Case Report, Clin Oncol Case Rep Vol: 1 Issue: 1
A Very Rare Case Presentation of Chronic Lymphocytic Leukemia Occurring during the Course of Chronic Myeloid Leukemia
Patkar Salil, Panchal Harsha*, Asha Anand, Patel Apurva and Parikh Sonia
Medical Oncology Department, Gujarat Cancer Research Institute, Ahmedabad, India
*Corresponding Author : Dr. Harsha P Panchal
Professor and Head of Medical Oncology, Department of Medical Oncology, Gujarat Cancer and Research Institute, Ahmedabad, Gujarat, India
E-mail: drharshapanchal@gmail.com
Received: December 13, 2017 Accepted: March 08, 2018 Published: March 15, 2018
Citation: Salil P, Harsha P, Anand A, Apurva P, Sonia P (2018) A Very Rare Case Presentation of Chronic Lymphocytic Leukemia Occurring during the Course of Chronic Myeloid Leukemia. Clin Oncol Case Rep 1:1.
Abstract
The occurrence of Chronic Myeloid Leukemia (CML) And Chronic Lymphocytic Leukemia (CLL) in the same patient is a rare event. In at least some of the cases the etiology appears to be either chemotherapy or radiation therapy induced molecular damage to the hematopoietic stem cells. However, a report of a few cases where coexistence or subsequent development of the two diseases was found in previously untreated patients also raises the possibility of other causes. We report the case of one patient who was diagnosed with CLL 66 months after CML diagnosis. This article is to the best of our knowledge only the sixth case report of its nature in published literature and the first from India.
Keywords: Leukemia; Hematopoietic stem cells; Myeloproliferative disorder
Introduction
Chronic lymphocytic leukemia (CLL) is the most common leukemia of adults characterized by a progressive accumulation of functionally incompetent lymphocytes which are usually monoclonal in origin. Chronic myeloid leukemia (CML), the most common myeloproliferative disorder, has a characteristic t (9; 22) (q34; q11) cytogenetic abnormality that involves fusion of the BCR gene on chromosome 22 with the ABL gene on chromosome 9. BCR/ABL fusion results in constitutive activation of tyrosine kinase, which leads to uncontrolled proliferation of myeloid cells.
Occurrence of chronic myeloid and chronic lymphocytic leukemia in the same patient is a very rare phenomenon. Most cases reported had CLL and CML simultaneously [1-6] or developed CML several years after treatment of CLL with chemo- or radio-therapy [7-14]. Until now, only five patients have been reported in whom CLL developed after the diagnosis of CML [15-18]. We report an additional patient who developed CLL several years after the diagnosis of CML. Our paper is the first Indian report of CLL occurrence after CML diagnosis and as far as we know the sixth case report of such association in published literature.
Case Report
A 57-year-old male patient from a rural area, farmer by occupation came to our hospital with chief complaints of abdominal pain, fatigue and generalized weakness.
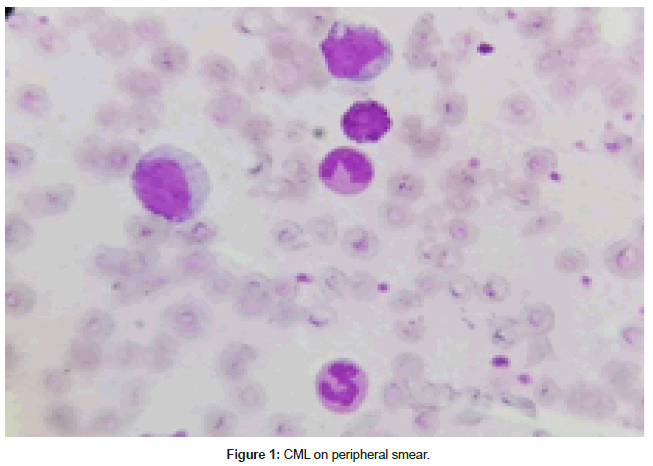
His CBC was Hb 9.2 g/dl, WBC-107 × 109/L; Differential count was Blast- 03, Promyelocytes-02, Myelocytes- 28, Metamyelocytes-16, Band + Polymorphs -32, Basophils-04, Eosinophils-03 .There was no evidence of lymphocytosis. Short term cultured bone marrow sample was used for conventional cytogenetics and fluorescent in situ hybridization (FISH). The FISH probe 9_22 was labeled with Orange signal for the ABL gene on chromosome 9q34 and Green signal for the BCR gene on chromosome 22q11. The sample was positive was BCR ABL fusion by FISH. We have used a real time PCR assay that detects both the E13A2 and E14A2 transcripts for the purpose of monitoring disease post therapy. It is not possible to distinguish between the two on real time PCR. Transcript analysis was not done at baseline. He was started on 400 mg/day of Imatinib. The patient showed a complete hematological response at 4 weeks and had achieved complete cytogenetic and major molecular response (IS ratio< 0.1% by quantitative real-time quantitative polymerase chain reaction) at one year. However there was loss of hematological response at 3 years and the dose of Imatinib was increased accordingly. Imatinib Resistance Mutation Analysis (IRMA test) was advised by us, however, was not done by our patient due to economic constraints and hence, second line Tyrosine Kinase Inhibitor (TKI) was not an option.
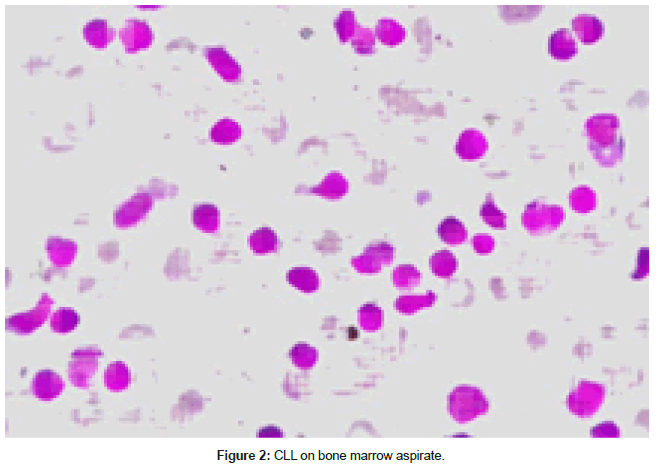
Five years after the start of treatment, he began to show a progressive increase in the lymphocyte count and lymphadenopathy. His WBC count was 30.7 × 109/L and platelets- 400 × 109/L. The bone marrow aspirate was hyper cellular. It showed marked proliferation of small lymphoid cells (81%). Myeloid and erythroid precursors were suppressed. Megakaryocytes were seen. On peripheral smear, lymphocytic leukocytosis (68% Lymphocytes on differential count)) was seen. Absolute lymphocyte count was 10,800/mm3.
Immunophenotypic analysis by flowcytometry was done on FACS Canto II confirmed the diagnosis of CLL:90% lymphocytes were gated with CD19 APCH7 vs side scatter : CD23+, CD5+, CD10 -, CD3-, CD45+,CD56-,FMC7 -, sIgM weak + and CD79b -. Expression of CD5/CD23 was 37%. FISH for CLL cytogenetics was not done. The patient showed bilateral cervical, axillary and inguinal lymph node enlargement of 3.5 cm or less. The patient is at present under close observation for CLL with no active intervention due to an indolent course so far. At last follow up in October 2017 the patient was on Imatinib for CML and was on observation for CLL with a count of 8.2 g/dl Hb, WBC count of 8.2 × 109/L with 40% lymphocytes and platelet count of 142 × 109/L. His RT-PCR BCR-ABL ratio was 5.10% in June 2017 (Figures 1 and 2).
Discussion
Patients with CLL are predisposed to the development of a second malignancy due to impaired immune system or chemotherapy [19]. The second malignancy in the majority of cases is non-hematologic and occurs several years after the diagnosis of CLL [20]. Our patient was confirmed with CLL 48 months after the initial diagnosis of CML. (Table 1).
| Articles | Age [years] | Gender | Interval [months] | Treatment |
|---|---|---|---|---|
| Salim [17] | 54 | F | 36 | Hydroxyurea, IFN-α, Imatinib |
| Gargallo [15] | 88 | F | 20 | Chlorambucil, Hydroxyurea |
| Bhagavathi [16] | 71 | M | 74 | Imatinib |
| Manuela [15] | 54 | 60 | Hydroxyurea,Imatinib, Rituxima based chemotherapy | |
| Chang [21] | 57 | M | 6 | Hydroxyurea, Imatinib |
Table 1: Published articles of patients with CLL after CML.
Bagvathi et al reported a case of a 71 year old male diagnosed with CML and started on Imatinib for the same. The patient’s subsequent BCR/ABL analyses were negative. Seven years later a bone marrow examination with immunophenotyping by flowcytometry revealed CLL. Cytogenetic analysis demonstrated 46XY, Inv (9) (p12q13) and negative for t (9; 22). As reported in 2008, their patient was in molecular remission for CML and not being treated for CLL [16].
There was loss of major molecular response to Imatinib 400 mg dose in our patient, following which the dose was escalated to 600 mg.
Ana Manuela Crisan et al reported a 54 yr old patient who underwent nephrectomy for a renal tumor (tubular adenocarcinoma). Six months later an abnormal blood count revealed CML confirmed by FISH. At 60 months while on Imatinib the patient was diagnosed with CLL. The patient continued to maintain molecular remission for CML as defined by European leukemia net (ELN). Two years later the patient showed progression for the CLL clone. Imatinib was stopped and the patient was started on Rituximab based chemotherapy. The patient died due to neutropenia related complications [18].
Our patient has no history of any prior cancer diagnosis or treatment and continues to be treated for CML with Imatinib, but is not at present being treated for an indolent CLL.
Chang et al. reported CLL diagnosis six months after CML, the patient was treated with hydroxyurea for a brief period until counts normalized and then started on Imatinib. The authors used fluorescence activated sorting method of purified CLL cells (CD5+/ CD19+) and analyzed them by interphase FISH with two colors to detect translocations BCR/ABL1. The conclusion was that there were two different clone proliferations: a population of B-cells clone, which did not, expressed the BCR/ABL1 fusion gene and another CML clone which expressed BCR/ABL1 fusion gene [22].
In our patient the CLL clone was demonstrated by flow cytometry, however no further investigations were made to demonstrate if the two diseases had different progenitor stem cells.Gargallo et al. reported B-cell CLL diagnosis 20 months after CML diagnosis. The patient received Hydroxyurea and 20 months later blood count revealed leukocytosis and absolute lymphocytosis. The authors demonstrated by cytogenetic, FISH and molecular tests that the two diseases have emerged from different clones [15]. Salim et al. reported CLL diagnosis a few years after CML diagnosis [17].
One hypothesis by Peters et al suggests that CML may create a microenvironment conducive for the development of CLL [23]. Malignant transformed cells in CML secrete a variety of cytokines such as interleukin- 3 (IL3). These cytokines increase the production of B lymphoid cells from human CD 34(+) CD 38(-) immature cells [22]. Sufficient data exists to exclude the possibility of a common hematopoietic stem cell origin for the two entities. Crisan et al considered the role of TKI and development of secondary malignancy [18]. In a study at MD Anderson of over 1400 CML pts on TKI the incidence of secondary malignancy was 4.6 percent with skin being the most common at 31%. CLL occurred at rate of 3 %. Currently however there is no evidence to suggest that TKIs increase the risk for a second cancer.
Conclusion
We report a case of a 57 year male patient presenting with CLL four years after the diagnosis of CML .To our knowledge this is the first case reported from India. So far only six cases of its kind have been reported in literature, there appears to be no difference in the disease biology when CML precedes CLL, however, rarity of this event, and hence, paucity of data makes establishing a definite hypothesis difficult.
References
- Manoharan A, Catovsky D, Clein P, Traub NE, Costello C, et al. (1981) Simultaneous or spontaneous occurrence of lympho and myeloproliferative disorders: A report of four cases. Br J Haematol 48: 11-16.
- Viplo JA, Klemi P, Lassila O, Andde la Chapelle A (1980) Concomitant presentation of two chronic leukemias: Evidence for Independent clonal evolution. Am J Haematol 8: 205-221 I.
- Browett P.J, Pattinson J, Pinkney J, Hoffbrand AV, Norton JD (1988) Gene probe analysis demonstrates independent clonal evolution of coexistent chronic myeloid and chronic lymphocytic leukemia. Eur J Haematol 40: 181-184.
- Schreiber ZA, Axelrod MR, Abebe LS (1984) Coexistence of chronic myelogenous leukemia and chronic lymphocytic leukemia. Cancer 54: 697-701.
- Leoni F, Ferrini PR, Castoldi GL, Pata M, del Prete GF, et al. (1987) Simultaneous occurrence of chronic granulocytic leukemia and chronic lymphoid leukemia. Haematologica 72: 253-256.
- Esteve J, Cervantes F, Rives S, Rozman M, Zarco MA, et al. (1997) Simultaneous occurrence of B-cell chronic lymphocytic leukemia and chronic myeloid leukemia withfurther evolution to lymphoid blast crisis. Hematologica 82:596-599.
- Teichman, JV, Seiber G, Ludwig WD, Karow J, Ruehl H (1986) chronic myelocytic leukemia as second neoplasia in thecourse of chronic lymphocytic leukemia: Case report and review of literature. Leuk Res 10: 361-368.
- Khojasteh A, Perry MC, Taylor HM (1981) chronic myelocyticleukemia developing as a second cancer in a patient with chronic lymphocytic leukemia. CA-Cancer J Clinicians 31: 172-176
- Martin PJ, Najfeld V, Hansen JA, Penfold GK, Jacobson RJ, et al. (1981) Involvement of the B lymphoid system in chronic myelogenousleukemia. Nature 287: 49.
- Whang-Peng J, Gralnik HR, Johnson RE, Lee EC, Lear A (1974) Chronic granulocytic leukemia (CGL) during the course of chronic lymphocytic leukemia (CLL): Correlation of blood, marrow and spleen morphology and cytogenetics. Blood 43: 333.
- Faguet GB, Little T, Agee JF, Garver FA (1983) Chronic lymphocytic leukemia evolving into chronic myelocytic leukemia. Cancer 52: 1647-1652.
- Nanjangud GJ, Saikia TK, Chopra H, Kadam PR, Advani SH (1996) Development of PH positive chronic myeloid leukemia in a patient with chronic lymphocytic leukemia treated with total body irradiation: a rare association. Leuk Lymphoma 22: 355-359.
- Mossafa H, Fourcade C, Pulic M, Jary L, Cheze S, et al. (2001) Chronic lymphocytic leukemia associated with myelodysplastic syndrome and/or chronic myeloid leukemia: evidence for independent clonal chromosomal evolution. Leuk Lymphoma 41: 337-341.
- Ramanarayanan J, Dunford LM, Baer MR, Sait SN, Lawrence W, et al. (2006) Chronic myeloid leukemia after treatment oflymphoid malignancies: response to imatinib mesylate and favorable outcomes in three patients. Leuk Res 30: 701-705.
- Gargallo P, Cacchione R, Chena C, Dupont J, Garay G, et al. (2005) Chronic lymphocytic leukemia developing in a patient with chronic myeloid leukemia: evidence of distinct lineage-associated genomic events. Cancer GenetCytogenet 161: 74-77.
- Bhagavathi S, Borromeo V, Desai H, Crisan D (2008) Case report and literature review: a rare patient with chronic myeloid leukemia and chronic lymphocytic leukemia. Ann Clin Lab Sci 38: 405-409
- Salim R, Wang L, Lin K, Clark RE (2002) Chronic lymphocytic leukemia developing in the course of chronic myeloid leukemia. Leuk Lymphoma 43: 2225-2227.
- Crişan AM1, BădeliŢă SN, Jardan C (2015) The occurrence of chronic lymphocytic leukemia after chronic phase of chronic myeloid leukemia: case report and literature review.Rom J Morphol Embryol 56: 1145-1151
- Bartik MM, Welker D, Kay NE (1998) Impairments in immune function in B cell chronic lymphocytic leukemia.Semin Oncol 25: 27-33.
- Hisada M, Biggar RJ, Greene MH, Fraumeni JF, Travis LB (2001) Solid tumors after chronic lymphocytic leukemia.Blood 98: 1979-1981.
- Chang H, Sutherland R, Nayar R, Li D, Kamel-Reid S, Mile MA, et al. (2004) Chronic lymphocytic leukemia in the course of chronic myelocytic leukemia: evidence of independent clonal origin as shown by interphase fluorescence in sit hybridization and fluorescence-activated cell sorting. Cancer Genet Cytogenet 152: 146-148.
- Peters DG, Klucher KM, Perlingeiro RC, Dessain SK, Koh EY, et al. (2001) Autocrine and paracrine effects of an ES-derived, BCR/ABL transformed hematopoietic cell line that induces leukemia in mice Oncogene 20: 2636-2646.
- Crooks GM, Hao QL, Peterson D, Barsky LW, Bockstoce D (2000) IL-3 increases production of B lymphoid progenitor’s from human CD34+CD38- cells. J Immunol 165: 2382-2389.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi