Case Report, Clin Oncol Case Rep Vol: 5 Issue: 4
A Rare Case of AML Presenting as Leukocytoclastic Vasculitis
Medhavi Rajput*, Iulia Kovalenki, and Sudhamshi Toom
Department of Internal Medicine, University of Pittsburgh Medical Center, Harrisburg, Pennsylvania, USA
*Corresponding Author: Medhavi Rajput
Department of Internal Medicine, University of Pittsburgh Medical Center, Harrisburg, Pennsylvania, USA
E-mail: medhavirajput@gmail.com
Received: March 23, 2022; Manuscript No: COCR-22-58143;
Editor Assigned: March 30, 2022; PreQC Id: COCR-22-58143 (PQ);
Reviewed: April 15, 2022; QC No: COCR-22-58143 (Q);
Revised: April 18, 2022; Manuscript No: COCR-22-58143 (R);
Published: April 25, 2022; DOI: 10.4172/cocr.5(4).224
Citation: Rajput M, Kovalenki I, Toom S (2022) A Rare Case of AML Presenting as Leukocytoclastic Vasculitis. Clin Oncol Case Rep 5:4
Abstract
Cutaneous manifestations are commonly observed in the clinical course of Acute Myelogenous Leukemia (AML). In 10% to 15% of cases, skin eruptions arise from leukemic skin infiltration and are known as leukemia cutis. Nonspecific cutaneous lesions caused by non-leukemic skin reactions, such as vasculitis, are also described in the literature. Here we present a rare case of patient who presented to the clinic with recent diagnosis of leukocytoclastic vasculitis and new onset neutropenia after she was treated with antibiotics for her skin condition.
Keywords: Leukemia; Myelogenous; Clinical; Antibiotics; Vasculitis
Case Presentation
A 69-year-old female presented to Hematology clinic for the evaluation of neutropenia associated with painful bilateral lower extremity swelling with skin changes. She was prescribed cephalexin for her lower extremity swelling and rash, her symptoms did not improve with antibiotic regimen. Patient had eventual skin biopsy done, which showed leukocytoclastic vasculitis (Figure 1). She was started on prednisone and it improved her lower extremity rash. However, her rash started to come back when she was on the steroid taper. And the CBC obtained after prednisone treatment showed neutropenia (with neutrophil % 39.6 and absolute neutrophils 0.9). Initially her neutropenia which was new was attributed likely a side effect from antibiotic, her neutropenia persisted and started worsening prompting a bone marrow biopsy. Her neutropenia persisted despite stopping the antibiotic. She also had new symptoms such as noticing discomfort, intermittent needles/pins sensation and mild swelling on her legs. Repeat CBC showing cytopenias on other cell lines including platelet and hemoglobin (85 and 8.3 respectively). Eventually, patient got bone marrow aspiration and biopsy done that showed acute leukemia M4 subtype with 23% CD 34 positive myeloblasts.
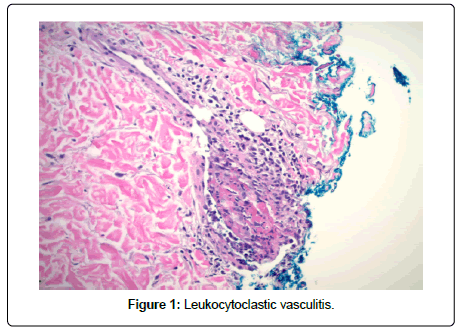
Figure 1: Leukocytoclastic vasculitis.
Discussion
Autoimmune reactions are widely described as a part of clinical presentation of Myelodysplastic Syndromes (MDS) with an incidence from 10% to 30% of cases [1-3]. This association may occur either secondary to immunosuppressive treatments or due to autoimmune nature of MDS itself related to altered T-cell hemostasis and oligoclonal activation against stem cells [4]. Importantly, autoimmune diseases including vasculitis occurrence in patients with MDS appears to be a predictor of transformation to AML [5]. Herein, there must be a common pathophysiologic component involved into development of AML and accompanying autoimmune reactions.
Leukocytoclastic vasculitis is the most common vasculitis in patients with MDS and constitutes 8% of cutaneous lesions in patients with AML [6]. Still, it appears to be a rare condition with only 8 cases of leukocytoclastic vasculitis described in the literature [6-8]. Most commonly, it occurs in the setting of adverse drug reaction. However, our case highlights the possibility of leukocytoclastic vasculitis occurrence in treatment-naïve patients. Moreover, this case appears to be the second case of leukocytoclastic vasculitis described in the literature as a part of the AML clinical manifestation [9].
Conclusion
We propose a possibility of common pathophysiologic mechanism involved in MDS transformation to AML. Herein, vasculitis occurring in a patient with previously known MDS or in a patient with no significant past medical history may be a sign of AML new-onset. Awareness of this unusual presentation can contribute into early diagnosis and improve this patient population outcomes.
References
- Cibull TL, Thomas AB, O'Malley DP, Billings SD (2008) Myeloid leukemia cutis: A histologic and immunohistochemical review. J Cutan Pathol 35: 180-185.
Google Scholar Cross Ref - Berthier S, Magy N, Gil H (2001) Myelodysplasies et maladies systémiques: une association non fortuite. Rev Med Intern 22: 428-432.
Google Scholar Cross Ref - Enright H, Jacob HS, Vercellotti G (1995) Paraneoplastic autoimmune phenomena in patients with myelodysplastic syndromes: Response to immunosuppressive therapy. Br J Haematol 91: 403-408.
Google Scholar Cross Ref - Sloand EM, Mainwaring L, Fuhrer M (2005) Preferential suppression of trisomy 8 compared with normal hematopoietic cell growth by autologous lymphocytes in patients with trisomy 8 myelodysplastic syndrome. Blood 106: 841-851.
Google Scholar Cross Ref - Komrokji RS, Kulasekararaj A, Al Ali NH, Kordasti S, Bart-Smith E, et al. (2016) Autoimmune diseases and myelodysplastic syndromes. Am J Hematol 91: E280-E283.
Google Scholar Cross Ref - Desch JK, Smoller BR (1993) The spectrum of cutaneous disease in leukemias. J Cutan Pathol 20: 407-410.
Google Scholar Cross Ref - Azari-Yaam A, Safavi M, Ghanadan A (2020) Aleukemia cutis: Clinicopathological and molecular investigation of two cases. J Cutan Pathol 47: 747-754.
Google Scholar Cross Ref - Engelhardt M, Rump JA, Hellerich U, Mertelsmann R, Lindemann A (1995) Leukocytoclastic vasculitis and long-term remission in a patient with secondary AML and post-remission treatment with low-dose interleukin-2. Ann Hematol 70: 227-230.
Google Scholar Cross Ref - Neftel K, Hauser S, Müller M, Wälti M, Murphy M, et al. (1986) Cephalosporin-induced neutropenia. Brit J Haematol 62: 394-397.
Google Scholar Cross Ref
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 