Case Report, Clin Oncol Case Rep Vol: 6 Issue: 5
A Case Study on Two Primary Cancer of Non-Hodgkin's Lymphoma Together with Lung Squamous Cell Carcinoma
Mohammed Alnaggar1,2*, Xue Yang3, Wei wei Huang2
1Department of Internal Medicine, Clinic Medical College, Hubei University of Science and Technology, Xianning, Hubei, China.
2Department of Oncology, South Hubei Cancer Hospital, Xinning, Hubei, China. 437000.
3Gongan Hospital of Traditional Chinese Medicine, Jingzhou City, Hubei, China.
*Corresponding Author: Mohammed Alnaggar
Department of Internal Medicine
Clinic Medical College, Hubei University of Science and Technology, Xianning, Hubei, China.
E-mail: dr.alnaggar@hotmail.com
Received: May 18, 2023; Manuscript No: COCR-23-99947;
EditorAssigned: May 20, 2023; PreQC Id: COCR-23-99947 (PQ);
Reviewed:May 27, 2023; QC No: COCR-23-99947 (Q);
Revised: May 28, 2023;Manuscript No: COCR-23-99947 (R);
Published: May 31, 2023; DOI: 10.4172/cocr.6(5).290
Citation: Alnaggar M, Yang X, wei Huang W (2023) A Case Study on Two Primary Cancer of Non-Hodgkin's Lymphoma Together with Lung Squamous Cell Carcinoma. Clin Oncol Case Rep 6:5
Abstract
Multiple Primary Cancer (MPC) is repetitive cancer with two or more primary malignant tumors occurring simultaneously or successively in a single organ or multiple organs of the same host. We discuss the treatment strategy for Non-Hodgkin's Lymphoma with Lung Squamous Cell Carcinoma, which has been increasing in recent years, and include epidemiological considerations.
Keywords: Non-Hodgkin's Lymphoma; Lung squamous cell carcinoma; Double primary cancer
Introduction
Non-Hodgkin's lymphoma, a heterogeneous group of lymphoid malignancies, has been extensively studied. It arises from lymphoid tissues and is characterized by abnormal lymphocyte proliferation. Lung squamous cell carcinoma, on the other hand, is one of the major histological subtypes of Non-Small Cell Lung Cancer (NSCLC) and accounts for a significant proportion of lung cancer cases worldwide [1].While the coexistence of primary NHL and lung SCC in a single patient is a rare occurrence, it highlights the importance of comprehensive diagnostic evaluation and individualized treatment planning. Understanding the underlying mechanisms and risk factors associated with the development of multiple primary malignancies can provide insights into the complex interplay of genetic, environmental, and lifestyle factors contributing to cancer development [2].
This case study aims to present a detailed analysis of the clinical presentation, diagnostic workup, treatment modalities, and patient outcomes in a unique scenario of concurrent NHL and lung SCC. By examining this case, healthcare professionals can enhance their knowledge and improve patient management strategies in similar clinical scenarios.
Case Presentation
A 67-year-old male with a smoking history of more than 20 years (40 cigarettes daily). The patient was diagnosed in March 2020 with left tonsil enlargement ( III0). Due to the outbreak of COVID-19, the patient did not receive any treatment. Till Oct. 19, 2020, the patient got treatment in our hospital. Chest enhanced contrast CT scan shows a space-occupying lesion in the inferior lobe of the right lung. Nasopharynx perfusion enhanced contrast MRI and left neck soft tissue MRI shows a tumorous lesion in the left pharynx wall and parapharyngeal region, together with left neck lymph node enlargement (Figures 1 and 2). Pathology of right lung spaceoccupying lesion indicates non-keratinizing squamous cell carcinoma (T2N0M0 IB Stage). On Nov. 13, the patient underwent neck tumor resection and biopsy under general anesthesia. Its pathology shows (neck tumor tissue) non-Hodgkin's Lymphoma (invasion type, nongerminal center type), which is considered as diffuse large-B cell lymphoma (Figure 3) Stage I. This patient received two cycles of R-CHOP chemotherapy. After chemotherapy, the patient developed grade IV myelosuppression. The follow-up MRI showed that the mass in the mandible was bigger than before, and the patient's disease progression was considered. After MDT discussion, R-CHOP + etoposide chemotherapy was recommended, then do radiotherapy. The patient and his family refused chemotherapy and requested radiotherapy for the left submandibular mass.
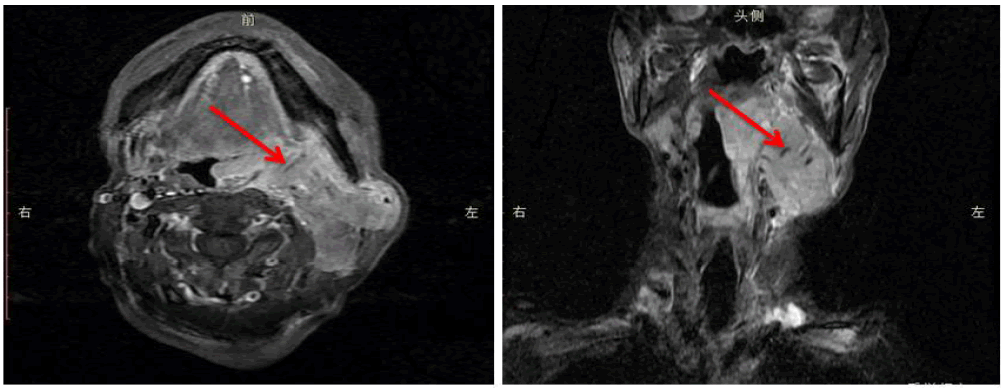
Figure 1: An irregular poorly-defined tumor with a soft tissue signal protruding to the pharyngeal cavity is seen in the left pharynx wall of the oropharyngeal region. The left eustachian tube is narrowed. A rare soft tissue tumor is seen in the left parapharyngeal region. Perfusion enhanced contrast scan: uneven enhancement is detected in the tumor of the left pharynx and parapharyngeal region. Moderate ring-shaped enhancement is detected in a neck lymph node.
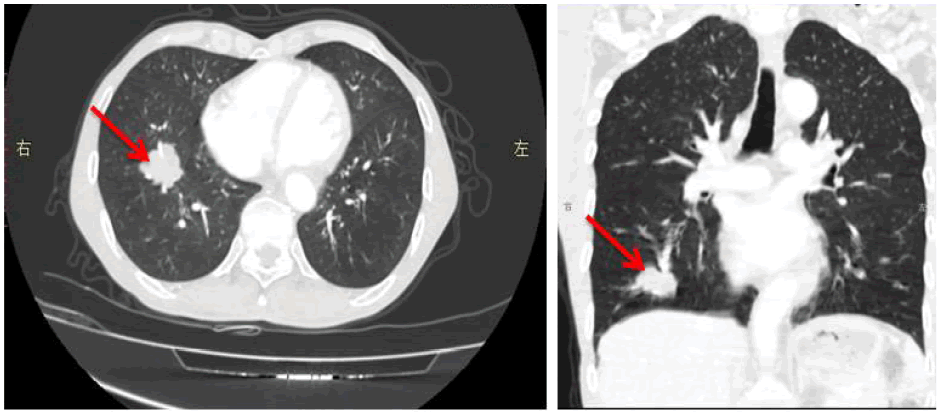
Figure 2: Chest enhanced contrast CT scan shows a lobulated tumor measuring 35 mm*31 mm in the inferior lobe of the right lung.
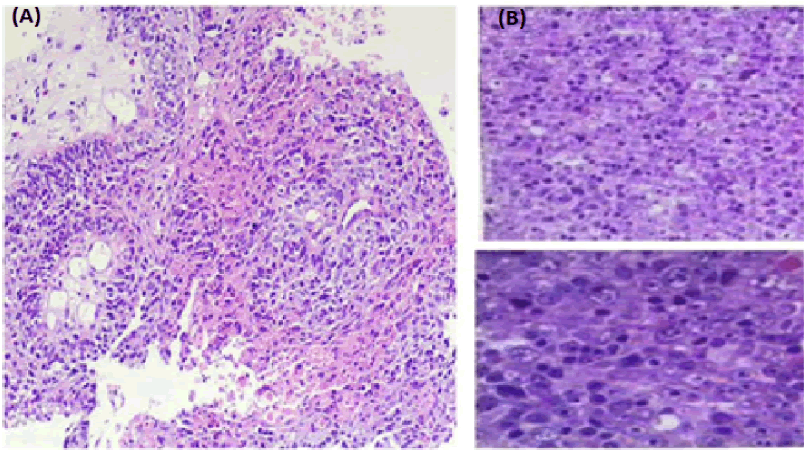
Figure 3:(A) Pathology of right lung space-occupying lesion: non-keratinizing squamous cell carcinoma. Immunohistochemistry: P40 (+), CK5/6 (+), CK7 (-), TTF-1 (-), Syn (-), CD56 (-), P53 (mutant type), Ki67 (+, around 25%). (B) pathology of neck tumor resection and biopsy: (neck tumor tissue) non-Hodgkin's lymphoma (invasion-type, non-germinal center) which is considered as diffuse large-B cell lymphoma. Immunohistochemistry: Tumorous cell CD20 (+, positive control+), CD19 (+), CD22 (+), BCL2 (about 100%+), BCL6 (about 5%+), CD23 (+), C-MYC (about 60%+), MUM (about 90%+), CD43 (+), P53 (+, mutant type), CD3 (-), CD5 (-), CD10 (-), CyclinD1 (-), CD21 (-), CD30 (-, positive control+), PCK (-), P40 (-), CK5/6 (-), TTF-1 (-), NapsinA (-), ALK(D5F3) (-, positive control +, negative control-), Ki-67 LI; around 80%. Molecular pathology: EBERCISH (-, positive control+).
