Case Report, Clinic Oncol Case Rep Vol: 8 Issue: 1
Case Report: Managing Adverse Outcomes in a Laryngeal Cancer Patient
Mitchell Sager*, Shaileshkumar Desai, Avi Desai
Department of Internal Medicine, American University of the Caribbean, Michigan, USA
*Corresponding Author: Mitchell Sager
Department of Internal Medicine, American University of the Caribbean Medicine, Michigan, USA
E-mail: mmsager1162@gmail.com
Received: July 23, 2025, Manuscript No. COCR-25-168093
Editor assigned: July 26, 2025, PreQC No. COCR-25-168093(PQ)
Reviewed: August 04, 2025, QC No. COCR-25-168093
Revised: August 06, 2025, Manuscript No. COCR-25-168093(R)
Published: August 16, 2025, DOI: 10.4173/cocr.8(1).372
Citation: Sager M. et al., (2025) Case Report: Managing Adverse Outcomes in A Laryngeal Cancer Patient. Clin Oncol Case Rep 8:1.
Abstract
It could be said that laryngeal cancer is one of the most unfortunate disorders to befall patients. Unfortunately, the painful treatment can be a small consolation to a patient’s sense of well-being. Primary care and hospital physicians may not be familiar with proper management of patients who relapse, as laryngeal cancer is handled by specialists and frankly it can be rather complicated. An additional challenge presents itself with laryngeal cancer. The emotional and physical burden of this disease can further stretch a patient’s resolve and the medical team’s morale, possibly leading to adverse outcomes. This case report details a 50 year old male with a history of total laryngectomy for stage IVa squamous cell carcinoma with a persistent oropharyngeal tumor. This caused the patient to suffer frequent admission to the hospital for problems including bilateral internal jugular vein thrombosis and infection. This report will detail the particularities of treating patients with complicated oropharyngeal cancers post laryngectomy.
Keywords: Laryngeal cancer, Thrombosis, Laryngectomy, Squamous cell carcinoma
Introduction
Squamous cell carcinoma is the most common type of laryngeal cancer and as such, smoking is the most common risk factor [1]. The staging criteria is split between the three tumor locations which are infraglottic, glottic and supraglottic [2]. It is estimated that there will be 13,020 cases of laryngeal cancer in 2025, typically 35% of cases are supraglottic [3]. The treatment of laryngeal cancer always involves radiation and/or surgery, the former is solely utilized if the lesion is small [4]. The patient of this case initially presented with hoarseness and had a history of smoking beyond thirty years. A CT scan and laryngoscopy revealed a 1.6 cm mass that was exophytic and friable, which made surgery inevitable. As mentioned, the patient suffered a recurrence of cancer growth less than two years later. One cohort study with over 1,000 patients calculated the general risk of recurrence for squamous cell laryngeal cancer to be 20.5% [5].
However, the risk was greater among supraglottic tumors and typically occurred within the first three years after treatment [5]. Both of these data points match our patient’s history. The specifics of management are largely functional and integrative. Patients need their care team to have specific, structured guidelines for management and ensure that patients are being treated at appropriate care sites such as intensive units and cancer centers.
Case Presentation
The patient was a 48-year-old caucasian male complaining of hoarseness at the initial presentation. A CT scan showed a nasopharyngeal mass and thickening of the vocal chords. A biopsy revealed stage IV, p-16 negative squamous cell carcinoma of the right false vocal chord. The patient began treatment with cisplatin every three weeks in addition to radiation in accordance with HRG-HN009. Several months after beginning treatment, the patient presented to the emergency room for nausea, vomiting and difficulty tolerating oral intake. Inpatient management was required and the patient received fluids, anti-emetics, steroids and treatment for oral thrush. A PET scan roughly six months after diagnosis showed considerable reduction in tumor size but unfortunately showed a paratracheal lymph node concerning for metastasis. CRT therapy continued for another three months afterward. A PET scan was repeated one month after CRT completion and revealed a stable tumor size and a reduction in the concerning lymph node’s metabolic activity. Unfortunately, the main exophytic tumor was persistent. Biopsies taken five months after the previously mentioned PET scan showed benign ulcerated squamous mucosa of the epiglottis and mucosa of the left vocal mucosa but nothing else. The tissue changes were consistent with radiation induced dysplasia. The exophytic mass remained consistent with p-16 negative squamous cell carcinoma. Laryngectomy, partial pharyngectomy, right hemithyroidectomy, cricopharyngeal myotomy and bilateral neck dissection were performed roughly five months later. Unfortunately, the patient presented to the emergency room only a month after surgery for neck “spasms.” A CT revealed a 5.8 × 4.2 × 3.5 cm mass in the posterior oropharynx, which was inseparable from the epiglottis. The patient returned to the emergency room only a week later for neck pain, nausea and vomiting. The patient was admitted and began to complain of a severe, predominantly right sided headache with pain extending from the skull down to the neck. The patient reported light sensitivity but no neurological deficits were noted. Lab values were significant for mild leukocytosis between 10 and 11 k/ mcl for about three days.
The patient’s platelets remained elevated in the mid-400s (k/mcl). MRA revealed thrombosis of the left and right internal jugular veins. The right IJV was suffering from almost complete occlusion. The thrombosis of the left internal jugular vein was diffuse and involved the jugular bulb, transverse sinus and up to the sigmoid sinus. Neurosurgery was consulted and intervention was not advised. Anticoagulation with enoxaparin was initiated. Hydromorphone was effective for pain control but only for an hour to two. Buprenorphine was eventually initiated and replaced oxycodone. The patient was discharged on apixaban and buprenorphine notably but returned to the hospital about a week later due to inability to tolerate pain. The patient reported only oxycodone and hydromorphone control the pain. It should be noted that the patient was considerably malnourished on admission. The patient’s ability to speak was limited at this point, only some words could be communicated.
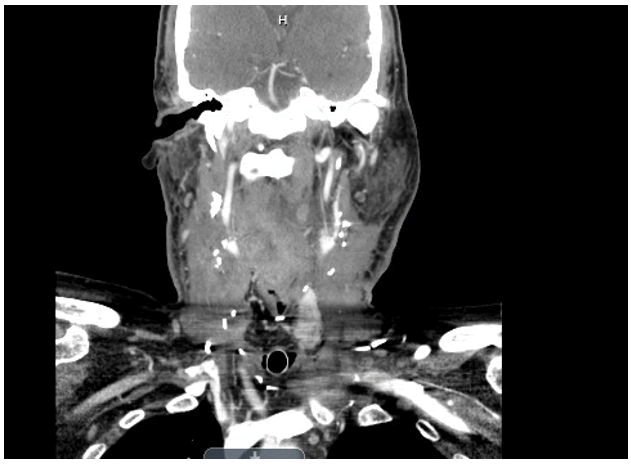
Pain management sought to try valproate and dexamethasone for head pain in addition to hydromorphone. The consideration of thrombectomy for the venous thrombosis became a discussion if there was no improvement on duplex ultrasound, which showed limited if any changes. However, neurovascular still advised against intervention. The patient had begun to suffer sinus pauses as well, cardiology considered pacing support but in any case he was kept on telemetry. It was thought to be caused by respiratory distress and intense pain. An ECHO was conducted which fortunately showed normal EF. At this point, the patient was suffering from hyponatremia, folate deficiency, thrombocytosis, leukocytosis, and dysphagia. Additionally, the patient was not able handle salivary secretions, thus requiring intensive medical management. In terms of pain control, the patient was now receiving hydromorphone 0.5 mg q3h and a 75 mcg transdermal fentanyl patch.The patient still suffered from headache but this controlled his pain to a greater degree. Careful attention was paid to tracheal secretions as an episode of desaturation to 88% occurred, thus the patient had suction nearby preferably at all times. The patient suffered an episode of hypercalcemia at 16.4, treated with calcitonin. BMP and other lab values were ordered q12h to stay ahead of any abnormalities. Additionally, an acute kidney injury occurred with Creatinine of 2.6 and BUN of 19. The treatment plan was to give 150 ml/hr of normal saline along with potassium and phosphorus supplementation. The patient suffered increasingly prolonged sinus pauses, one episode over seven seconds. A pacemaker was implanted accordingly. The patient was also suffering from hypotension and midodrine was used in addition to vasopressors when necessary. A PEG tube was attempted but failed due to esophageal stenosis. The patient had an episode of hematemesis, about one liter of blood was lost. The patient was transferred to the ICU for care. ENT recommended packing the throat if bleeding occurred again and ventilating though the laryngostoma The patient was taken to the operating room about a day after the hematemesis episode for PEG tube placement and laryngoscopy. Anti-coagulation was recommended to be held according to ENT, as tumor bleeding was held responsible for the episode of hematemesis. The patient stabilized over the course of about a week and was discharged. The patient returned via EMS after suffering excessive secretions (salivation) and oxygen desaturations upon sitting up. The patient was admitted and treated empirically for an infection. Hemoglobin was 10.1, WBC 22.3 and platelets 561 k/mcl on admission. The bilateral IJV thrombosis still had not resolved at this point. Excessive secretions and blood were seen throughout the laryngostoma. It appeared the patient had either tracheitis or a pseudomonas infection. The patient also had excessive neck swelling, CT showed a necrotic mass on the left side of the neck. At this point, the patient was transferred to a cancer facility for further care (Figure 1).
Figure 1: MRA revealed bilateral thrombosis of the internal jugular veins plural.
Discussion
The two main goals for patients with recurrent malignancies, particularly head and neck cancer, is to simplify treatment and stay abreast of complications. A theme running through the case discussion is clearly that of responding to adverse events. The problem is that patients with refractory cancer such as here, cannot tolerate adverse events very well. They have a high baseline of pain, suffer from nutritional deficiency, and have a limited ability to communicate. It was evident here that it was very difficult to keep the patient stable once the cancer had spread. It goes without saying that patients presenting with hoarseness who also have a smoking history, should be worked up without delay. The bilateral thrombosis of the IJV was a critical junction in the patient’s course. This incident brought his pain out of control and it took a considerable amount of time to get it stabilized. The combination of severe pain and respiratory distress was theorized to be responsible for the recurrent episodes of asystole that ultimately required a pacemaker. This was greatly exacerbated by the pain from bilateral IJV thrombosis. Internal jugular vein thrombosis in supraglottic squamous cell carcinoma has been reported in the literature [5]. Therefore, we would like to propose guidelines for prevention. Patients with supraglottic SCC specifically but not exclusively, should be monitored for thrombocytosis monthly. A study of patients with platelets above 443 × 109/L had a risk of venous thrombosis of 34% after one year [6]. This patient had a platelet count in that range. As a general rule of thumb, we propose that laryngeal SCC patients with thrombocytosis beyond three consecutive months should be considered for anticoagulation. Another issue was that lab values continued to fluctuate outside of clinically safe ranges which required constant correction. Repeat labs every nine to twelve hours is appropriate for inpatient management of severe cases such as this. It is imperative to stay ahead of complications. Caloric deficiency was an underlying detriment to the patient’s condition. Laryngeal cancer patients should be evaluated bimonthly for problems regarding oral intake and nutrition. Nutritional support was detected late in this patient and further delayed due to esophageal stenosis. All in all, streamlining patient care with general guidelines will help physicians stay ahead of complications. Once a condensable insult occurs to the patient’s health, such as the IJV thrombosis or malnourishment, it is extremely difficult to recover.
Conclusion
Several conclusions can be drawn from the patient’s course. Firstly, outpatient monitoring and subsequent intervention could have significantly improved the patient’s outcome as noted in our proposed guidelines. Secondly, pain control may be varied depending on the patient but regardless, an effective regimen must be found early. Excess pain was in no small part responsible for deleterious effects in the patient’s outcome. Another critical aspect of treatment is determining when ICU and cancer center treatment is necessary versus a standard medical floor or even outpatient treatment. Lastly, adequate emotional and social support is very important for these patients. Lest we forget that physicians are also responsible for the patient’s mental wellbeing while under our treatment.
Acknowledgment
I would like to extend a special thanks to Janice Jones.
References
- Koroulakis A, Agarwal M (2025) Laryngeal Cancer. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
- Laryngeal Cancer Staging (2021) Stages of throat Cancer. American Cancer Society.
- Throat Cancer Statistics. Cases of throat cancer per year. American Cancer Society.
- PDQ® Adult Treatment Editorial Board (2025) PDQ Laryngeal Cancer Treatment. Bethesda, MD: National Cancer Institute.
- Tudor F, Kosec A, Pegan A (2024) Internal jugular vein thrombosis caused by invasive pharyngeal cancer: A case report and literature review. Braz J Otorhinolaryngol 90: 101425.
[Crossref] [Google Scholar] [PubMed]
- Simanek R, Vormittag RC, Ay C, Alguel G, Dunkler D, et al. (2010) High platelet count associated with venous thromboembolism in cancer patients: Results from the Vienna Cancer and Thrombosis Study (CATS). J Thromb Haemost 8: 114-120.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi