Case Report, Clin Oncol Case Rep Vol: 6 Issue: 1
Biphasic Synovial Sarcoma of the Pyriform Fossa: Case Report
Arsheed Hussain Hakeem1*, Hassaan Javaid 2, Meenakshi Swain3, Novfa Iftikhar4
1Department of Head and Neck Oncology, Apollo cancer Institute, Hyderabad, Telangana, India
2Department of Trauma Surgery, All India Institute of Medical Sciences, New Delhi,India
3Department of Pathology, Apollo Cancer Institute, Hyderabad, Telangana, India
4Department of Internal Medicine, Government Medical College, Srinagar, J&K, India.
*Corresponding Author: Arsheed Hussain Hakeem
Department of Head and Neck Oncology
Room No: 10, Apollo Cancer Institute, Jubilee Hills, Hyderabad, Telangana, India 500096.
E-mail: drahhakim@gmail.com
Received: January 09, 2023; Manuscript No: COCR-23-86256;
Editor Assigned: January 11, 2023; PreQC Id: COCR-23-86256 (PQ);
Reviewed: January 21, 2023; QC No: COCR-23-86256 (Q);
Revised: January 23, 2023; Manuscript No: COCR-23-86256 (R);
Published: January 30, 2023; DOI: 10.4172/cocr.6(1).270
Citation: Hakeem AH, Javaid H, Swain M, Iftikhar N (2023) Biphasic Synovial Sarcoma of the Pyriform Fossa: Case Report. Clin Oncol Case Rep 6:1
Abstract
Synovial sarcomas are rare malignant tumours originating from pluripotent mesenchymal stem cells. These sarcomas are usually seen in the deep soft tissue of the lower and upper extremities, particularly in adolescents. Head and neck is a rare site for these sarcoma and pyriform sinus is more unusual site to occur. We report a biphasic synovial sarcoma of the left pyriform sinus in a 16-year-old male and describe its clinical, pathological and immunohistopathology features. With this background the existing literature is being reviewed. The standard of care is wide surgical excision with adjuvant radiation therapy to increase local control and prolong disease-free survival.
Keywords: Synovial; Sarcoma; Pyriform sinus; Biphasic; TLE1
Introduction
Synovial sarcoma is usually seen near large joints and bursae originating from the primitive pluripotent mesenchymal cells [1]. Therefore, the extremities are the common site of occurrence followed by the head and neck region (5% to 10% of all cases) [2,3]. Most of the cases in the head and neck region originate in the paravertebral connective tissue spaces and present as retropharyngeal and/or parapharyngeal masses [4]. Since the first case report of a hypopharyngeal synovial sarcoma by Jernstorm, there have been independent case reports [5]. Pathologically synovial sarcoma has two main components, spindle cells (fibrous) and epithelial cells. If spindle cells are predominant on histopathology, it is categorised as monophasic synovial sarcoma. Biphasic subtype is composed of both spindle and epithelial components and a poorly differentiated synovial sarcoma has also been reported [3,6]. Due to the rare nature of this neoplasm, their diagnosis and therapy is a challenge. No male preponderance has been reported in synovial sarcoma of the head and neck, contrary to that of extremities, where male to female ratio is 1.2:1.3. Very less number of cases have been reported in the subsites like pyriform fossa [4]. We present a case of biphasic synovial sarcoma of the left lateral wall of the pyriform and discuss the surgical approach, pathology with an update on management.
Case Report
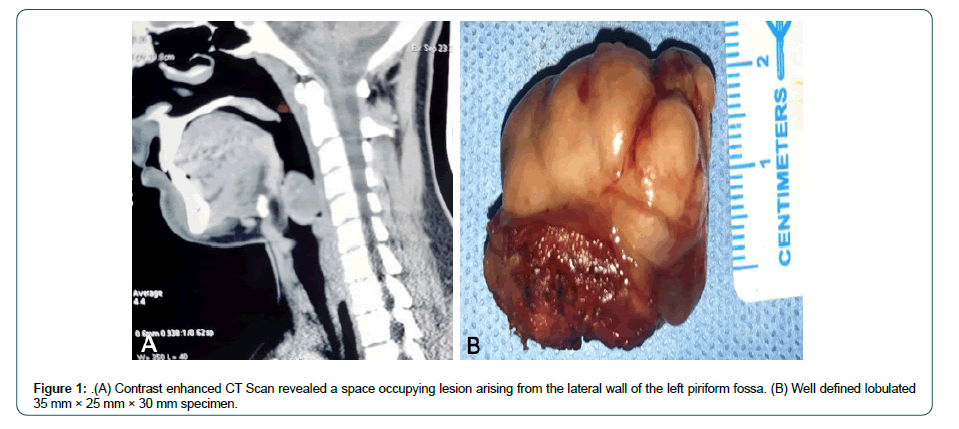
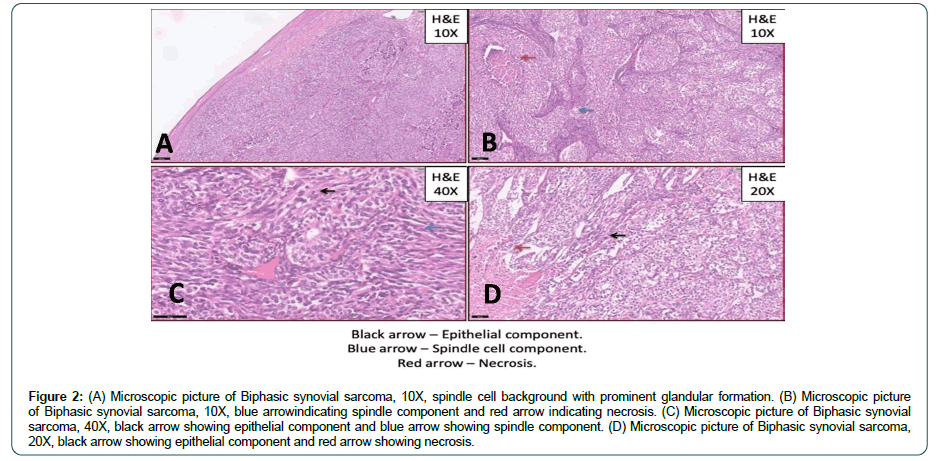
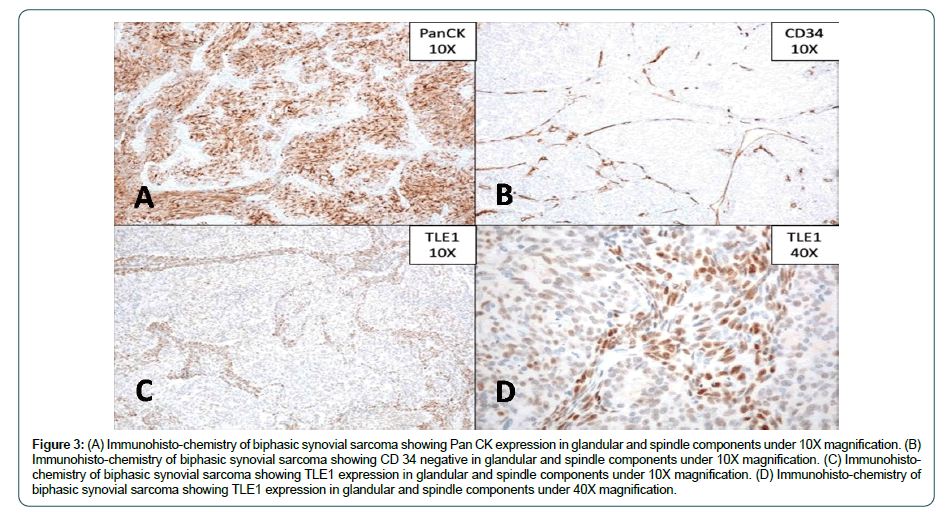
A 16-year-old male presented to our head and neck services with persistent pharyngeal discomfort of 3 months duration. He was not a smoker and had no other significant m edical h istory. Endoscopy revealed a smooth polypoid mass arising from the left lateral wall of the pyriform fossa. Contrast enhanced CT Scan revealed a 35 mm × 25 mm × 30 mm space occupying lesion arising from the lateral wall of the left pyriform fossa (Figure 1A). The tumour was thin walled, homogenous without any signs of calcification (Figure 1B). CT scan chest and ultrasound abdomen did not reveal any distant metastasis. Direct laryngoscopy examination confirmed the above mentioned findings and punch biopsy was performed. On histopathology, the tumour has a biphasic appearance being focally composed of gland like spaces with luminal eosinophilic material with adjoining areas showing a spindle cell component arranged in short fascicles (Figure 2). On immunohistochemistry, majority of the tumour cells were positive for pan cytokeratin (Figure 3A and B) and TLE-1 (Figure 3C and D) and negative for SOX-10, S100, CD34,CK7 and Caldesmon, favouring diagnosis of malignant biphasic synovial sarcoma (Figure 3B). Wide surgical excision was performed by lateral pharyngotomy and selective neck dissection was performed removing lymph nodes from level II to IV on the left neck side. All the resected margins were negative for invasive cancer and all the nodes were free of metastatic deposits. Postoperative course was uneventful and nasogastric feeding tube was removes on the 7 day postoperatively. He was advised adjuvant radiotherapy, which he refused. He has completed 2 years of follow up and is disease free.
Discussion
Synovial sarcomas present as well defined, painless progressive swelling. Clinically it is challenge to diagnose a synovial sarcoma as most often it masquerades as the benign pathology. The be nign presentation of the synovial sarcoma is mainly attributed to presence of the fibrous pseudo-capsule that often surrounds th e tumour [7]. Such capsulated pathology in pyriform sinus may remain silent for considerable amount of time as happened with our patient who presented with just mild discomfort in throat of three months duration. It is only after his voice changed that he sought medical attention. Radiology is not helpful in distinguishing a synovial sarcoma from the benign masses as typical radiological features of synovial sarcoma in the head and neck are homogenous masses mimicking benign growth. On computed tomography, synovial sarcoma often seems slightly hypodense with up to 30% to 50% of all cases displaying areas of calcification [8]. In our case no calcification was noted.
Histopathology is characterised by presence of spindle and epithelioid cells (Figure 2A and B). Epithelial component consists of cuboidal or tall columnar cells that form nests or glandular structures (Figure 2C and D, black arrow) and the spindle cells are densely packed in fascicles or sheets form the sarcomatous component (Figure 2B, blue arrow). Immunohistochemistry plays a crucial role for definitive diagnosis. TLE1, in view of its high sensitivity is a useful marker within the IHC panel comprising EMA, BCL2, MIC2, CD34 and CK7, especially on small biopsy samples, for substantiating a diagnosis of synovial sarcoma [9]. Pathogenesis of the synovial sarcoma has been explained on genetic basis, a reciprocal translocation between chromosome 18 and Xt (X;18) (p11.2;q11.2) generates the SYT-SSX1 or SYT-SSX2 gene usion [10,11]. This gene fusion appears to be the primary event in the pathogenesis of synovial sarcoma and can be observed in far more than 90% of patients [11,12].
Standard treatment for synovial sarcoma of the head and neck is not yet established due to rarity of disease. However, complete surgical excision with tumour free margins remains central to successful local control [13-15]. Guillou et al. reported a strong association between negative margins and local recurrence-free survival, with a median local recurrence-free survival of 179 months (88%), for those with negative margins but only 33 months (22%) for those with positive margins (p< .0001) [16]. Other authors have also reported very high recurrence of 60% to 90% after local excision only, usually within 2 years [3,17,18]. Harb et al found no prognostic association for either margin status or initial biopsy type, but found that local recurrence was more common in patients with initially positive margins than in patients with initially negative margins [19]. Adjuvant radiotherapy has been shown to improve the survival and decreases the recurrence rates, although statistical significance could not be proven due to the small sample size [19]. Fontanesi et al. from the St Jude children’s hospital reported questionable benefit with the addition of radiation for patients with adequate surgical resection and having good tumour characteristics. But in patients with incomplete resection or partial response to chemotherapy, radiation therapy provided durable local control [20]. Harb et al. recommends adjuvant radiotherapy for all patients with head and neck synovial sarcoma and systemic neoadjuvant chemotherapy for all patients with tumours of >5 cm in size, clinical or imaging evidence of local extension on presentation,or a high-risk site of presentation [19]. On the contrary the role of adjuvant chemotherapy is of questionable value. Italiano et al. reported no improvement in resected primary synovial sarcoma with either neoadjuvant or adjuvant chemotherapy [18].
argeted therapy may play important role in the management synovial sarcoma in the future. Trautmann et al. showed that inhibition of the SYT-SSC-induced WNT/ catenin signalling pathway led to induction of apoptosis and reduced tumour growth in synovial sarcoma cell lines [21]. Palbociclib, which is an inhibitor of the CD4/6-cyclin D1 axis, has been studied as a potential future treatment for a subset of synovial sarcoma patients [22]. It is likely that future studies will further emphasize the importance of targeted therapy in synovial sarcoma and move treatment approaches from research into successful clinical practice [23].
Conclusion
Despite relatively slow growth, synovial sarcoma in the head and neck has an aggressive nature and a guarded prognosis. Most important prognostic factors include tumour size and extension at the time of presentation. complete surgical resection with negative margins plays significant role in survival. Adjuvant radiotherapy improves survival, especially in the presence of the residual disease. Role of chemotherapy in the neoadjuvant or adjuvant setting needs to be studied further. Targeted therapy may play important role in the improvement of overall and disease specific survival.
References
- Sturgis E M, Potter B O (2003) Sarcomas of the head and neck region. Curr Opin Oncol 15: 239-252. [Google Scholar] [Cross Ref]
- Weiss SW, Goldblum JR (2013) Enzinger and Weiss’s soft tissue tumors. 6th ed. Philadelphia: Mosby Elsevier. [Google Scholar] [Cross Ref]
- Carrillo R, Rodriguez-Peralto JL, Batsakis JG (1992) Synovial sarcoma of the head and neck. Annal Otol Rhinol Laryngol 101: 367-370. [Google Scholar] [Cross Ref]
- Fatima SS, Din NU, Ahmad Z (2015) Primary synovial sarcoma of the pharynx: A series of five cases and literature review. Head Neck Pathol 9: 458-462. [Google Scholar] [Cross Ref]
- Jernstorm P (1954) Synovial sarcoma of the pharynx: Report of a case. Am J Clin Pathol 24: 957-961. [Google Scholar] [Cross Ref]
- Fletcher C, Bridge JA, Hogendoorn CW, Mertens F (2013) WHO classification of tumours of soft tissue and bone: WHO classification of tumours, vol. 5. World Health Org. [Google Scholar] [Cross Ref]
- Verma R, Verma RR, Verma RR, Sardana NK (2014) Synovial sarcoma: Laryngopharynx a challenge. Indian J Otolaryngol Head Neck Surg 66: 219-223. [Google Scholar] [Cross Ref]
- O’Sullivan PJ, Harris AC, Munk PL (2008) Radiological features of synovial cell sarcoma. Br J Radiol 81: 346-356. [Google Scholar] [Cross Ref]
- Rekhi B, Basak R, Desai SB, Jambhekar NA (2012) Immunohistochemical validation of TLE 1, a novel marker, for synovial sarcoma. Indian J Med Res 136: 766-775. [Google Scholar] [Cross Ref]
- Bridge JA, Bridge RS, Borek DA, Shaffer B, Norris CW (1988) Translocation t (X;18) in orofacial synovial sarcoma. Cancer 62: 935-937. [Google Scholar] [Cross Ref]
- Kawai A, Woodruff J, Healey JH, Brennan MF, Antonescu CR (1998) SYT-SSX gene fusion as a determinant of morphology and prognosis in synovial sarcoma. N Engl J Med 338: 153-160. [Google Scholar] [Cross Ref]
- Ladanyi M, Antonescu CR, Leung DH, Woodruff JM, Kawai A, et al. (2002) Impact of SYT-SSX fusion type on the clinical behavior of synovial sarcoma: A multi-institutional retrospective study of 243 patients. Cancer Res 62:135-140. [Google Scholar] [Cross Ref]
- Gronchi A, Casali PG, Mariani L, Miceli R, Fiore M, (2005) Status of surgical margins and prognosis in adult soft tissue sarcomas of the extremities: A series of patients treated at a single institution. J Clini Oncol 23: 96-104. [Google Scholar] [Cross Ref]
- Pisters PW, Leung DH, Woodruff J, Shi W, Brennan MF (1996) Analysis of prognostic factors in 1,041 patients with localized soft tissue sarcomas of the extremities. J Clin Oncol 141676-1689. [Google Scholar] [Cross Ref]
- Zagars GK, Ballo MT, Pisters PW, Pollock RE, Patel SR (2003) Prognostic factors for patients with localized softâ?tissue sarcoma treated with conservation surgery and radiation therapy: An analysis of 1225 patients. Cancer: Interdis International J Am Cancer Soc 97: 2530-2543. [Google Scholar] [Cross Ref]
- Guillou L, Benhattar J, Bonichon F, Gallagher G, Terrier P (2004) Histologic grade, but not SYT-SSX fusion type, is an important prognostic factor in patients with synovial sarcoma: A multicenter, retrospective analysis. J Clin Oncol 22: 4040-4050. [Google Scholat] [Cross Ref]
- Balakrishnan V, Flatman S, Dixon BJ, Lyons B (2012) Synovial sarcoma of the pharynx causing airway obstruction. Med J Aust 196: 72-73. [Google Scholat] [Cross Ref]
- Italiano A, Penel N, Robin YM, Bui B, Le Cesne A (2009) Neo/adjuvant chemotherapy does not improve outcome in resected primary synovial sarcoma: A study of the french sarcoma group. Annals Oncol 20: 425-430. [Google Scholar] [Cross Ref]
- Harb WJ, Luna MA, Patel SR, Ballo MT, Roberts DB (2007) Survival in patients with synovial sarcoma of the head and neck: Association with tumor location, size, and extension. Head Neck: J Sci Specialties Head Neck 29: 731-740. [Google Scholar] [Cross Ref]
- Fontanesi J, Pappo AS, Parham DM, Hurwitz CA, Rao BN (1996) Role of irradiation in management of synovial sarcoma: St. Jude children's research hospital experience. Med Pediatric Oncol: Official J SIOP- Intern Soc Pediatric Oncol 26: 264-267. [Google Scholar] [Cross Ref]
- Trautmann M, Sievers E, Aretz S, Kindler D, Michels S (2014) SS18-SSX fusion protein-induced Wnt/β-catenin signaling is a therapeutic target in synovial sarcoma. Oncogene. 33: 5006-5016. [Google Scholar] [Cross Ref]
- Li X, Seebacher NA, Garbutt C, Ma H, Gao P (2018) Inhibition of cyclin-dependent kinase 4 as a potential therapeutic strategy for treatment of synovial sarcoma. Cell Death Dis 9: 446. [Google Scholar] [Cross Ref]
- Bukachevsky RP, Pincus RL, Shechtman FG, Sarti E, Chodosh P (1992) Synovial sarcoma of the head and neck. Head Neck 14: 44-48. [Google Scholar] [Cross Ref]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 