Discussion
At present, multiple primary cancers still need confirming by the following diagnostic criteria once proposed by IARC[1]; (1). The detection of two or more primary tumors is not time-dependent;(2). A primary cancer is defined as one that begins in a primary place or tissue and is not an extension, recurrence, or metastasis;(3). Only one tumor per organ, pair of organs, or tissue shall be recognized;(4). Rule 3 is inapplicable in two instances: 1. Individuals are only counted once for systemic (or multicentric) malignancies that may involve multiple organs; 2.Multiple malignancies should be considered neoplasms with distinct morphologies (even if they are diagnosed simultaneously at the same site). Multiple primary cancers are common in double cancer and less in triple cancer and above. In recent years, with the unceasing advancement of diagnosis and treatment technology and the prolonged survival period of patients with malignant tumors, multiple primary cancers' incidence tends to increase [2, 3]. However, the current incidence rates differ from countries, from 0.73% to 11.70% abroad and about 2.67% in China [4, 5]. Due to rich lymphoid tissues, the neck is believed as a common pathogenic site of non- Hodgkin's Lymphoma (NHL), and the incidence rate has shown a pronounced increase in recent years. This thesis demonstrates a rare case of double primary cancer of non-Hodgkin's Lymphoma together with lung squamous cell carcinoma [6-9].
Multiple primary cancers have shown a continuous increase in clinical cases in recent years. Among the people with confirmed malignant tumors, the incidence of multiple primary cancers is between 2% and 17% [10]. The longer the follow-up period after diagnosis is, the more likely it is to discover the second malignant tumor. The incidence rate can reach as high as 17% within 20 years of follow-up [10-11]. The onset of multiple primary cancers is a process involving multiple factors, multiple genes, and multiple steps.
The most famous "regional cancerization" theory and many related studies of MPC have shown that after tumors occur in cancerous areas, the risk of new tumor recurrence is higher than that of non-tumor populations , studies have concluded that the causes of multiple primary cancers mainly include multiple risk factors like immune deficiency and escape of cancer cells, living environment factors smoking, alcoholism, obesity [12,13]. Besides that, there is evidence that unhealthy lifestyle, age, some anti-cancer treatments can also increase the risk of multiple primary cancers. The pathogenesis of MPC is considered to be related to the following factors: 1. With the improvement of medical level, the life expectancy of the population increases, and swelling occurs in old age, increasing the likelihood of neoplasia; 2. Genetic susceptibility; 3. The proximity of carcinogenic factors to similar tissue structures Organs have the same carcinogenic effects; 4.Chemical drugs and radioactive substances used to treat the first primary tumor have carcinogenic effects on other organs [14-16]. Diffuse large B-cell lymphoma is the most common pathological type of non-Hodgkin's Lymphoma. The head and neck are the second most likely position of lymphoma occurrence, of which diffuse large B-cell Lymphoma of the head and neck (HN-DLBCL) is the most common invasive malignant B-cell Lymphoma. As shown in the results of TAKANO's research [17,18], HN-DLBCL generally occurs in nonreproductive ages, with a higher proportion of males than that females. The most common site of HN-DLBCL occurrence is the oropharynx, followed by the cervical lymph nodes. The patient in the case above was diagnosed with right lung squamous cell carcinoma and neck non-Hodgkin lymphoma in the same month. The two cancers are simultaneous multiple primary cancer. Most studies feel that many primary tumors have a similar prognosis to single malignant tumors and even have a much longer survival period [19]. Numerous data indicate that patients with multiple primary malignancies can survive for an extended period [20]. Multiple primary cancers have different clinical manifestations due to different types of tumors, and it is easy to overlook another primary lesion during the diagnosis process, resulting in missed diagnosis. At present, there is no uniform standard of the treatment plan for MPC, but whether it is a patient with simultaneous MPC or metachronous MPC, simultaneous surgery, or complete excision of each lesion one by one is believed as the first choice of treatment. Due to the individualized characteristics, MPC patients often adopt multidisciplinary discussions and treatment plans to maximize their survival benefits. At present, many pieces of literature highly recommend radical treatment methods, mainly including surgery, radiotherapy, and chemotherapy based on tumor pathology type, tumor position, and general conditions of patients with MPC. The distance between the two tumors also dramatically impacts the treatment plan selection. If the two tumors are far apart, the patient can receive the treatments such as surgery or radiotherapy and chemotherapy for one primary tumor, which may have a more negligible effect on the second primary tumor; if the two tumors occur close to each other. Considering the potential postoperative adhesions and anatomical changes caused by the surgical treatment of a single tumor and the influence of radiotherapy and chemotherapy on the tissue structure and blood supply, conservative treatments such as radiotherapy or chemotherapy are often adopted to treat the second tumor. Suppose surgery cannot be selected during treatment. In that case, it is generally considered that the lesion with the most significant physiological impact and the most prominent symptoms are the main symptoms, and active anti-cancer treatment can be carried out to prolong the survival of patients. Epidemiological data on lymphoma in patients with lung cancer is unclear, Lung cancer with lymphoma is even rarer, Van Leeuwen et al.counted 744 cases of Hodgkin's lymphoma over 18 years, with 14 subsequent lung cancer cases [21] ,the risk of lung cancer was associated with high-dose radiotherapy, although all lung cancers occurred in non-radiation sites. Studies conducted a retrospective analysis of 29,153 patients with Non- Hodgkin's lymphoma and found that radiotherapy increased the risk of lung cancer [22], It was also reported that 6 cases of lung cancer were found in 655 patients with HL or NHL who were followed up [23].
Conclusion
This case study aims to from the in-depth learning of multiple primary cancers. We should be satisfied with the first diagnosis and need endeavor to know the patient's medical history in detail, do a thorough physical examination, adhere to follow-up results, and perfect all aspects of examination to minimize the rate of missed diagnosis clinically.
Author Contribution
These authors contributed equally to this work.
References
- Report WG (2005) International rules for multiple primary cancers (ICD-0 third edition). Europ J Cancer Prevent 14: 307-308. [Google Scholar] [Cross Ref]
- Salem A, Abu-Hijlih R, Abdelrahman F, Turfa R, Amarin R, et al. (2012) Multiple primary malignancies: Analysis of 23 patients with at least three tumors. J Gastrointes Can 43: 437-443. [Google Scholar] [Cross Ref]
- Bittorf B, Kessler H, Merkel S, Bruckl W, Wein A, et al. (2001) Multiple primary malignancies: An epidemiological and pedigree analysis of 57 patients with at least three tumours. Europ J Surg Oncol 27: 302-313. [Google Scholar] [Cross Ref]
- Izmajlowicz, B., Kornafel, J., & BÅ?aszczyk, J. (2014). Multiple neoplasms among cervical cancer patients in the material of the lower Silesian cancer registry. Adv Clin Exp Med 23: 433-440. [Google Scholar] [Cross Ref]
- Fu J, Huang Z, Lin Y, Xiao B. (2013) Clinical analysis of 39 cases of multiple primary colorectal carcinoma. J South Med Uni 33: 578-581. [Google Scholar] [Cross Ref]
- Tokuchi Y, Kamachi M, Harada M, Hasegawa M, MlSHINA T, et al. (2003) Synchronous triple lung cancers after treatment for non-Hodgkin's lymphoma: Metachronous quadruple cancers. Internal Med 42: 1031-1034. [Google Scholar] [Cross Ref]
- De Giacomo T, Martelli M, Venuta F, Anile M, Diso D, et al. (2006) Lung cancer after treatment for non-Hodgkin lymphoma. Minerva Chirurgica 61: 467-471. [Google Scholar] [Cross Ref]
- Kawashima O, Sakata S, Kamiyoshihara M, Maeshima A, Ishikawa S, et al. (1999) Primary pulmonary collision tumor including squamous cell carcinoma and T-cell lymphoma. Lung Cancer 23: 67-70. [Google Scholar] [Cross Ref]
- Zhang Y, Li G, Zhuang H (2008) Unsuspected synchronous lung cancer unveiled on FDG PET after chemotherapy for non-Hodgkin lymphoma. Clin Nuclear Med 33: 109-110. [Google Scholar] [Cross Ref]
- Vogt A, Schmid S, Heinimann K, Frick H, Herrmann C, et al. (2017) Multiple primary tumours: Challenges and approaches, a review. ESMO Open 2: e000172. [Google Scholar] [Cross Ref]
- Wood ME, Vogel V, Ng A, Foxhall L, Goodwin P, et al. (2012) Second malignant neoplasms: Assessment and strategies for risk reduction. J Clin Oncol 30: 3734-3745. [Google Scholar] [Cross Ref]
- Zhou S, Lu Z, Wu H, Gu CY, Zhang DY, et al. (2017) Synchronous multiple primary gallbladder and gastric malignancies: Report of two cases and review of the literature. Mol Clin Oncol 7: 869-873. [Google Scholar] [Cross Ref]
- Utada M, Ohno Y, Hori M, Soda M. (2014) Incidence of multiple primary cancers and interval between first and second primary cancers. Cancer Sci 105: 890-896. [Google Scholar] [Cross Ref]
- Whitworth J, Hoffman J, Chapman C, Ong KR, Lalloo F, et al. (2015) A clinical and genetic analysis of multiple primary cancer referrals to genetics services. Europ J Human Genet 23: 581-587. [Google Scholar] [Cross Ref]
- Ohno Z, Tamaki H, Ohsuga T, Iwata H, Yasuda N, et al. (2012) Primary lung cancer complicated by malignant lymphoma in two cases of Epstein-Barr virus infection. Case Rep Oncol 5: 367-372. [Google Scholar] [Cross Ref]
- Liu Z, Liu C, Guo W, Li S, Bai O. (2015) Clinical analysis of 152 cases of multiple primary malignant tumors in 15,398 patients with malignant tumors. PLoS One 10: e0125754. [Google Scholar] [Cross Ref]
- Lee DY, Kang K, Jung H, Park YM, Cho JG, et al. (2019) Extranodal involvement of diffuse large B-cell lymphoma in the head and neck: An indicator of good prognosis. Auris Nasus Larynx 46: 114-121. [Google Scholar] [Cross Ref]
- Takano S, Matsushita N, Oishi M, Okamoto S, Teranishi Y, et al. (2015) Site-specific analysis of B-cell non-Hodgkin’s lymphomas of the head and neck: A retrospective 10-year observation. Acta Oto-Laryngologica 135: 1168-1171. [Google Scholar] [Cross Ref]
- Powell S, Tarchand G, Rector T, Klein M. (2013) Synchronous and metachronous malignancies: Analysis of the Minneapolis Veterans Affairs (VA) tumor registry. Cancer Causes Control 24: 1565-1573. [Google Scholar] [Cross Ref]
- Arakawa K, Hata K, Yamamoto Y, Nishikawa T, Tanaka T, et al. (2018) Nine primary malignant neoplasms-involving the esophagus, stomach, colon, rectum, prostate, and external ear canal-without microsatellite instability: A case report. BMC Cancer 18: 1-5. [Google Scholar] [Cross Ref]
- Van Leeuwen FE, Somers R, Taal BG, Van Heerde P, Coster B, et al. (1989) Increased risk of lung cancer, non-Hodgkin's lymphoma, and leukemia following Hodgkin's disease. J Clin Oncol 7: 1046-1058. [Google Scholar] [Cross Ref]
- Travis LB, Curtis RE, Boice Jr JD, Hankey BF, Fraumeni Jr JF (1991) Second cancers following nonâ?Hodgkin's lymphoma. Cancer 67: 2002-2009. [Google Scholar] [Cross Ref]
- Konits PH, Aisner J, Whitacre M, Wiernik PH (1982) Lung cancer as a complication of prolonged survival in patients with lymphoma. Med Pediat Oncol 10: 331-338. [Google Scholar] [Cross Ref]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 