Research Article, J Womens Health Vol: 13 Issue: 2
Unmet Needs in the Healthcare Experience of Women of Childbearing Age with Chronic Disease and Recommendations for Change
Sara Franklin1,2*, Trishna Bharadia2,3, Julia-Tatjana Maul4,5, Christiane Schneider-Gold6, Louise Moore7, Jennifer Hsiao8, Niki Grossheim2,9, Dalila Tremarias2,10, Ian Giles11 and Catherine Nelson-Piercy12
1Epilepsy Foundation, Birmingham, Alabama, USA
3The Spark Global, Buckinghamshire, UK
4Department of Dermatology, University Hospital Zurich, Zurich, Switzerland
5Department of Medicine, University of Zürich, Zurich, Switzerland
6Department of Neurology, St. Josef Hospital, Ruhr-University of Bochum, Germany
7Rheumatic & Musculoskeletal Disease Unit, Our Lady’s Hospice and Care Services, Harold’s Cross, Dublin, Ireland
8Department of Dermatology, Keck School of Medicine, University of Southern California, USA
9Myasthenia Gravis Holistic Society, Georgia, USA
10Lupus Europe, Brussels, Belgium
11Department of Medicine, Centre for Rheumatology, University College London, UK
12Guy’s and St Thomas’ NHS Foundation Trust, London, UK
*Corresponding Author: Sara Franklin,
Epilepsy Foundation, Birmingham,
Alabama, USA
E-mail: sarasfranklin@gmail.com
Received date: 28 February, 2024, Manuscript No. JWHIC-24-128500;
Editor assigned date: 01 March, 2024, PreQC No. JWHIC-24-128500 (PQ);
Reviewed date: 15 March, 2024, QC No. JWHIC-24-128500;
Revised date: 22 March, 2024, Manuscript No. JWHIC-24-128500 (R);
Published date: 01 April, 2024 DOI: 10.4172/2325-9795.1000487.
Citation: Franklin S, Bharadia T, Maul JT, Schneider-Gold C, Moore L, et al. (2024) Unmet Needs in the Healthcare Experience of Women of Childbearing Age with Chronic Disease and Recommendations for Change. J Womens Health 13:2.
Abstract
Research into the management of Chronic Disease (CD) during pregnancy is limited, with a lack of knowledge, evidence generation, and consensus on the medical outcomes for Women of Childbearing Age (WoCBA; 15-49 years) with CD. While some studies exist for specific CDs, there are few evaluations of the overlapping needs of WoCBA across multiple CDs. As such, we aimed to identify the common unmet needs for WoCBA with CD and generate recommendations for addressing them.
A social media listening study was conducted across Europe, the UK, and the USA and validated by a working group of patient representatives and healthcare professionals. Thematic analysis of the social media listening study revealed four areas of unmet need: (1) lack of patient support, (2) inadequate specialist discussions, (3) suboptimal coordination of the care pathway, and (4) need for empowering WoCBA with CD. Proposed solutions to enhance the patient experience included the co-creation of information resources, improved collaboration between specialist Healthcare Professionals (HCPs) as part of a multidisciplinary team, and the formation of peer support groups.
Keywords: Women’s Health; Chronic disease; Burden;
Practice recommendations; Pregnancy; Fertility; Hiradenitis
suppurativa; Rheumatoid arthritis; Psoriatic arthritis; Axial
spondyloarthritis; Ankylosing spondylitis; Epilepsy; Myasthenia
gravis
Introduction
People living with Chronic Diseases (CD) experience substantial physical, economic, and emotional burden [1]. Alongside being the leading cause of female mortality worldwide, chronic diseases are often debilitating, preventing or disrupting the pursuit of daily activities such as work, socializing, and family care, which in turn has an impact on economic and psychosocial wellbeing [2]. These challenges can be exacerbated during family planning and pregnancy [3].
Historically, pregnancy was discouraged for Women of Childbearing Age (WoCBA) with CDs due to the increased risk of complications and poor outcomes for mother and child. While consensus has shifted to be more supportive of pregnancy for WoCBA with CDs, risk of difficult pregnancies and poor-to-severe birth outcomes remains high when compared with the general population [4-7].
Furthermore, information is limited for WoCBA with CDs who are or wish to become pregnant and clear treatment plans for CD management during pregnancy are often lacking for both WoCBA and Healthcare Professionals (HCPs) [8]. Many treatments used for the management of CDs have limited data on safety for mothers and infants during and post-pregnancy, with only 5% of all drugs approved in the USA between 2003 and 2012 providing information on use during pregnancy [9].
As a result, WoCBA with CDs have reported feeling isolated and confused by a fragmented patient pathway, conflicting advice, and a lack of support from peers [10]. These individuals sometimes pursue self-initiated care routes such as halting medication, which can lead to negative impact on mental health and pregnancy outcome [11-14]. While some studies have characterized these unmet needs in the context of specific CDs and countries, there has not yet been a holistic evaluation of the overlapping needs common to WoCBA with CDs [15-20]. This study employed social media listening to identify common unmet needs among WoCBA with CDs and convened a multi-national panel of healthcare professionals and patients across multiple therapeutic areas to provide recommendations that address these unmet needs.
Materials and Methods
Social listening
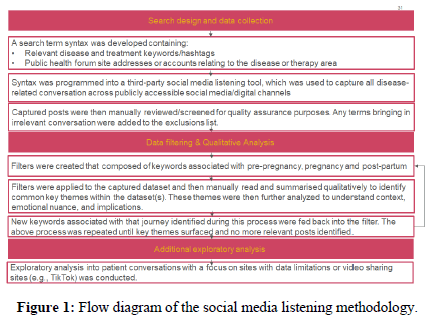
Social media listening methodology flow chart is represented with search design and data collection, data filtering and qualitative analysis and additional exploratory analysis as shown in Figure 1.
Using a combination of existing research and manual review of online conversations a list of search terms was created (Supplementary Tables). These terms consisted of keywords, expressions, hashtags, and public websites or accounts relating to Rheumatoid Arthritis (RA), Psoriatic Arthritis (PsA), Axial Spondyloarthritis/Ankylosing Spondylitis (AxSpa/AS), Epilepsy, Myasthenia Gravis (MG), and Hidradenitis Suppurativa (HS). Data were collected from France, Germany, Italy, Spain, the United Kingdom (UK) and the United States of America (USA), with terms translated and localized to the language(s) in each nation.
The search terms were used to identify and capture relevant posts authored between November 2020 and December 2022. Posts and sites were sourced across public social media accounts including YouTube, X (formerly Twitter), Instagram, TikTok and Facebook. Health-focused and parent/mother support forums, and blogs were then manually screened for quality assurance purposes to ensure the opinions and experiences of the target population were being captured sufficiently. Smart keyword filtering was used to separate posts into pre-pregnancy, pregnancy, and post-partum themes; filtered posts were manually reviewed to determine stakeholder relevance and context. Posts were then qualitatively reviewed to identify new keywords relevant to each search theme, which were then used to iterate the search filter to identify any additional posts of relevance from the initial dataset. Filtered posts were manually screened to identify common key themes. These themes were then further analyzed to understand context, emotional nuance, implications, and areas of unmet need. Additional, exploratory analysis into patient conversations with a focus on sites with data limitations or video sharing sites (e.g., TikTok) was conducted. These themes and unmet needs were validated by an online survey with a multidisciplinary working group of experts.
Expert working group round table
A multidisciplinary working group of experts comprising of HCPs and patient representatives was convened to provide recommendations on improvements of healthcare for WoCBA with CDs. The working group consisted of nineteen experts from Europe (n=12) and the USA (n=7). Participants included patient representatives (n=7) and HCPs (n=12); patient representatives had experience across different disease areas, including multiple sclerosis (n=1), psoriasis (n=1), epilepsy (n=1), myasthenia gravis (n=1), hidradenitis suppurativa (n=1), lupus (n=1), and ankylosing spondylitis (n=1). HCPs had specialist expertise in psychology (n=1), rheumatology (n=4), neurology (n=4), dermatology (n=2), and obstetrics (n=1). The round table session comprised of semi-structured, in-depth group discussions focused on unmet needs and solutions for the following periods: Pre-partum, pregnancy and post-partum. The advisory board was conducted in English online via Microsoft Teams in October 2022.
Ethical considerations
Informed consent was obtained from all working group participants before the advisory board. Participants were informed about the confidentiality of the data they provided, and the voluntary nature of their participation. All data were stored securely in accordance with international regulations and best practices.
Results
Unmet needs identified from social media listening
Social media data were collected from France, Germany, Italy, Spain, the UK, and the USA for WoCBA with CDs. Over 1.2 million publicly published posts were screened across Twitter (X), Instagram, TikTok, Facebook, blogs and forums (general, health or parent specific), with more than 2,600 attributable to WoCBA with CDs regarding pregnancy or childbirth. Thematic analysis of these data revealed four key areas of unmet need, which were validated with the expert working group. The themes were:
• Inadequate specialist discussions;
• Suboptimal coordination of the care pathway;
• Lack of patient support;
• Need for empowering WoCBA with CD.
Inadequate discussions with specialists, particularly around medication and disease management during pregnancy, was a common theme identified. Fears over whether medications would harm the infant, or how their condition may affect their pregnancy, were often raised on forums and on social media, with many WoCBA citing limited advice or discussions with their specialists. Others reported frustration of being advised to delay pregnancy until they achieved more stable disease and/or until a suitable washout period has passed after changing medication.
Relatedly, difficulties with discussing pregnancy with their physicians was a frequent barrier for WoCBA with CD. Some reported changing physicians due to lack of engagement with their goals for pregnancy, while others struggled or were reluctant to speak about treatment options surrounding pregnancy. Many posts were related to lack of trust or confidence in their HCP’s ability to support them during pregnancy.
Suboptimal coordination between different specialists was the second theme identified. Receiving conflicting advice and a perceived lack of motivation among HCPs to address problems outside of their specialty area were common, particularly regarding menstrual cycles, contraception, and pregnancy. WoCBA with CDs frequently posted about lack of communication between their specialists, with many feeling that they were required to piece together information themselves. Challenges with fragmented care pathways continued after childbirth, with mothers describing routine appointments where physicians were unaware of the effect of having a young child on disease management.
The third unmet need identified was lack of patient support. Posts relating to feelings of isolation, loneliness, depression, and uncertainty were common, especially with regards to pregnancy. Many WoCBA sought confirmation or reassurance from other people who had or were experiencing similar situations, with conception and breastfeeding as common topics. WoCBA often sought other women like them, who had similar experiences with their condition and social circumstances. Other common challenges were related to communication with families around safety of medication use and challenges in family life with young children and in the workplace.
The final theme identified was a need to empower WoCBA with CD to have greater agency surrounding pregnancy, childbirth, and raising a family. Many of the posts screened described uncertainty in whether they would be able to conceive, whether their child would inherit their condition, the safety of medications during pregnancy and breast feeding, how to manage their condition during pregnancy, and how to manage life with a young family. Where advice was shared between patients, it was often not clinically robust.
Recommendations for addressing unmet needs from the expert working group
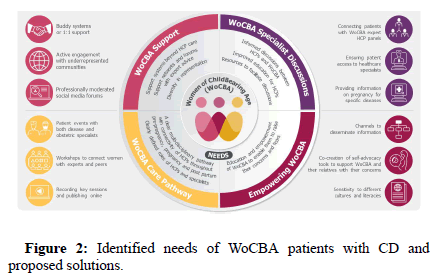
Recommendations from the expert working group for addressing unmet needs are summarized in Table 1 and Figure 2. Verbatim recommendations from the expert working group are also provided. Commentary from the expert working group is shown alongside each of the themes identified.
| Key unmet needs | Solution | Recommendations |
|---|---|---|
| Inadequate specialist discussions | Integrate resources for HCPs into their training |
|
| Design apps for HCPs to facilitate information sharing |
|
|
| Assemble dedicated multidisciplinary health teams |
|
|
| Suboptimal coordination of the care pathway | Improve access to information by convening events/workshops |
|
| Lack of patient support | Create social media forums with expert advice and professional moderators |
|
| Improve diversity in representation |
|
|
| Facilitate support groups and meetings |
|
|
| Ensure emotional and mental health support |
|
|
| Need for empowering WoCBA with CD | Develop resources for patients |
|
| Design apps for patients |
|
|
| Support evidence generation |
|
Table 1: Recommended solutions to key unmet needs of women of childbearing age with chronic disease.
Inadequate specialist discussions
Three potential solutions are proposed to address inadequate specialist discussions: 1) Integrate resources for HCPs into their training; 2) Design apps for HCPs to facilitate information sharing; and 3) Assemble dedicated multidisciplinary health teams. HCP and patient knowledge are key factors in determining the quality of discussions occurring between these two parties, with many patients feeling burdened by having to start discussions without specialist knowledge of their CD and pregnancy and many HCPs feeling uncomfortable in having any conversations on the topic. As such, educational materials and integrated training for HCPs could enable both parties to improve the quality of discussion during consultations. In a similar fashion, greater uptake of electronic health records and/or development of apps and software to enable sharing of patient data and information between specialists would facilitate discussions on pregnancy and contraception.
Given the complexity of CD management and pregnancy, in addition to the patient’s CD specialist physician, a dedicated reproductive health Multidisciplinary Team (MDT) is recommended alongside the usual CD care team. This MDT should include an obstetric physician, a reproductive medicine specialist, and a single point of contact, such as a patient navigator or specialist nurse to help manage misinformation and navigate patients through their journey.
Suboptimal coordination of the care pathway
As an extension of the above recommendations, creating greater understanding for WoCBA and between HCPs of the roles of each specialty and how they connect to form the care pathway is a critical step for improving pregnancy care for WoCBA with chronic diseases. Convening events, live or online, for WoCBA, patient organizations, and HCPs to share learnings and ideas through panel discussions and networking sessions would allow dissemination of information. Such events could be hosted at the local or regional level by healthcare organizations.
Lack of patient support
Many WoCBA rely on social media to connect with peers and seek advice about managing their condition during pregnancy. While in this respect, social media is an important tool to bolster patient support, it comes with the risk of unsubstantiated and poor advice (experience of the patient representatives in the expert working group). Professional moderation and medical input, preferably from a qualified HCP, is critical to ensure the scientific validity of information and to stem the flow of false or inaccurate information while maintaining the valuable support function of social media. While moderating social media forums would be time-consuming for already stretched individual HCPs, a dedicated external group or facilitator, such as a hospital, could be responsible for running such forums.
Beyond social media, ensuring access and signposting to local inperson support groups and mental health services is recommended. Improving HCP awareness of the available mental health services and resources would in turn allow HCPs to encourage patients to seek mental health support and provide information. Furthermore, developing a ‘buddy system’ for peer support through existing services could provide emotional support to patients. Activating patients to volunteer to organize events could address existing challenges surrounding access to mental health services (experience of the expert working group).
Beyond moderation of scientific accuracy, enabling participation for all WoCBA in social forums and groups, whether online or inperson is imperative. Patients can feel isolated or unable to engage, particularly if they don’t feel represented in a group (experience of patient representatives in the expert working group). Creating welcoming and safe environments that embrace diversity across all axes (such as ethnicity, age, faith, and socio-economic background) through a ‘bottom-up’ approach was recommended, where healthcare organizations (for example, patient advocacy organizations or hospitals) and HCPs reach out to community leaders of underrepresented groups, inviting perspectives and input on how to best include all members of the community.
Need for empowering WoCBA with CD
WoCBA with CD expressed a need for encouragement to bolster their confidence in the ability to raise their concerns and to request information during pre-pregnancy, pregnancy, childbirth, and the postpartum period in conversation with their HCPs. Developing a symptom tracker app linked to a patient’s records could facilitate information sharing and care continuity between HCPs, reducing the burden on WoCBA to raise issues and enabling conversations. While not suitable for all patients, such a tool would enable patients to feel more informed of their condition.
Beyond enabling WoCBA with CD to track the course of their symptoms and disease management, supporting greater understanding of their disease and treatment options could enable engagement in shared decision-making. Resources could include leaflets explaining clinical data, a roadmap to illustrate disease progression and the care pathway, discussion guides to support patients’ conversations with their families and HCPs, and medical vocabulary cheat sheets, and should include a mix of educational material and practical advice. These resources should be developed or co-developed by patient organizations, who should also take an active role in providing resources and information on pregnancy for their specific disease area. Resources should be easy to use, easy to understand, discoverable and accessible, regularly updated, and scientifically validated by HCPs and professional organizations.
Discussion
The central unmet needs identified here are supported by publications exploring the concerns of WoCBA with rheumatoid arthritis, multiple sclerosis, cystic fibrosis and lupus [21-25]. Chief amongst these concerns is lack of patient support, where women with chronic medical conditions often feel as though they are messengers between different healthcare specialists [26]. This lack of support also plays a central role in many subsequent challenges, including misunderstandings around healthcare recommendations and the safety of available treatment approaches. Our findings support the notion that patients’ interests in the harms and benefits of their treatment are aligned to the same concerns as their HCP, though they need guidance in how to address these questions [27].
Furthermore, without adequate support and knowledge, WoCBA with CD may opt to remain childless, even in cases where there is a personal desire for parenthood and no medical contraindication to pregnancy. For example, in a study of women with Systemic Lupus Erythematosus (SLE), 53.7% (51/95) were childless; 21% (11/51) of whom were voluntarily, 6% (n=3/51) of whom indicated that the decision was based on medical advice from their HCP, and 4% (2/51) of whom indicated that their infertility was attributed to medication use [28]. These prior data support our finding that many WoCBA across multiple CDs feel uncertainty surrounding pregnancy and management of their condition. Recent work by Krysko et al., aligns with our recommendations, encouraging HCPs managing multiple sclerosis to initiate proactive discussions with WoCBA with CD and help them to voice their concerns in order to find a psychological balance between risks of treatment, potential worsening of the disease course, and implications of pregnancy [29]. Recommendations for a holistic approach to family planning for WoCBA with lupus include incorporation of information and resources for how to manage lupus during pregnancy but also timely, accurate, and easily accessible information on pre-pregnancy pregnancy planning and birth choices [30]. While these recommendations were created for the management of lupus, many have broader applicability to WoCBA with other CDs.
In addition, WoCBA with CD express a strong desire to hear about and learn from the experiences of peers, while in parallel they want their HCPs to help them navigate the healthcare system and to delineate a clear, easily comprehensible care pathway. This level of support should continue post-partum, covering specialized maternity care topics such as breastfeeding. Without this knowledge or appropriate advice, WoCBA with CD generally consider there to be only two courses of action: To stop breastfeeding or stop medication, either of which may be avoidable with appropriate HCP guidance [31]. Enabling greater education and support, as outlined in the recommendations above, is a critical step in improving outcomes and experiences for WoCBA with CD.
While this research and recommendations focuses on the needs of WoCBA with CDs, it is crucial that the wider community of support around them, including partners, caregivers, and family members are also adequately informed, so that they are equipped to have an informed dialogue and empower WoCBA with CDs in their decisions [32]. Additionally, stakeholders across the healthcare ecosystem, including regulatory and research organizations and pharmaceutical companies, should strive to increase research into the legitimacy of recommending or contraindicating CD medication during pregnancy and breastfeeding. WoCBA with CD should be encouraged by HCPs to report adverse events associated with their medications to enable monitoring and greater understanding of medication use during pregnancy. Furthermore, research into long-term outcomes of children of women with CDs exposed to medications should be encouraged and supported.
This research combines insights gathered from social listening and expert opinion to identify unmet needs across various CDs bridging several medical specialties and provide recommendations. Unlike many previous studies, this work involved close collaboration between HCPs from different medical specialties and patients and investigated commonalities between multiple diseases across multiple geographies. As such, the common themes identified here are likely to have broad applicability to many CDs. Limitations of the study include restriction of the social listening and working group to participants from European countries and the US, which are high-income countries, and involvement of predominantly Caucasian participants.
Conclusion
We present a holistic view of unmet needs among WoCBA across multiple CDs surrounding pregnancy and provide recommendations for ways to address them. Common efforts that would benefit multiple patients across various disease conditions would be the establishment of moderated online and in-person support services to reduce misinformation and provide platforms for communication between patients, development of educational resources for patients and HCPs, and creation of tools to enable discussion between WoCBA with CDs and their HCPs. Such efforts require concerted involvement of healthcare providers, the pharmaceutical industry, and patient organizations to work together and improve the current state of reproductive healthcare for WoCBA with CD.
Competing Interests
Sara Franklin has participated in advisory boards for UCB and has served as a member of staff for the Epilepsy Foundation.
Trishna Bharadia has received consulting and/or speaking fees from Abbvie, 67 Health, Admedicum, A Life in a Day (The Method), Becaris Publishing, Bristol Myers Squibb, Boehringer Ingelheim, Clara Health, Gilead, Heel Pharma, IDEA Pharma, Medable, Medidata, Medipace, Merck KGaA, Novartis, Parexel, Pfizer, Queen Mary University London, Roche, Sandoz, Savvy Cooperative, Talking Medicines, Teva, UCB, Worldwide Clinical Trials, Professional Record Standards Body (PRSB), Karger Publishers, MSD, Trilogy Writing, Insmed UK, Protas, International Society for Medical Publications Professionals (ISMPP), Ethos Pharmaceutical, Open Health, Alira Health, Curebase, Kings College London, and National Institute for Health Research. TB has also served in roles in the MS Society, Asian MS, and International Society for Medical Publications Professionals (ISMPP), and TB has received support for travel from Siro ClinPharm.
Julia-Tatjana Maul has served as an advisor and/or received speaking fees and/or participated in clinical trials sponsored by AbbVie, Almirall, Amgen, BMS, Celgene, Eli Lilly, LEO Pharma, Janssen-Cilag, MSD, Novartis, Pfizer, Pierre Fabre, Roche, Sanofi, and UCB.
Christiane Schneider-Gold has received consulting and/or speaking fees from Alexion Pharmaceuticals, Amicus Therapeutics, Argenx, Hormosan Pharma, Immunovant, Lupin Pharmaceuticals, Roche, Sanofi-Genzyme, and UCB Pharma. CSG has also participated in advisory boards for Alexion Pharmaceuticals, Argenx, Hormosan Pharma, Immunovant, Lupin Pharmaceuticals, Roche, Sanofi- Genzyme, and UCB, and has received travel support from Alexion.
Louse Moore has received speaking fees from UCB and support for meeting attendance from Nordic Pharma.
Jennifer Hsiao has received consulting and/or speaking fees from AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, and UCB. JH has also served on the board of directors for the Hidradenitis Suppurativa Foundation.
Niki Grossheim has served as a board member for the Myasthenia Gravis Holistic Society.
Dalila Tremarias has received speaking fees from Otsuka and UCB. DT has served in roles for Lupus Europe, Lupus UK, NHS Ethics Committee, and Welsh Blood Panel.
Ian Giles has received funding and speaking fees from UCB, royalties from Elsevier, and has served on the British Society of Rheumatology Working Group on prescribing anti-rheumatic drugs in pregnancy.
Catherine Nelson-Piercy has received consulting and/or speaking fees from UCB, Sanofi, and Otsuka. CNP is a medical advisor for the pregnancy sickness support charity and is a patron of the Lauren Page Trust.
Funding
UCB Biopharma SRL funded the publication of this manuscript and provided data as a stimulus for an advisory board, from which the authors developed this manuscript.
Role of The Funder
The advisory board upon which this manuscript was based was initiated and funded by UCB Biopharma SRL and organized by Medical Consulting at VML Health (London, UK) in partnership with UCB. UCB had no influence on the authorship of this publication.
Acknowledgements
The authors would like to extend sincere thanks to Brindley Brooks, Rebecca Bromley, Megan Clowse, Zakieyah Davids, Linzi Dunlevy, Kelly Fraser, Hellen Wangui Gathere, Kimford Jay Meador, Bettina Schmitz, Jessica Smith, and Angela Tincani for their value contribution to the working group, and to Ágnes Koncz from UCB for instigating and funding this advisory board. Laura Galimam from Lumanity, and Maryam Sidat and James Camp from VML Health supported with the preparation of the manuscript.
References
- Ansah JP, Chiu CT (2023) Projecting the chronic disease burden among the adult population in the United States using a multi-state population model. Front Public Health 10:1082183.
[Crossref] [Google Scholar] [Pubmed]
- MBRRACE-UK. Lessons Learned to Inform Maternity Care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2019-21.
- Houtum LV, Rijken M, Groenewegen P (2015) Do everyday problems of people with chronic illness interfere with their disease management? BMC Public Health 15(1):1-9.
[Crossref] [Google Scholar] [Pubmed]
- Leibowitz U, Antonovsky AA, Kats RA, Alter MI (1967) Does pregnancy increase the risk of multiple sclerosis? J Neurol Neurosurg Psychiatry 30(4):354.
[Crossref] [Google Scholar] [Pubmed]
- Munoz SR, Lupattelli A, De Vries ST, Mol PG, Nordeng H (2020) Differences in medication beliefs between pregnant women using medication, or not, for chronic diseases: A cross-sectional, multinational, web-based study. BMJ Open 10(2):e034529.
[Crossref] [Google Scholar] [Pubmed]
- Jovanovic L, Pettitt DJ (2007) Treatment with insulin and its analogs in pregnancies complicated by diabetes. Diabetes Care 30(Supplement_2):S220-S224.
[Crossref] [Google Scholar] [Pubmed]
- Kersten I, Lange AE, Haas JP, Fusch C, Lode H, et al. (2014) Chronic diseases in pregnant women: Prevalence and birth outcomes based on the SNiP-study. BMC Pregnancy Childbirth 14(1):75.
[Crossref] [Google Scholar] [Pubmed]
- Firoz T, Pineles B, Navrange N, Grimshaw A, Oladapo O, et al. (2022) Non-communicable diseases and maternal health: A scoping review. BMC Pregnancy Childbirth 22(1):787.
[Crossref] [Google Scholar] [Pubmed]
- Riley L, Cahill A, Beigi R, Savich R, Saade G (2017) Improving Safe and Effective Use of Drugs in Pregnancy and Lactation: Workshop Summary. Am J Perinatol 34(08):826-832.
[Crossref] [Google Scholar] [Pubmed]
- Williams C, Johnson B, Middleton PG, Becker V, Gibson PG, et al. (2021) Family planning, pregnancy and birth in women with lung conditions: A worldwide survey. ERJ Open Res 7(4):00357-02021.
[Crossref] [Google Scholar] [Pubmed]
- Birmingham Health Partners (2022) Healthy Mum, Healthy Baby, Healthy Future: The Case for UK Leadership in the Development of Safe, Effective and Accessible Medicines for Use in Pregnancy.
- MBRRACE-UK. Lessons Learned to Inform Maternity Care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2017-19.
- Cantwell R (2021) Mental disorder in pregnancy and the early postpartum. Anaesthesia 76(S4):76-83.
[Crossref] [Google Scholar] [Pubmed]
- Aker AM, Vigod SN, Dennis C-L, Brown HK (2022) Perinatal Complications as a Mediator of the Association Between Chronic Disease and Postpartum Mental Illness. J Womens Health (Larchmt) 31(4):564-572.
[Crossref] [Google Scholar] [Pubmed]
- Shoela S, Beltagy A, Fayed F, Morsy M (2020) Sat0642-hpr capturing the unmet needs of women with systemic lupus erythematosus and identifying the information needed in physician-patient communication. Ann Rheum Dis 2020;79(Suppl 1):1280.
- López-Reyes L, Guío-Sánchez C, González-Uribe C, Cárdenas-Robledo S (2022) Fertility preferences and unmet need for family planning in women with multiple sclerosis. Front Neurol 13:1035595.
[Crossref] [Google Scholar] [Pubmed]
- Luo S, Yan J, Yang D, Xiong S, Wang C, et al. (2022) Current practice, attitude and views of providing pregnancy care for women with type 1 diabetes in China: A qualitative study. BMJ Open 12(11):e061657.
[Crossref] [Google Scholar] [Pubmed]
- Chimenti M-S, Alten R, D’Agostino M-A, Gremese E, Kiltz U, et al. (2021) Sex-associated and gender-associated differences in the diagnosis and management of axial spondyloarthritis: Addressing the unmet needs of female patients. RMD Open 7(3):e001681.
[Crossref] [Google Scholar] [Pubmed]
- De Simone C, Calabrese L, Balato A, Cannavò SP, Dattola A, et al. (2020) Psoriasis and its management in women of childbearing age: Tools to increase awareness in dermatologists and patients. G Ital Dermatol Venereol 155(4);434-440.
[Crossref] [Google Scholar] [Pubmed]
- Tsentemeidou A, Sotiriou E, Bakirtzi K, Papadimitriou I, Chatzi-Sotiriou T, et al. (2023) Quality-of-life endpoints in women of childbearing age with hidradenitis suppurativa: A tertiary-care-centre-based study. Mediterr J Rheumatol 34(4):469-478.
[Crossref] [Google Scholar] [Pubmed]
- Chew C, Rebić N, Baldwin C, Amiri N, Proulx L, et al. (2019) “r/Thritis”, Pregnancy, and Parenting: A Qualitative Descriptive Study of Reddit Forums to Explore Information Needs and Concerns of Women with Rheumatoid Arthritis. ACR Open Rheumatol 1(8):485-492.
[Crossref] [Google Scholar] [Pubmed]
- Phillips R, Pell B, Grant A, Bowen D, Sanders J, et al. (2018) Identifying the unmet information and support needs of women with autoimmune rheumatic diseases during pregnancy planning, pregnancy and early parenting: Mixed-methods study. BMC Rheumatol 2(1):21.
[Crossref] [Google Scholar] [Pubmed]
- Kosmala-Anderson J, Wallace LM (2013) A qualitative study of the childbearing experience of women living with multiple sclerosis. Disabil Rehabil 35(12):976-981.
[Crossref] [Google Scholar] [Pubmed]
- Holton S, Fisher J, Button B, Williams E, Wilson J (2018) Childbearing concerns, information needs and preferences of women with cystic fibrosis: An online discussion group. Sex Reprod Healthc 19:31-35.
[Crossref] [Google Scholar] [Pubmed]
- Adelekun AA, Villa NM, Hsiao JL, Micheletti RG (2020) Pregnancy in Hidradenitis Suppurativa-Patient Perspectives and Practice Gaps. JAMA Dermatol 157(2):227.
[Crossref] [Google Scholar] [Pubmed]
- Hansen MK, Midtgaard J, Hegaard HK, Broberg L, de Wolff MG (2022) Monitored but not sufficiently guided–A qualitative descriptive interview study of maternity care experiences and needs in women with chronic medical conditions. Midwifery 104:103167.
[Crossref] [Google Scholar] [Pubmed]
- Feeney T, Villanueva T, Price A (2023) Communicating the benefits and harms of anticancer drugs. BMJ 380:623.
[Crossref] [Google Scholar] [Pubmed]
- Blomjous BS, de Vries JIP, Zijlstra E, Cramer K, Voskuyl AE, et al. (2021) Desire to have children and preferences regarding to pre-pregnancy counselling in women with SLE. Rheumatology 60(6):2706-2713.
[Crossref] [Google Scholar] [Pubmed]
- Krysko KM, Dobson R, Alroughani R, Amato MP, Bove R, et al. Family planning considerations in people with multiple sclerosis. Lancet Neurol 22(4):350-366.
[Crossref] [Google Scholar] [Pubmed]
- Marder W (2019) Update on pregnancy complications in systemic lupus erythematosus. Curr Opin Rheumatol 31(6):650-658.
[Crossref] [Google Scholar] [Pubmed]
- Scime NV, Lee S, Jain M, Metcalfe A, Chaput KH (2021) A Scoping Review of Breastfeeding in Women with Chronic Diseases. Breastfeed Med 16(11):851-862.
[Crossref] [Google Scholar] [Pubmed]
- Anders S, Aaron H, Jackson GP, Novak LL (2019) Supporting Caregivers in Pregnancy: A Qualitative Study of Their Activities and Roles. J Patient Exp 6(2):126-132.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi