uganda travel to category 1 countries; school closed for 30 days. |
| March 22nd, 2020 | First confirmed case |
| March 25th, 2020 | Public transport suspended for 14 days; ban on international travels. |
| March 30th, 2020 | Lockdown; nationwide curfew from 7 pm to 6:30 am for 14 days. |
| April 15th, 2020 | Lockdown extended. |
| May 5th, 2020 | Lockdown extended for 14 days, but some restrictions eased. |
| May 18th, 2020 | Curfew extended; shops, outside of shopping malls reopened; public transport reopened; school opened for end of educational phases candidates. |
Table 1: COVID-19 related response timeline.
The key principles for preparedness and response to COVID-19 encompassed utilization of ICT innovations, community led approach and 24 hours surge capacity. The plan was arranged in 3 scenarios: Scenario 1 (best case scenario): No case is identified in Uganda and activities are focused on preparedness scenario 2 (most likely scenario), a single case is identified in Uganda response activities are initiated, and command and control structure shifted to the office of the prime minister and scenario 3 (worst case scenario), multiple cases are identified in which case activities of scenario 2 are enhanced and business continuity plans per sector activated. The response was centered around 8 key COVID-19 response pillars namely: Leadership, stewardship, coordination and oversight, all critical due to contributions from different sectoral agencies, teams and partners towards a common goal case management, as treatment was mainly supportive due to no definitive treatment at the time continuity of essential services aimed at strengthening community infection prevention and control community engagement and social protection due to mental health problems, social disruption to the infected and affected surveillance and laboratory to facilitate early detection, confirmation, reporting, notification, verification and response of alerts and suspected cases risk communication and social mobilization due to limited knowledge about the virus logistics and operations to ensure that logistical needs are availed to the different sites according to need in a timely and efficient manner and strategic information, research and innovation due to the fast evolving Corona virus that required innovation and leveraging of digital health in the preparedness and response.
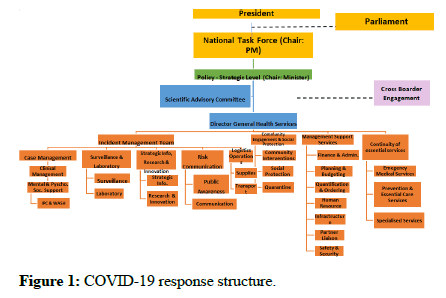
To affect the COVID-19 response pillars, Uganda established a nationwide joint prevention and control system to educate, surveil, identify, trace, vacate, and quarantine suspected cases, and to contain the critical cases with a structure in Figure 1.
By May 09 2020, the strategy had yielded positive results for Uganda reporting one confirmed case, or no domestic confirmed cases [2]. By this time, Uganda had confirmed 137 cases with a fatality rate of 0 percent. Most of the confirmed cases were truck drivers from neighboring countries like Kenya, South Sudan and DRC.
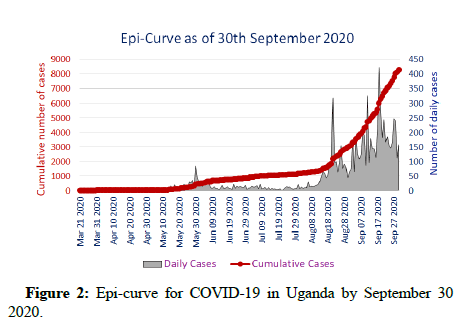
In phase 1, there were no cases, ports of entry were controlled, and travels to high-risk areas restricted. Uganda was in this phase up to March 22, 2020, when the first case was reported [3]. Phase 2 was when sporadic cases arose due to returning residents. The main aim here was to prevent local transmission to contacts, with containment measures including identification and quarantine of suspected individuals/cases. In phase 3, clusters of community spread were observed [4]. Uganda transitioned from sporadic cases to clusters at Ports Of Entry (PoE) at Elegu/Nimule and Malaba due to cross border build-up by exiting and incoming trucks, and slow testing and delivery of results. The major aim of the national response during this phase was to prevent transmission beyond the infected clusters. Uganda remained in this phase till around May 09, 2020 when the lockdown was eased [5]. Even with the introduction of extensive containment measures, non-adherence to mitigation measures was a major challenge and hence Uganda started transitioning to phase 4, with widespread community spread. Several indirect local contacts and multiple unconnected clusters of COVID-19 had been reported by end of September 2020. Deaths continued to rise, and the epidemic curve was oscillating (Figure 2). Since the emergence of clusters, there was re-deployment of efforts targeting the epicenters and PoE, in order to optimize resources. Uganda also enhanced border testing, surveillance and management of cases [6].
While the Ministry of Health (MOH) was responsible for policy and strategy, it coordinated with the office of the prime minister on the strategic and operational command of the response, as well as a series of cross-cutting functions, such as planning, budgeting, and partner coordination [7]. The already existing district surveillance teams and District Task Forces (DTF) were immediately called into play to respond to the virus in their jurisdictions.
Materials and Methods
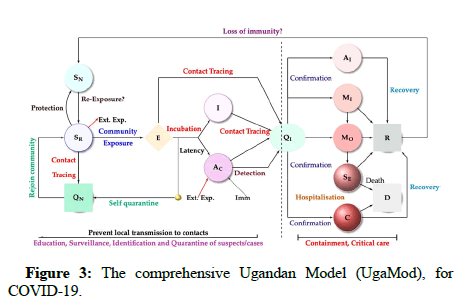
Although most of the cases from March through June 2020 were predominantly imported cases of truck drivers from neighboring countries, by the end of September 2020, Uganda had transitioned into community transmissions and most of the reported cases were local contacts and alerts (Figure 3). In its initial stages, Uganda responded with various restrictions and interventions including lockdown, physical distancing, hand hygiene, and use of face masks in public facilities etc., to control the growth rate [8-11]. This study gives a background on which the Ugandan model was designed, the assumptions, data used and eventual outputs for specific objectives such as different ways of implementing mitigation measures to control the outbreak. Among the COVID-19 response structure was the Uganda COVID-19 Scientific Advisory Committee (UGSAC) that comprised of a team of specialists from the ministry of health Uganda, makerere university college of health sciences, World Health Organization (WHO), and Uganda national academy of sciences, Kampala capital city authority, and makerere university college of natural sciences [12].
Objective: To report on the public health emergency governance mechanism that collectively and swiftly made strong emergency responses that combated COVID-19 in Uganda.
Specific objectives
• To illustrate the public health emergency governance mechanism.
• To summarize Uganda’s COVID-19 model that derived the policies
behind the positive intended response mechanisms.
Methods: The government’s response in the public health emergency governance mechanism included.
• The quick development of institutional arrangements to implement
control measures.
• Rapid pooling and allocation of funds.
• The development operational guidance to health system
stakeholders on how to respond and the development of standard
operating procedure.
To come up with the Ugandan model (UgaMod), the biology of infection of COVID-19 was considered, using information provided by the world health organization and other prior mathematical models for disease. These interventions were considered to design the Uganda COVID-19 model (UgaMod), that was instrumental in combating the virus and policy making.
The Uganda COVID-19 model (UgaMod) Before the first case was confirmed on March 22, 2020, the country was under partial lockdown, with schools closed but other sectors operational. After registering her first case, a complete lockdown was declared and movement was restricted. A public call was made to all returning citizens or visitors to report for testing, as well as their contacts. All those individuals were considered exposed and placed under self or institutional quarantine. While there, daily screening and testing was done to determine whether they were infected or not, and if so, the severity of their disease determined [13]. These dynamics of the government decisions, together with implemented mitigation measures informed the design of the model, which is a flow diagram based on characterization of the virus at cellular and population levels.
The Susceptible state (S) were the individuals at risk of infection, which included the protected (locked down at home) SN, and the essential workers who were allowed to move with a high risk of exposure SR). The Exposed (E) states were those that had come in contact with infected individuals but had not been clinically confirmed to have the virus. Before clinical confirmation and while waiting for test results, some exposed individuals quarantined in their homes (non-institutionalized Quarantine QN), where they remained for the next fourteen days until proven clinically negative to join the community, or positive, to be checked into institutionalized quarantines. After exposure and through alerts and contact tracing, some individuals tested and were confirmed to have COVID-19 with symptoms (I), or no symptoms (Asymptomatic, AC). This marked the end of the education, surveillance, identification, and quarantine of suspected cases. Both the confirmed symptomatic and asymptomatic cases were admitted in institutional Quarantines (QI), where further disaggregation was done based on severity of infection. These included the Asymptomatic in the Institution (AI), the Mild (MI), Moderate (MO), Severe (SE) and Critical (C). This was the containment and critical phase, where the severely and critically infected individuals would need hospital bed care and therefore formed a basis for threshold number of bed units, ventilators, or oxygen required in the treatment centers [14]. While in hospitals, some of the confirmed cases would respond to treatment and recovered to join class R, or died and joined class D. Using the world health organization guidelines. We based the UgaMod, on the concepts, parameterized using COVID-19 data from Uganda and determined the parameters that influenced its transmission from March 22, 2020.
These assumptions and descriptions gave rise to the Ugandan Model, UgaMod, which was a function fifteen variables all dependent on time.
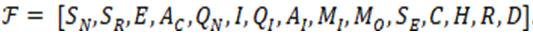
Therefore, the system of equations used were given by
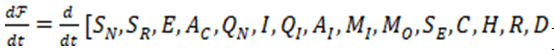
And gave the active number of cases in each transition state.
The dynamics of COVID-19 was modeled by the UgaMod under the assumption of frequency dependent transmission, where a successful positive contact depended on the probability of infection and the number of contacts made by an individual per unit time. According to WHO, the risk of exposure to Ugandans was 3.7% of the entire population, and only 10% of those resulted in positive tests. The 90% were sent to non-institutional quarantine where they remained for fourteen days, and returned to the population after confirmation of a negative PCR or antigen test. Of the 10% successful exposures, 80% did not develop symptoms while the 20% become symptomatic after an average of 5 days (WHO). Of the 20%, 8 were mild, 8% moderate, 3% severe and 1% critical [15].
As in prior studies on respiratory diseases, we assumed that asymptomatic individuals transmitted COVID-19 at a reduced rate compared to those with full blown symptoms. We also assumed that the transmission rate was slowed down by the implemented standard operating procedures such as lockdown, frequent hand washing, public face masks and physical distancing. We therefore constructed a transmission term which is a function of all these mitigation measures, and this was incorporated in the transmission term [16]. Changing the percentages of these mitigation coverages led to different numbers either applied singly or in combination with others. The best strategy was then identified and formed a basis for policy implementation. In the model, environmental transmission and contamination were ignored but only considered direct person to person infection. The model also included immigration at PoE, and porous borders, all assumed to enter the country while exposed but still asymptomatic.
Transitional probabilities
Using the WHO guidelines as in Cabore, et al., the probability of having mild, moderate, severe or critical disease was approximately 40%, 40%, 15% and 5%, respectively. Although hospitalization rates depended on policy and capacity, it was estimated that 30% of symptomatic patients needed hospitalization, with case fatality highest for critical cases (up to 89% without intervention) and 49% for severely ill patients. The infection induced mortality rate was estimated at less than 0.1%. We also tested our assumptions on parameters using sensitivity analysis, leading to a robust model for infection of COVID-19 in Uganda [17].
The basic reproduction number, R0
The basic reproduction number is the average number of secondary infections that arise from a single infective individual during their infectious period when everyone else in the population is susceptible and depicted the transmission risk in the early phase of COVID-19 transmission. In the model, the basic reproductive number was determined to be:
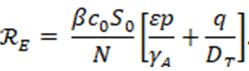
This was a sum of two terms: The proportion of new infections that arose from the asymptomatic individuals before they shed off the virus, and the proportion from the symptomatic before they were detected.
Results
Due to high transmission rates of the virus, Uganda responded with intensive intervention measures that were expeditiously implemented and led to gradual enhanced self-protection. In order to quantity the daily reproduction number and evaluate the transmission risk changing over time, the initial contact rate c0 in the expression for the basic reproductive number ℛ0 was replaced by the time-dependent contact rate c(t) to reflect the changes of intervention measures and people's behaviors. This gave;
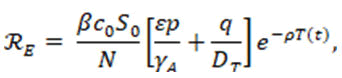
Where,
ρ=Level of adherence, and
T (t)=Active cases at any time t.
As in prior studies, in presence of control, the relationship between ℛ0 ℛ0 and ℛE was given by;
ℛE=(1-level of control) ℛ0
Using this expression, we computed the different levels of adherence with change in the number of active cases in real time.
Incorporating Non-Pharmaceutical Interventions (NPIs)
The model incorporated the Non-Pharmaceutical Interventions (NPIs) that related to the social distancing and hygiene measures Uganda implemented to reduce attack rate. Attack rate is the percentage of an at-risk population that contracted the disease in a specific time interval. The NPIs used were protection, or shielding the vulnerable, physical/social distancing, sanitizing, wearing facemasks in public, lockdown or closure, and restriction of movement [18]. By July 21, 2020, 7,121,246 masks had been distributed. Hot-spot districts were prioritized and supported with intensified surveillance, contact tracing, and testing alongside enhanced community engagement (Table 2).
| Scenario | Description |
|---|---|
| Unmitigated | No governmental intervention applied. |
| Social/physical distancing | Assuming moderate physical distancing measures restricting movement or limiting contacts with others. |
| Shielding of the vulnerable | The elderly (>65 years) and those with underlying conditions such as, TB, diabetes. |
| Public wearing of face masks | We assumed 30% compliance based on the 2020 Rapid Assessment Survey (RAS) undertaken by makerere university school of public health. |
| 50% hand-washing, 6 times a day | We assumed increase in hand-washing from 26% (Uganda demographic health survey 2016) to 50% based on the 2020 online survey by makerere school of public health. |
Table 2: Intervention scenarios analyzed in UgaMod.
Forecasting COVID-19
We forecasted COVID-19 using data and predict the expected number of cumulative cases. Four approaches namely linear forecasting, the trend line, slope and intercept, the equation of best fit we applied to the data. These forecasts based on statistical and/or mathematical models that aimed to predict national and regional numbers of new and total COVID-19 in terms of deaths, hospitalizations, and/or cumulative cases for a given period of time. The forecasting was done using different types of data, such as COVID-19 data, demographic data, and mobility data, and employed different methods, and estimates of the impacts of interventions (e.g., hand washing, social distancing, and use of face masks). These forecasts were useful as real-time tools and helped guide policy and planning. Different approached were used to increase the robustness of forecasts.
The gradual lifting of the national lockdown was accompanied by intensified communication of the presidential directives on the mandatory use of masks in public places and the observance of physical distancing measures. The government of Uganda also launched mass mask distribution across the country, targeting all individuals aged 6 years and older. By August 31, 2020, there was a reduction in compliance to mitigation measures (Table 3). As of September 30, 2020, wearing masks was sometimes enforced, but in other areas appearing with a mask was optional and observed by nonlocals. Using the non-pharmaceutical interventions relating to the distancing, facemasks, and hygiene, the percentage coverage of each used singly or in combination with others was determined.
| Mitigation (detection rate 5 days), number of contacts=30 | % coverage | No. of secondary infections R0 | Coverage to reduce R0 to less than 1 (thresholds) |
|---|---|---|---|
| Used as standalone | |||
| Face masks | 30% | 1.46 | 60% |
| Washing hands 6 times a day/sanitizing | 26% | 2.02 | 70% |
| Social distancing | 10% | 1.88 | 60% |
| Used in combination | |||
| Face masks and washing hands 6 times a day/sanitizing | 30%, 26% | 1.46 | 50%, 30% |
| Social distancing and washing hands 6 times a day/sanitizing | 10%, 26% | 1.88 | 50%, 40% |
| Face masks and social distancing | 30%, 10% | 1.32 | 60%, 50% |
| Used simultaneously | |||
| Face masks and washing hands 6 times a day/sanitizing and social distancing | 30%, 26%, 10% | 1.32 | 50%, 30%, 50% |
Table 3: Mitigation coverages needed to control COVID-19.
Sensitivity indices
Sensitivity indices helped to determine which parameters were responsible for persistence of disease in the population. We observed from the indices that the probability of infection was most sensitive and therefore measures to prevent infection would be enforced. This included the non-pharmaceutical interventions, and vaccination that reduce susceptibility of the population. Reducing susceptibility implied targeting those populations that were vulnerable to prevent exposure. The recovery rate was also very sensitive to how many secondary infections are expected from a single exposure. This meant that the longer the recovery time was the more chances of a secondary infection. Preventing such infections would include vaccination of health personnel, and also measures that ensured quick recovery of infectious individuals. The proportion of asymptomatic individuals and their probability of transmission also led to increase in secondary infections. The higher these values were; the more infections were expected. It was therefore imperative that asymptomatic individuals prevented further transmission through observation of the set standard operating procedures. The number of symptomatic individuals in the population increased chances of new infections but not as in the asymptomatic case. This was because these people had been identified and could be avoided unlike in the previous cases when an individual might not tell the status of another due to absence of symptoms. The detection rate affected the number of new infections in that when it was high, R0 is low, and when it was low, R0 was high. Therefore, the longer it took to detect and confirm a positive case implied that this person could infect more people and increased cases y within communities (Table 4).
| Parameter | Description | Estimated value | Index | Reference | Interpretation |
|---|---|---|---|---|---|
| β | Probability of infection | 0.0216-0.0413 | 6.6366-10.0976 | Cabore et. al. | ℛ0 increases with bb |
| c0 | Number of contacts | 20 | 0.0109-0.0209 | Ugandan data | ℛ0 increases with contacts |
| ε | Transmissibility of asymptomatic compared with the symptomatic | 0.8 | 0.2686-0.5136 | Ugandan data | ℛ0 increases with high transmissibility of the asymptomatic |
| γA | Recovery rate of asymptomatic individuals | 0.0476-0.0714 | 3.8337-8.6327 | Ugandan data | Long recovery days greatly influence an increase in ℛ0 |
| p | Proportion of asymptomatic individuals | 0.8 | 0.2686-0.5136 | Ugandan data | ℛ0 increases with high number of the asymptomatic |
| q | Proportion of symptomatic individuals | 0.2 | 6.6601×10-4-0.0160 | Ugandan data | ℛ0 increases with high number of symptomatic |
| DT | Detection rate | 0.041667-1 | -5.5501×10-6-0.0032 | Ugandan data | ℛ0 increases with reduced detection rate |
Table 4: Sensitivity indices of ℛ0 parameters.
Discussion
Setting up a multi-sectoral response structure was an important approach to public health governance of COVID-19 in Uganda. However, the outbreak of COVID-19 highlighted a series of governance issues and tested the governing capacity of nations. Although the pandemic was controlled with the strategies that were set up in Uganda, other secondary effects of the pandemic took a toll on services such as reduced HIV management, lack of ante natal care, high increase in child labor, high school dropouts, high poverty rates, high early pregnancy rates, and a huge toll on the socio-economic transformation of the nation. It is therefore important to study the governance mechanisms in public health emergency management. Many questions remain unanswered such as whether the outbreak could have been prevented; or if the outbreak and spread of the virus were inevitable, were the measures undertaken enough to slow the outbreak; or once it became a pandemic, could the socio-economical costs have been reduced with better and efficient policies; or, in case mistakes were made, is there anything to learn from them and foster pandemic preparedness.
Conclusion
This could call for examination of the effectiveness of government agencies, contingency plans, and governance frameworks in emergency management. At all different levels of decision-making and policy execution, emphasis on coordinating with other stakeholders could be stressed, regarding both virus containment and economic revival. With a probability of infection at just 3.7% in Uganda, COVID-19 was an event of low probability but high impact, and to combat such a disease would need decision models that integrate habitual thinking and political concerns, adequacy and authenticity of information disclosure, and empowering scientific and professional approaches to enhance performance in curbing the pandemic, as well as economic and social development.
References
- Olum R, Bongomin F (2020) Uganda's first 100 COVID-19 cases: Trends and lessons. Int J Infect Dis 96:517-518.
- Cabore JW, Karamagi HC, Kipruto H, Asamani JA, Droti B, et al. (2020) The potential effects of widespread community transmission of COVID-19 infection in the world health organization African Region: A predictive model. BMJ Glob Health 5:e002647.
[Crossref] [Google Scholar] [PubMed]
- Liu R, Wu J, Zhu H (2007) Media/psychological impact on multiple outbreaks of emerging infectious diseases. Comput Math Methods Med 8:153-164.
- Diekmann O, Heesterbeek JAP, Metz JA (1990) On the definition and the computation of the basic reproduction ratio R0 in models for infectious diseases in heterogeneous populations. J Math Biol 28:365-382.
- Van den Driessche P, Watmough J (2002) Reproduction numbers and sub-threshold endemic equilibria for compartmental models of disease transmission. Math Biosci 180:29-48.
[Crossref] [Google Scholar] [PubMed]
- Kombe IK, Munywoki PK, Baguelin M, Nokes DJ, Medley GF (2019) Model-based estimates of transmission of respiratory syncytial virus within households. Epidemics 27:1-11.
[Crossref] [Google Scholar] [PubMed]
- Tang B, Bragazzi NL, Li Q, Tang S, Xiao Y, et al. (2020) An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov). Infect Dis Model 5:248-255.
[Crossref] [Google Scholar] [PubMed]
- Sassi F, Archard L, Le Grand J (2001) Equity and the economic evaluation of healthcare. Health Technol Assess 5:1-13.
[Crossref] [Google Scholar] [PubMed]
- Mizumoto K, Kagaya K, Chowell G (2001) Early epidemiological assessment of the transmission potential and virulence of coronavirus disease 2019 Wuhan city, China,. BMC Med 18:217.
[Crossref] [Google Scholar] [PubMed]
- Huppert A, Katriel G (2013) Mathematical modelling and prediction in infectious disease epidemiology. Clin Microbiol Infect 19:999-1005.
[Crossref] [Google Scholar] [PubMed]
- Nishiura H, Chowell G (2009) The effective reproduction number as a prelude to statistical estimation of time-dependent epidemic trends. Math Stat Estim Approach Epidemiol 103-121.
- You C, Deng Y, Hu W, Sun J, Lin Q, et al. (2020) Estimation of the time-varying reproduction number of COVID-19 outbreak in China. Int J Hyg Environ Health 228:113555.
[Crossref] [Google Scholar] [PubMed]
- Blayney K, Cao Y, Kwon HD (2009) Optimal control of vector borne diseases: Treatment and prevention. Discrete Contin Dyn Syst-B 11:587-611.
- Chowell G, Hincapia-Palacio D, Ospina J, Pell B, Tariq A, et al. (2016) Using phenomenological models to characterize transmissibility and forecast patterns and final burden of zika epidemics. PLOS Curr.
[Crossref] [Google Scholar] [PubMed]
- Mizumoto K, Chowell G (2020) Estimating risk for death from coronavirus disease, China, January-February 2020. Emerg Infect Dis 26:1251-1256.
[Crossref] [Google Scholar] [PubMed]
- Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, et al. (2020) Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis 20:669-677.
[Crossref] [Google Scholar] [PubMed]
- Lenhart S, Workman JT (2007) Optimal control applied to biological models. 1st edition. Chapman and Hall: New York.
- Keeling MJ, Rohani P (2008) Modeling infectious diseases in humans and animals. Clin Infect Dis 47:864-865.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi