Research Article, J Fashion Technol Textile Eng Vol: 6 Issue: 1
An Insulating Palmar / Plantar Muff as a Passive Thermotherapeutic Intervention for Sleep Disturbance Caused by Primary Vascular Dysregulation
1Sleep Disorders Center, St. Peter's Health Partners, Albany, New York, USA
2Department of Biomedical Engineering, Cornell University, Ithaca, New York, USA
*Corresponding Author : Erik A. Zavrel, Ph.D
Department of Biomedical Engineering, Cornell University, 101 Weill Hall, 237 Tower Rd, Ithaca, New York 14853, USA
Tel: +646-760-9287
E-mail: eaz29@cornell.edu
Received: March 13, 2018 Accepted: April 10, 2018 Published: April 15, 2018
Citation: Glovinsky PB, Zavrel EA (2018) An Insulating Palmar / Plantar Muff as a Passive Thermo-therapeutic Intervention for Sleep Disturbance Caused by Primary Vascular Dysregulation. J Fashion Technol Textile Eng 6:1. doi:10.4172/2329-9568.1000164
Abstract
Our innovation is a specially constructed insulating muff, accessible through digit flexion, designed to produce distal skin temperature changes for the treatment of sleep disturbance caused by thermal dysregulation, a problem most often seen in women. We have designed a simple and comfortable muff that promotes either heat retention or heat dissipation depending upon digit flexion or digit extension, respectively. We have conducted small-scale piloting of our insulating muff and obtained encouraging preliminary data of its effect on distal skin warming. This innovation will allow sleepers to auto-regulate distal skin temperature through subtle movements
during sleep, preserving overall sleep architecture and improving sleep quality.
Keywords: Sleep; Sleepwear; Thermal insulation; Muff; Female health; Women’s health; Primary vascular dysregulation; Vasospastic syndrome; Flammer syndrome; Hands; Feet
Introduction
Thermoregulation plays a key role in promoting and maintaining sleep. Temperature dysregulation and sleep disturbance (difficulty initiating or maintaining sleep) commonly occur in two distinct populations of otherwise healthy women: (1) peri-or post-menopausal women with vasomotor symptoms (such as hot flashes and night sweats) and (2) those with primary vascular dysregulation (PVD), a condition characterized by abnormal vasoconstriction. Both are characterized by acute reactions to ambient temperature stressors. PVD (also known as vasospastic syndrome and now known as Flammer syndrome) is characterized by a propensity to react to cooler ambient temperatures with dysregulation in vascular tone. While vascular dysregulation can occur elsewhere in the body, it most often takes the form of peripheral vasoconstriction, leading to the chronic coldness of the extremities that is the hallmark of the disorder [1-3]. PVD most typically occurs in young to middle-aged women with a low body mass index (BMI) [4]. A random population survey of 2800 inhabitants of Basel, Switzerland, found that 31% of women but only 7% of men complained of cold hands and feet [5]. Those with PVD are characterized by cold hands and cold feet as well as by a significantly delayed sleep onset latency (SOL) and greater difficulty falling back to sleep after nocturnal arousal [6-8]. Thus, some presentations of insomnia may be secondary to distal vasodilation failure.
Existing Treatment Options and Limitations
Research into thermoregulation and sleep has revealed that warm hands and feet are associated with increased sleepiness and rapid sleep onset and that warming of hands and feet through the wearing of certain articles, e.g., mittens, gloves (https://clinicaltrials.gov/ct2/show/NCT02341287), socks, or full-body water-perfused thermosuits can reduce SOL and hasten sleep onset [9-17]. However, few people can remain comfortable while wearing insulating mittens, gloves, or socks throughout the entire night. The same distal skin warming that triggers sleepiness at the beginning of the night may interfere with sleep later on [18-21]. Insulating articles may result in uncomfortable temperature swings that disrupt sleep: wearing mittens, gloves, and socks may cause distal skin temperature to spike, causing the person to wake to remove the articles to obtain temporary relief, only to start feeling cold again, necessitating retrieval and re-donning of the articles, in a vicious sleep-disruptive cycle.
Innovation
In addition to position changes, rearrangements of the blanket or pillow, and other gross body movements [22], more subtle motions are also seen in sleep. These include involuntary, myoclonic movements (sudden twitches or jerks) that can be a source of sleep disruption, but also benign finger and toe movements, of the type commonly observed in sleeping infants presumably searching for contact comfort with the mother or her surrogate in a fleece or soft blanket [23-26]. Movements of the latter type can be used to increase or reduce contact with an insulating muff and thereby auto-regulate distal skin temperature, flexing digits around the insulating muff to increase contact, minimize heat loss, and increase distal skin temperature and extending digits away from the insulating muff to reduce contact, maximize heat loss, and decrease distal skin temperature. Unlike insulating gloves and socks, which can only heat and can lead to uncomfortable distal skin temperature spikes throughout the night, our insulating palmar and plantar muffs can produce bi-directional changes in distal skin temperature in response to internal cues of feeling too warm or too cold, thereby improving subjective comfort and sleep.
Prototype Description
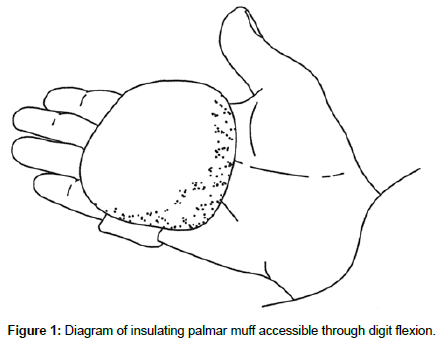
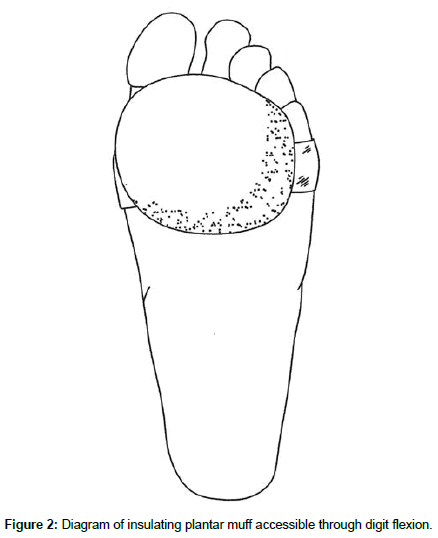
The insulating muffs are covered with a soft material such as shearling and fitted with a comfortable elastic band that allows them to be secured to the palmar aspect of the hand (Figure 1) or the plantar aspect of the foot (Figure 2) behind the phalanges. This arrangement allows the digits to access the insulating material at will with a comfortable flexion of the fingers or toes (Figures 3 and 4). Far from being simply a wad of insulating fabric, the muff is designed to allow the digits to curl around and conform to its contours (similar to an ergonomic computer mouse). Furthermore, the insulating efficiency of the device is continuously adjustable through the degree of digit flexion and hence the amount of contact with the muff, in contrast to gloves and socks, which function in a binary (on/off) manner. A smaller, more targeted degree of insulation present relative to the complete coverage provided by gloves and socks has the benefit of leaving most of the extremities uncovered, preventing overheating.
Materials and Methods
In our pilot tests, a volunteer (a healthy adult female) wore the insulating palmar muff on her left hand (her right hand with no muff served as a control) while awake and lying supine in a standard bed underneath a sheet and thin blanket at standard room temperature (68-70°F). The subject was instructed to flex the fingers of her left hand to grasp the muff for the first 15 minutes while making a similar motion with her right hand (flexing her fingers against her palm) and then naturally extend her fingers (on both hands) for the next 15 minutes. This was done twice, with trials separated by approximately two hours. The subject refrained from eating, drinking, and strenuous activity for at least one hour prior to the beginning of the study as ingestion of food or fluids can influence heat production and affect core and skin temperature, as can physical exertion [12,27].
Skin temperature at the thenar region of the left and right palms was simultaneously monitored using synchronized iButton temperature sensors (Maxim Integrated, San Jose, CA). Placement of DS1921H High-Resolution Thermochron iButtons (iButtonLink, Whitewater, WI) was mirrored bilaterally, i.e., left and right thenar area (palmar region). iButtons were affixed to the skin using thermally conductive double-sided adhesive pads die-cut to match the diameter of iButtons (DS9096P iButton Adhesive Pad, 3M, Maplewood, MN). The bottom sides of the iButtons were applied to the skin because the slightly larger area of the flat (non-engraved) side gave a better attachment when taped onto the skin. A small piece of adhesive dressing retention tape (Hypafix #4209, Amazon, Seattle, WA) was placed over each iButton to keep them from pulling loose during position changes. The data sample rate of the iButtons was set to one measurement per minute. After acquisition, iButton data was transferred to a personal computer using a USB iButton Probe Cable Reader (DS1402, Embedded Data Systems, Lawrenceburg, KY) and a USB to 1-Wire / iButton Adapter (DS9490R, Embedded Data Systems, Lawrenceburg, KY), imported using Thermodata Viewer 3.2.6 software (Thermodata Corporation, Milwaukee, WI), and plotted using a custom iButton data visualization application we developed.
Data
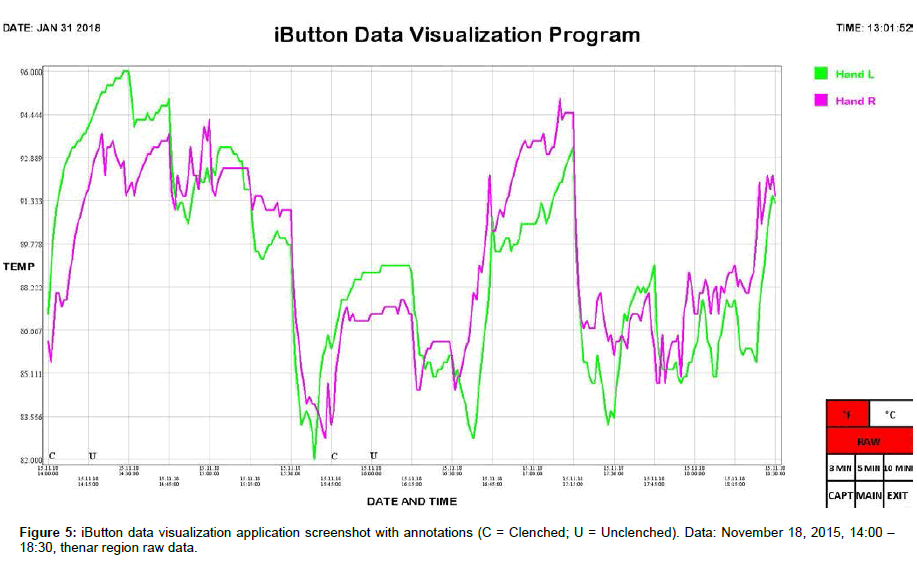
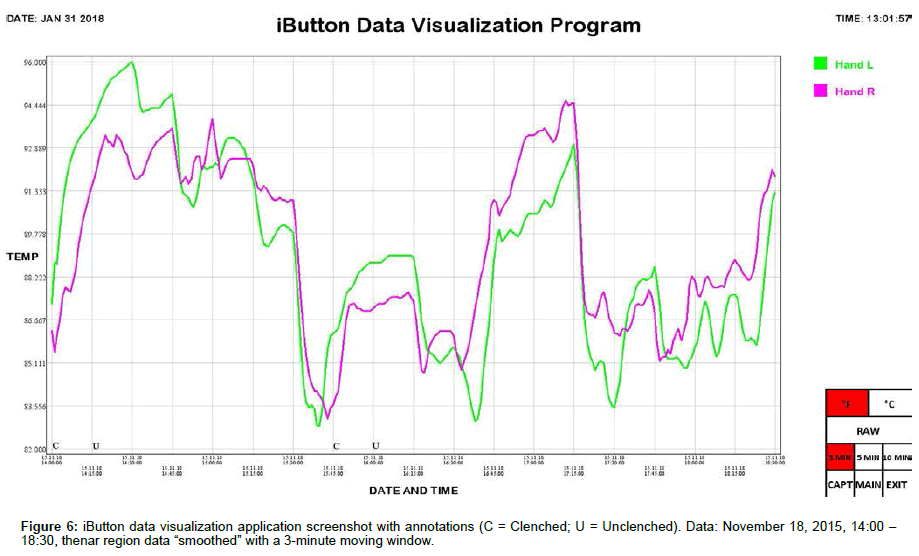
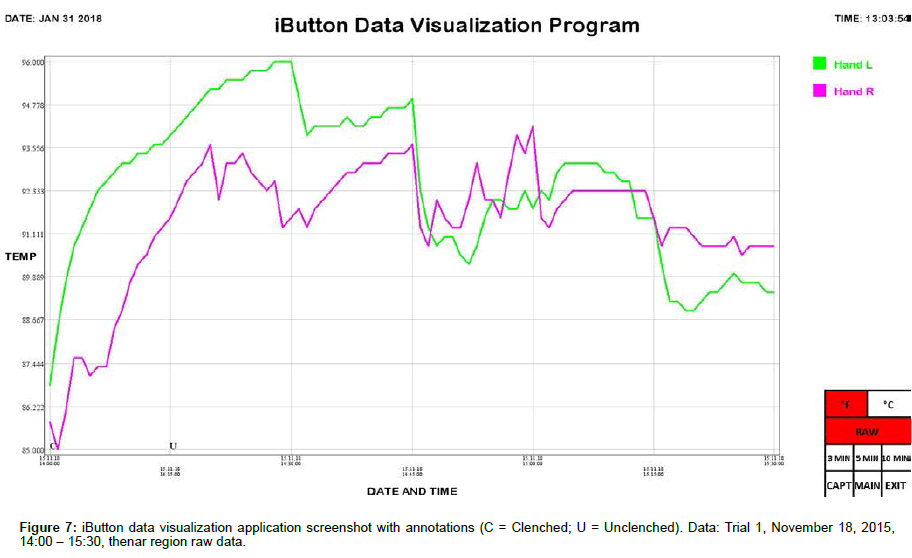
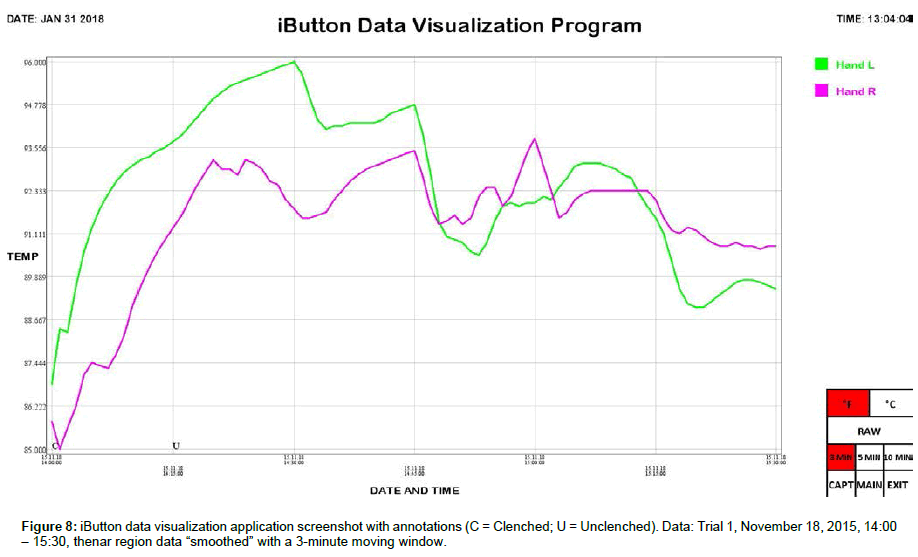
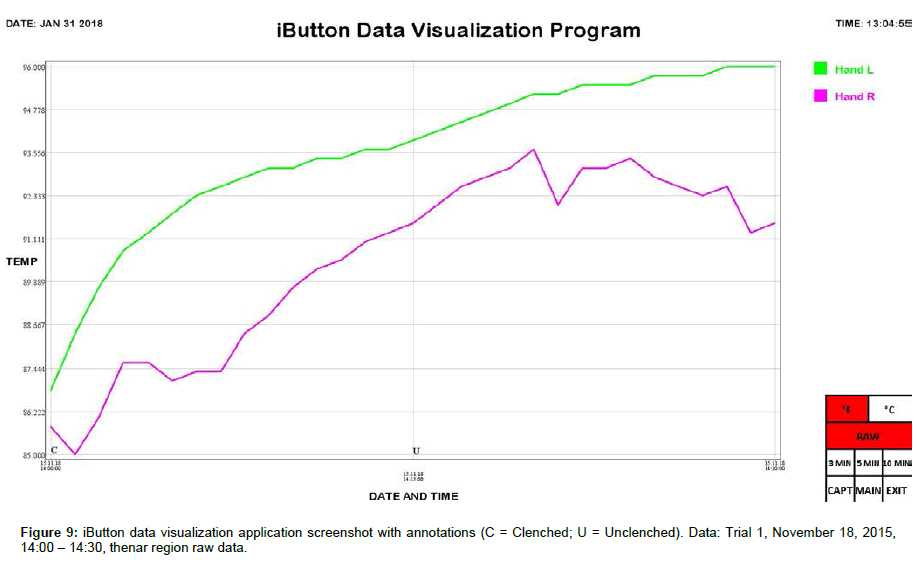
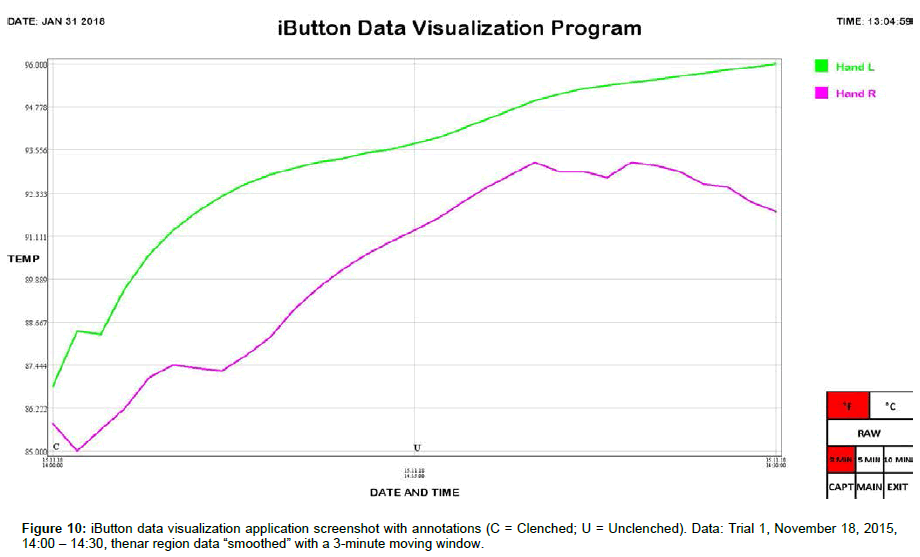
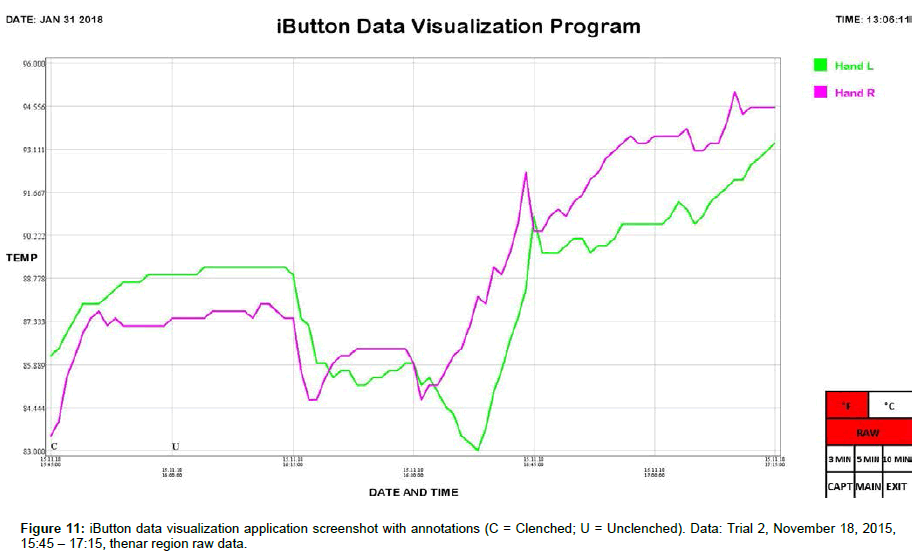
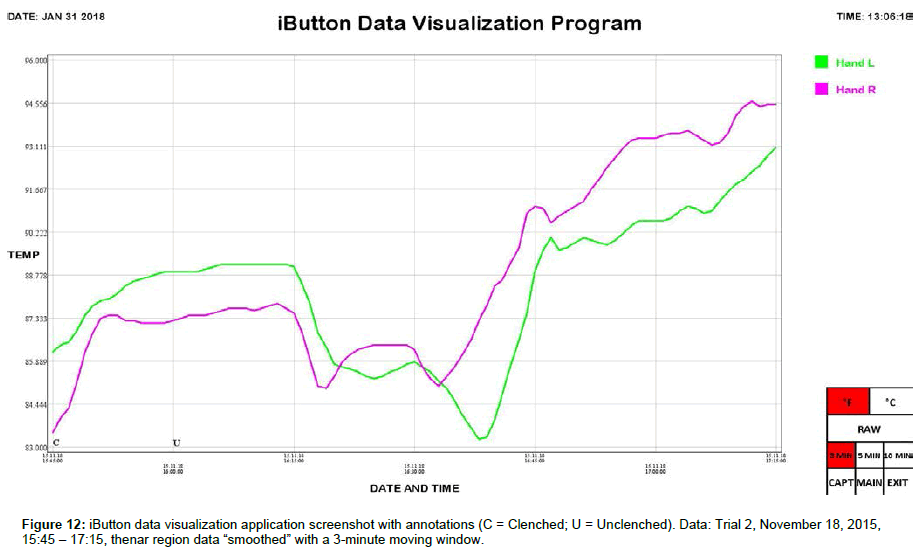
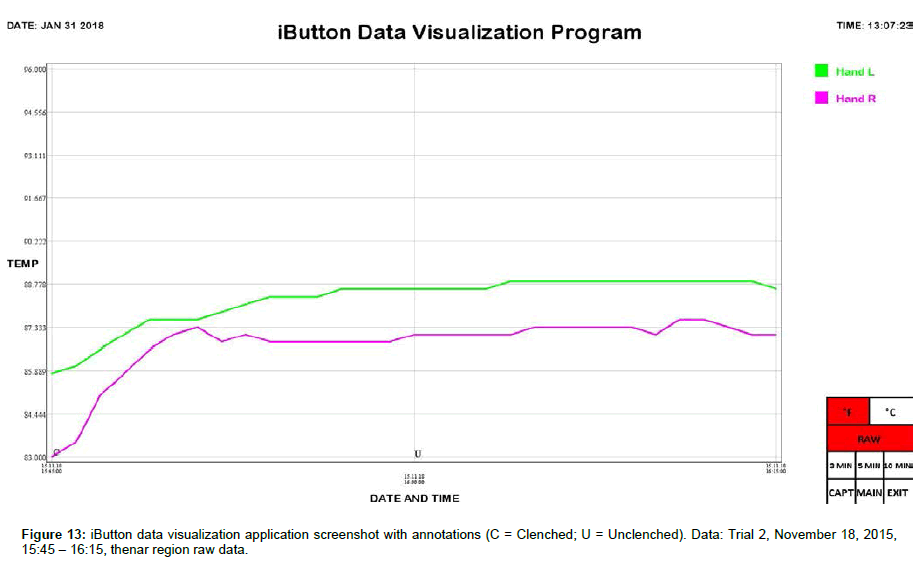
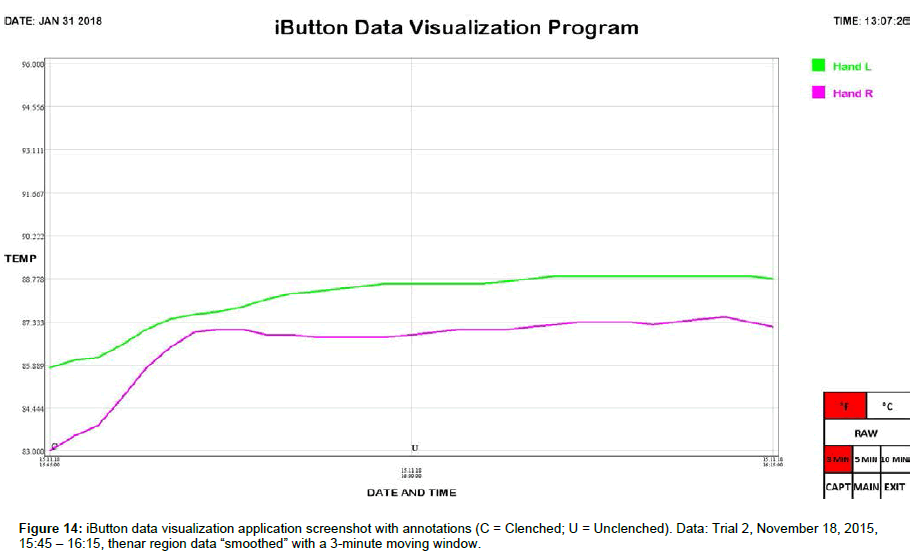
We include here data (Tables 1 and 2) and plots (Figures 5-14) from our pilot study trials comparing skin temperature from the thenar region of the left and right hand (insulating muff on the subject’s left hand and no muff on the subject’s right hand).
| Mean Left Temperature (°F) | Mean Right Temperature (°F) | Mean Lateral Temperature Difference (°F) (Left-Right) | |
|---|---|---|---|
| Trial 1: | |||
| Palmar Muff on and Hands Clenched (N=15) | 91.610 ± 0.456 | 88.580 ± 0.435 | 3.030 ± 0.243 |
| Palmar Muff on and Hands Unclenched (N=15) | 94.550 ± 0.146 | 92.315 ± 0.146 | 2.235 ± 0.187 |
| Palmar Muff Off (N=60) | 91.858 ± 0.212 | 91.786 ± 0.103 | 0.071 ± 0.166 |
| Mean (N=90) | 92.265 ± 0.194 | 91.340 ± 0.166 | 0.925 ± 0.178 |
| Trial 2: | |||
| Palmar Muff on and Hands Clenched (N=15) | 87.875 ± 0.210 | 86.585 ± 0.303 | 1.290 ± 0.153 |
| Palmar Muff on and Hands Unclenched (N=15) | 88.865 ± 0.027 | 87.500 ± 0.042 | 1.365 ± 0.034 |
| Palmar Muff Off (N=60) | 88.081 ± 0.343 | 89.604 ± 0.408 | -1.522 ± 0.183 |
| Mean (N=90) | 88.178 ± 0.233 | 88.750 ± 0.305 | -0.572 ± 0.189 |
| Average | |||
| Palmar Muff on and Hands Clenched (N=30) | 89.742 ± 0.426 | 87.582 ± 0.319 | 2.160 ± 0.215 |
| Palmar Muff on and Hands Unclenched (N=30) | 91.708 ± 0.533 | 89.908 ± 0.453 | 1.800 ± 0.123 |
| Palmar Muff Off (N=210) | 88.468 ± 0.209 | 89.285 ± 0.194 | -0.818 ± 0.103 |
| Mean (N=270) | 88.969 ± 0.190 | 89.165 ± 0.167 | -0.196 ± 0.111 |
Table 1: Average left palm temperature, average right palm temperature, and average lateral temperature difference (left palm temperature minus right palm temperature) from thenar location (values are mean ± SEM); N = number of sample points.
| Max Δ Thenar Temp (°F) | Max Δ Thenar Temp Rate (°F/min) | |||
|---|---|---|---|---|
| Left | Right | Left | Right | |
| Trial 1: | ||||
| Palmar Muff on and Hands Clenched (N=15) | 5.850 | 4.725 | 1.350 | 0.525 |
| Palmar Muff on and Hands Unclenched (N=30) | 1.800 | 1.800 | 0.225 | 0.450 |
| Trail 2: | ||||
| Palmar Muff on and Hands Clenched (N=15) | 2.475 | 3.825 | 0.394 | 0.900 |
| Palmar Muff on and Hands Unclenched (N=30) | 0.225 | 0.450 | 0.056 | 0.045 |
Table 2: Maximum temperature increases and maximum temperature increase rates from thenar location; N = number of sample points.
Results and Discussion
iButton data was collated and analyzed using SPSS 25 software (IBM, Armonk, NY). Statistical analysis was conducted using Welch’s t-test, which is robust against unequal variances and sample sizes. Several observations can be made from the preliminary data. First, the highest thenar temperature reading (95.225 °F), the greatest mean lateral temperature difference (3.030 ± 0.243 °F), the greatest increase in thenar temperature (5.850 °F), and the greatest rate of thenar temperature increase (1.350 °F/min) were all seen with the palmar muff on and hands clenched (Trial 1). Second, the mere presence of the insulating palmar muff serves to elevate thenar temperature whether or not the hand is being clenched. The hand with the palmar muff was always warmer than the hand without the muff, i.e., the mean lateral temperature difference (left minus right) was always positive (Table 1), regardless of hands being clenched or unclenched (Trial 1: hands clenched palmar muff on vs. palmar muff off: 3.030 ± 0.243 °F vs. 0.071 ± 0.166 °F, p<0.001; hands unclenched palmar muff on vs. palmar muff off: 2.235 ± 0.187 °F vs. 0.071 ± 0.166 °F, p<0.001; Trial 2: hands clenched palmar muff on vs. palmar muff off: 1.290 ± 0.153 °F vs. -1.522 ± 0.183 °F, p<0.001; hands unclenched palmar muff on vs. palmar muff off: 1.365 ± 0.034°F vs. -1.522 ± 0.183 °F, p<0.001). Temperatures tend to equalize bilaterally (lateral temperature difference decreases) when the muff is removed. Third, the act of clenching – whether an insulating muff is present or not – serves to increase thenar temperature (Table 2). Lastly, we believe the values obtained in Trial 1 to be more representative of true muff performance as the subject was wearing control sleepwear made of 100% cotton while the subject was wearing special sleepwear with lateralized thermal properties [28] in Trial 2. Even though the subject was in a supine position during testing of the palmar muff in both trials, we feel the data collected while wearing regular sleepwear to be more compelling. Additionally, the difference between the mean lateral temperature difference for palmar muff on and hands clenched vs the mean lateral temperature difference for palmar muff on and hands unclenched was statistically significant in Trial 1 (3.030 ± 0.243°F vs. 2.235 ± 0.187°F, p=0.015) while it was not statistically significant in Trial 2.
Future Work
We intend to correlate distal skin temperature with finger flexion during sleep to further justify our muff intervention. We will do this by correlating hand temperature data collected by iButtons with finger flexion data gathered using flex sensors, which have found widespread use in gestural interface and virtual reality gloves. Demonstrating a correlation between distal skin temperature and finger flexion during sleep will lend additional credence to our proposed intervention.
References
- Flammer J, Orgül S (1998) Optic nerve blood-flow abnormalities in glaucoma. J Prog Retin Eye Res, 17: 267-289.
- Teuchner B, Orgül S, Ulmer H, Haufschild T, Flammer J (2004) Reduced thirst in patients with a vasospastic syndrome. Acta Ophthalmologica 82: 738-740.
- Flammer J, Konieczka K, Flammer A (2013) The primary vascular dysregulation syndrome: implications for eye diseases. The EPMA Journal 4: 1-33.
- Mozaffarieh M, Gasio P, Schötzau A, Orgül S, Flammer J, et al. (2010) Thermal discomfort with cold extremities in relation to age, gender, and body mass index in a random sample of a Swiss urban population. Population Health Metrics 8: 1-5.
- Kräuchi K, Gasio P, Vollenweider S, Von Arb M, Dubler B, et al. (2008) Cold extremities and difficulties initiating sleep: evidence of co-morbidity from a random sample of a Swiss urban population. J Sleep Res 17: 420-426.
- Kräuchi K, Pache M, Cajochen C, Wirz-Justice A, Dubler B, et al. (2001) Cold feet and prolonged sleep-onset latency in vasospastic syndrome. Lancet 358: 125-126.
- Kräuchi K (2007) The thermophysiological cascade leading to sleep initiation in relation to phase of entrainment. Sleep Med Rev 11: 439-451.
- Von Arb M, Gompper B, Meyer A, Stutz E, Orgül S, et al. (2009) Relationship between gender role, anger expression, thermal discomfort and sleep onset latency in women. BioPsychoSocial Medicine 3: 1-7.
- Kräuchi K, Cajochen C, Werth E, Wirz-Justice A (1999) Warm feet promote the rapid onset of sleep. Nature 401: 36-37.
- Kräuchi K, Cajochen C, Werth E, Wirz-Justice A (2000) Functional link between distal vasodilation and sleep-onset latency? The American Journal of Physiology 278: 741-748.
- Fronczek R, Overeem S, Lammers G, van Dijk J, Van Someren E (2006) Altered skin-temperature regulation in narcolepsy relates to sleep propensity. Sleep 29: 1444-1449.
- Kräuchi K, Cajochen C, Pache M, Flammer J, Wirz-Justice A (2006) Thermoregulatory effects of melatonin in relation to sleepiness. Chronobiology International 23: 475-484.
- Van der Heide A, Werth E, Donjacour C, Reijntjes R, Lammers G, et al. (2016) Core body and skin temperature in type 1 narcolepsy in daily life; effects of sodium oxybate and prediction of sleep attacks. Sleep 39: 1941-1949.
- ClinicalTrails.gov (2018) Temperature Manipulating Gloves for the Treatment of Insomnia.
- Kräuchi K, Knoblauch V, Cajochen C, Renz C, Wirz-Justice A (2004) Kneipp bedsocks shorten sleep latency only when feet are warm.
- Raymann R, Swaab D, Van Someren E (2005) Cutaneous warming promotes sleep onset. American Journal of Physiology 288: 1589-1597.
- Raymann R, Swaab D, Van Someren E (2008) Skin deep: enhanced sleep depth by cutaneous temperature manipulation. Brain 13: 500-513.
- Kräuchi K, Wirz-Justice A (1994) Circadian rhythm of heat production, heart rate, and skin and core temperature under unmasking conditions in men. American Journal of Physiology 267: 819-829.
- Van Someren E (2004) Sleep propensity is modulated by circadian and behavior-induced changes in cutaneous temperature. Journal of Thermal Biology 29: 437-444.
- Lack L, Gradisar M, Van Someren E, Wright H, Lushington K (2008) The relationship between insomnia and body temperatures. Sleep Medicine Reviews 12: 307-317.
- Okamoto-Mizuno K, Mizuno K (2012) Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol 31: 1-9.
- Shen T, Tan S, Wu F (2015) Comparison of sleep quality and thermal comfort for innovative mattress design. Procedia Manufacturing 3: 5874-5880.
- Harlow H, Zimmermann R (1958) The development of affectional responses in infant monkeys, Proceedings of the American Philosophical Society 102: 501-509.
- Harlow H, Zimmermann R (1959) Affectional responses in the infant monkey. Science 130: 421-432.
- Harlow H (1959) Love in infant monkeys. Scientific American 200: 68-74.
- Harlow H (1960) Primary affectional patterns in primates. Am J Orthopsychiatry 30: 676-684.
- Kräuchi K (2007) The human sleep-wake cycle reconsidered from a thermoregulatory point of view. Physiology & Behavior 90: 236-245.
- Glovinsky P, Zavrel E (2018) Sleepwear with Lateralized Thermal Properties for the Treatment of Sleep Disturbance in Women. Int J Cloth Sci Tech.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi