Case Report, Clin Res Orthop Vol: 2 Issue: 1
Heterotopic Ossification- Induced Osteomyelitis 3 Years after a Closed Both-Bone Forearm Fracture in a Pediatric Patient: A Case Study
Arsalan Amin1* and Carayannopoulos NL2
1University of Texas Medical Branch at Galveston, Galveston, TX, USA
2Houston Institute for Sports Medicine and Orthopaedics, Houston, TX, USA
*Corresponding Author : Arsalan Amin
Houston Institute for Sports Medicine and Orthopaedics, 2000 Crawford St. Suite 1750, Houston, TX 77002, USA
Tel: + (972) 904 – 3958
E-mail: Arsalan.Amin@bcm.edu
Received: July 14, 2017 Accepted: February 09, 2018 Published: February 16, 2018
Citation: Amin A, Carayannopoulos NL (2018) Heterotopic Ossification-Induced Osteomyelitis 3 Years after a Closed Both-Bone Forearm Fracture in a Pediatric Patient: A Case Study. Clin Res Orthop 2:1.
Abstract
Osteomyelitis is an infection, predominately bacterial in origin, of the bone which incites an acute inflammatory response with subsequent bacterial and inflammatory dissemination to the cortex and periosteum. Microorganism seeding typically occurs via hematogenous spread form existing bacteremia, direct inoculation secondary to penetrating trauma, or contiguous spread from localized infection. Treatment of osteomyelitis typically requires a multidisciplinary approach, including long term oral and/or intravenous antibiotic therapy and surgical intervention. Osteomyelitis as a secondary complication of closed fractures is a rare occurrence with less than 50 document cases reported in literature to the extent of the author’s knowledge. We report an atypical case of acute osteomyelitis originating from a localized bony
spicule in a pediatric patient, more than 3 years after a surgically treated closed distal forearm both-bone (radius and ulna) fracture. The patient in this report exhibited an atraumatic nine-month course of recurrent abscess formation and localized inflammation, despite surgical debridement and multiple rounds of antibiotic therapy. A bony spicule noted on x-ray, which the authors believe formed from early consolidation of heterotopic ossification fragments, was surgically excised, after which the patient ceased to develop recurrent abscesses. Histological analysis of the spicule revealed findings consistent with a definitive diagnosis of S. aureus (MSSA) acute osteomyelitis. In conclusion, to the extent of the author’s knowledge, this is the first reported case of acute osteomyelitis complicating a closed fracture
and localized to a bony fragment, which formed from heterotopic ossification, a known complication of fractures.
Keywords: Acute osteomyelitis; Heterotopic ossification (HO); Pediatric fracture; Fracture complication; Both-bone forearm fracture (BBFFx); Staphylococcus aureus (MSSA) osteomyelitis
Introduction
Osteomyelitis, an infection of the marrow and bone, incites an acute inflammatory response with subsequent bacterial and inflammatory dissemination to the cortex and periosteum through Volkmann’s canals and the Haversian system [1,2]. Microorganism seeding of the bone occurs via: hematogenous spread from bacteremia, direct inoculation from penetrating trauma, or contiguous spread from local infection. Hematogenous spread is the predominant underlying pathogenesis in the pediatric (children<18-years-old) population, because of the rich vascular supply associated with developing skeletal tissue [2]. Staphylococcus aureus, a gram-positive cocci, is the most commonly isolated organism in children and adults with Osteomyelitis [3-7]. Treatment modalities typically involve both surgical intervention and long-term antibiotic therapy. Untreated, the infection can progress to a chronic stage and is associated with complications including: pathologic fractures, growth arrest, septic arthritis, and sepsis [1,2]. We present a case of acute osteomyelitis originating from an isolated bony fragment in a pediatric patient more than 3 years after a surgically treated closed distal forearm both-bone (radius and ulna) fracture. To the extent of our knowledge, this is the first reported case of osteomyelitis localizing to a bony spicule which formed from consolidation of heterotopic ossification fragments.
Case Report
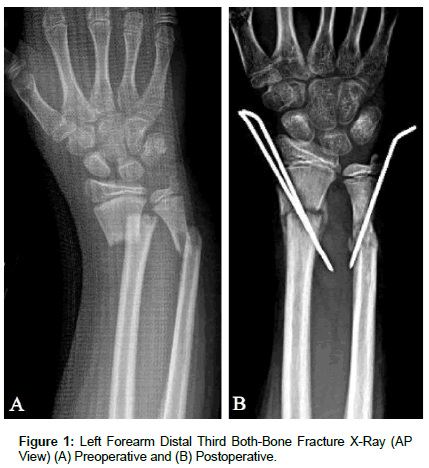
[04/13/2012] A 12-year-old Hispanic male was evaluated by the Orthopaedic Trauma service for a chief complaint of left forearm pain, after suffering a fall while playing soccer. The patient endorsed pain at the left wrist with range of motion, but denied constitutional symptoms and any other recent inciting trauma or injuries. On physical exam, the patient was noted to have a gross deformity of the left wrist and had tenderness to palpation overlying the distal radius and ulna. He was neurovascularly intact. Radiography (Figure 1) of the Left Upper Extremity (LUE) provided a definitive diagnosis of a skeletally immature individual with a closed distal radius and ulnar (both-bone) fracture with 100% displacement and 2 centimeters (cm) of shortening; subsequently the patient and his parents elected to pursue surgical intervention. Closed reduction and percutaneous pinning with placement of two 0.62 K-wires from the radial styloid distally to the medial aspect of the radial shaft proximally was performed to address the distal radius fracture and restore mechanical alignment. Closed reduction of the distal ulna fracture proved difficult so the procedure was converted to an open reduction through a direct approach to the ulnar fracture between the Extensor Carpi Ulnaris and Flexor Carpi Ulnaris. A 0.62 K-Wire was placed from distal to proximal through the ulnar shaft to restore mechanical alignment; dorsal comminution of the ulnar shaft was noted intraoperatively and consequently may have contributed to the difficulty with obtaining successful closed reduction.
During the subsequent three-month period, the patient continued to follow-up in clinic for assessment of his postoperative fracture healing. At his initial follow-up three weeks after surgery, the radial pins were removed without complication and silver nitrate was applied to the wound. Otherwise, the patient was without any signs of infection and exhibited a normal postoperative course with respect to progressive bony healing, decreased pain and tenderness, and improved range of motion. During each subsequent postoperative evaluation, the patient progressively improved and exhibited appropriate bone healing (Figure 2), including callus formation and bony remodeling. Additionally, he was never found to have neurovascular compromise of the left upper extremity, nor did he demonstrate signs or symptoms of an infection. At the time of his final postoperative evaluation at 3-months, the patient exhibited appropriate fracture healing alongside symmetrical and equal range of motion for the upper extremities bilaterally; therefore, he was cleared to return to physical activity and exercise of the LUE without restrictions.
[08/19/2015] The patient, now fifteen years old, presented more than three years after the initial LUE both-bone forearm fracture and subsequent surgical intervention complaining of increased pain, localized swelling, erythema and drainage along the radial styloid of 5-days duration. He denied recent inciting trauma or injuries, as well as fever or chills. The physical exam was benign aside from a 1 cm x 1 cm localized fluctuant swelling with surrounding erythema and mild tenderness to palpation overlying the radial styloid. Radiographs of the left forearm demonstrated healed and remodeled radius and ulna fractures; additionally, there were no changes consistent with concern for the presence of sequestrum. Furthermore, the ulna exhibited growth arrest, shortening, and a negative variance, and a small amount of heterotopic ossification (HO) was noted at the volar aspect of the distal radius. The patient was diagnosed with a left forearm abscess and discharged on Cephalexin antibiotic therapy. The radiographic findings were benign findings associated with the patient’s previous fracture pattern. Over the following 4-month period, the patient exhibited a pattern of draining abscess resolution while on outpatient antibiotic therapy and abscess recurrence upon completion and discontinuation of antibiotics. He denied having inciting trauma or injury during this period as well as absent development of constitutional symptoms. His medical work-up included assessment of the white blood cell (WBC) count and inflammatory markers (ESR and CRP), which were all found to be within normal limits. Needle aspiration of the abscess fluid for wound cultures did not yield microbial growth and MRI of the left wrist was negative for the presence of a sequestrum suggestive of osteomyelitis. The patient and his family opted to pursue surgical incision, debridement, and bone biopsy. [12/18/2015] Exploration of the wound revealed no pus; however, a sinus tract communicating with the distal radius was appreciated. Wound cultures and a bone biopsy of the distal radius were both negative. He was discharged with a prescription for a tenday course of Cephalexin antibiotic therapy.
[01/27/2016] At his one month postoperative follow-up, the patient presented with an erythematous fluctuant mass overlying his incision which had been present for three days; he denied inciting trauma or injury, fevers, chills, or drainage. Serosanguinous fluid aspirated from the abscess was cultured and grew 1+ Staphylococcus Aureus (MSSA) with susceptibility to several antibiotics (Table 1). The patient was referred to the Pediatric Infectious Disease service and admitted to the hospital for a working diagnosis of Osteomyelitis. Diagnostic workup revealed the WBC count and CRP were within normal limits, ESR was slightly elevated at 11 mm/Hr (ref. range: 0-10 mm/Hr), and an MRI of the left wrist revealed mild bony edema at the distal radial diaphysis with adjacent soft tissue swelling and no erosive changes, consistent with a nonspecific bony inflammatory response. During his two-day admission, the patient received Vancomycin 1 gram (g) intravenously every twelve hours and Rifampin 600 milligrams (mg) intravenously every 24 hours. He was discharged on day three with an antibiotic therapy regimen consisting of Cephalexin 750 mg by mouth every six hours for twenty-eight days and Rifampin 300 mg every twelve hours for fourteen days.
| Susceptibility | |
|---|---|
| Antibiotics | Staphylococcus aureus |
| Susceptibility Testing | |
| Clindamycin | <=0.25 Susceptible |
| Erythromycin | <=0.25 Susceptible |
| Oxacillin | <=0.25 Susceptible |
| Penicillin | Resistant |
| Rifampin | <=0.5 Susceptible |
| Tetracycline | <=1 Susceptible |
| Trimethoprim/Sulfamethoxazole | <=10 Susceptible |
Table 1: Wound culture staphylococcus aureus antibiotic susceptibilities.
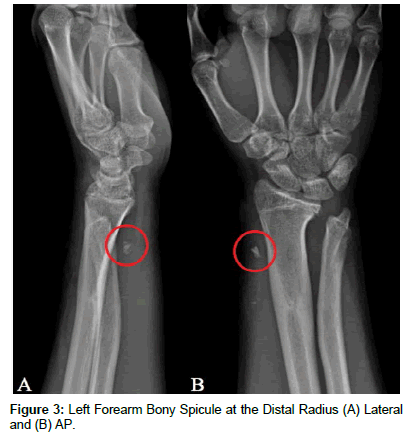
[04/11/2016] The patient again presented to clinic with a recurrence of the abscess and one week of progressively worsening swelling and erythema at the left distal radius; he had otherwise been asymptomatic during the interim following his hospital discharge and off antibiotic therapy for six weeks. Serosanguinous fluid aspirated from the abscess grew 2+ Staphylococcus Aureus (MSSA) with a similar antibiotic susceptibility profile as had been previously determined. Plain films of the left forearm revealed the presence of a bony spicule in the soft tissue at the lateral aspect of the distal radius (Figure 3); it is suspected that the fragment is a result of possible early consolidation of the heterotopic ossification previously noted. The patient and his parents opted to pursue surgical wound debridement and excision of the bony fragment. [05/09/2016] Surgical exploration of the left wrist first extensor compartment revealed notable inflammatory changes and synovitis, with thickening of the sheath. Additionally, the spicule previously noted on x-ray alongside necrotic fatty tissue was identified and subsequently removed. Acute osteomyelitis of the bone fragment was diagnosed secondary to histologic features of neutrophilic granulocyte infiltrate and necrotic bone tissue. The patient was discharged on Cephalexin antibiotic therapy one gram by mouth daily for 28 days. He has not had a recurrence of the abscess over the past year and has been doing well, without the need for additional antibiotic therapy or surgical intervention.
Discussion
Osteomyelitis as a secondary complication of closed fractures, is a rare occurrence and there exist few documented cases, which have been reported in literature [8-25]. Typically, the infection is associated with Staphylococcus aureus; however, other commonly isolated organisms include Streptococcus pyogenes, Streptococcus pneumoniae, Pseudomonas with puncture wounds to the plantar foot, and Salmonella in Sickle-Cell patients [2,3,5-7]. A characteristic feature of these microorganisms is the ability to synthesize a three-dimensional biofilm, which dampens the immune response and antibiotic efficiency [5]. There exist three primary mechanisms which allow for microorganism seeding of bone: hematogenous spread, penetrating trauma, or contiguous spread from adjacent tissue. Orthopaedic literature has demonstrated that osteomyelitis typically affects the metaphyseal region of long bones (e.g. femur, tibia, humerus, radius) because of the associated tortuous vascular supply which allows for greater bacterial aggregation and decreased inflammatory response [4,6,7,26]. Nade provides an in-depth description of the underlying vascular morphology and pathophysiology allowing for metaphyseal bacterial seeding [26]. Bacterial and inflammatory cell dissemination through Volkmann’s canals and the Haversian system causes a lifting of the periosteum, further compromising the vascular supply to the affected region [1,2,4]. Ischemic injury contributes to segmental bone necrosis and the formation of dead bony tissue, otherwise recognized as sequestrum [1,2]. The avascular sequestrum inhibits antibiotic penetration while simultaneously serving as a necrotic nidus for continued bacterial proliferation [2]. Definitive treatment classically involves a multidisciplinary approach of intravenous and/ or oral antibiotic therapy and surgical debridement to eradicate the infection. Osteomyelitis as described in our patient is inconsistent with the findings previously described. The infection localized not to the fracture site as has been reported in literature, rather to a bony fragment. We speculate the spicule formed from early consolidation of the heterotopic ossification which was first noted on x-ray during the initial presentation three years out from his initial injury. Studies have demonstrated that while heterotopic ossification maybe continuous with the anatomical bone tissue, the periosteum is not typically involved [27-29]. Although devoid of periosteal vasculature, HO exhibits mature cancellous and lamellar bone, innervating vessels, and minor hematopoietic potential [27,30,31]. We believe the heterotopic ossification fragment became hematogenously seeded with S. Aureus and progressively became devascularized, which allowed for continued bacterial growth in the presence of antibiotic therapy.
The majority of cases described in literature also identified a primary infectious source, predominately upper respiratory tract or urinary tract infections, contributing to the development of acute hematogenous osteomyelitis [8,10,12,13,17,22,24,25]. A review of the literature suggest that patients also exhibit constitutional symptoms such as fever and have a corresponding inflammatory response, including elevated WBC with a proportional increase in neutrophils, and elevated ESR and CRP [8-9,22-24]. Additionally, case studies reveal that patients typically exhibited findings on imaging consistent with Osteomyelitis and intraoperatively purulent material was encountered [8-13,15-21,23-25]. Although the patient in our study exhibited localized inflammatory symptoms of pain, erythema, swelling, and tenderness as have been described in previous cases; there was no evidence suggestive of bacteremia, penetrating trauma, or any infectious etiology. Interestingly, throughout the approximate nine-month interval during which the patient was evaluated, he did not exhibit leukocytosis or an elevated CRP, and there was only a single instance of an elevated ESR at 11 mm/Hr (ref. range 0-10 mm/ Hr). Nearly five months after his initial presentation for concern of an abscess, S. aureus was isolated from wound cultures, which had previously been negative despite multiple recurrences of the abscess. Of note, the patient had completed multiple rounds of antibiotic therapy and undergone surgical exploration and debridement of the wound. Furthermore, imaging did not reveal changes consistent with the formation of a sequestrum; however, a nonspecific bony inflammatory response was noted on MRI. Heterotopic ossification had been noted on plain films at the time of the initial presentation for abscess formation and subsequently, a bone fragment was identified approximately eight months later. During the initial operation, purulent material was not encountered and intraoperative wound cultures and bone biopsy were negative for the presence of infection. Histological changes consistent with acute osteomyelitis and sequestrum formation were identified after the second surgical intervention to excise the bony spicule.
A review of the literature revealed cases with osteomyelitis secondarily complicating a closed fracture have occurred with a variable timeline, ranging from a few days to many years after the initial injury. The delay in diagnosis is attributed predominately to a low clinical index of suspicion, based on the very low incidence of osteomyelitis complicating closed fractures. Similarly, osteomyelitis was not atop the list of differential diagnoses in our patient based on the timeline, presenting symptoms, and clinical findings. Additionally, the patient previously had an unremarkable postoperative course following his closed both-bone forearm fracture. The infection became progressively more concerning because of the recurrent nature of inflammatory abscess formation, despite multiple rounds of antibiotic therapy and a surgical intervention. Definitive diagnosis and resolution was reached only after the bony spicule noted on plain films was surgically excised and exhibited features of acute osteomyelitis on histology. We speculate that the bony fragment formed from consolidation of the heterotopic ossification which had progressively developed and is a known potential complication of musculoskeletal trauma. Furthermore, we believe that the metabolically active bone fragment was hematogenously seeded by bacteria and eventually served as a necrotic nidus for continued S. aureus growth; however, the source of infection remains unknown. Additionally, it remains unclear as to why histologic changes were consistent with acute rather than chronic osteomyelitis, given the recurrent nature of abscess formation and inflammation spanning a period of nine months. To the extent of the authors’ knowledge, this is the first known reported case of osteomyelitis complicating a closed fracture a few years after the initial injury and localizing to a bony spicule, rather than the previous fracture site.
In conclusion, we present the case of a 15-year-old male who developed osteomyelitis at the distal aspect of his left forearm, more than three years after suffering from a closed both-bone distal forearm fracture. The initial injury was addressed with surgical intervention and the patient exhibited appropriate healing clinically and on radiographs with an uncomplicated postoperative period. The patient was evaluated over a nine-month period, during which he exhibited recurrent abscess formation overlying the left radial styloid alongside localized inflammatory symptoms, in spite of multiple rounds of antibiotics and a surgical debridement. Additionally, the patient did not exhibit clinical or radiographic signs or findings on bone biopsy consistent with osteomyelitis, further delaying an appropriate diagnosis in the presence of an already low index of suspicion. Complete resolution was achieved with a second surgical intervention to excise the bony spicule which was noted on x-ray. A diagnosis of acute osteomyelitis was confirmed with histological analysis of the excised bone fragment and the patient did not experience additional recurrences of inflammatory abscess formation.
References
- Kumar V, Abbas AK, Aster JC (2014) Robbins and Cotran Pathologic Basis of Disease. (9th Edtn), Elsevier, Philadelphia, USA.
- Whyte NS, Bielski RJ (2016) Acute Hematogenous Osteomyelitis in Children. Pediatr Ann 45: 204-208.
- Kumar V, Abbas AK, Aster JC (2012) Robbins SL. Robbins Basic Pathology (9th edtn). Philadelphia, USA.
- Blickman JG, van Die CE, de Rooy JW (2004) Current imaging concepts in pediatric osteomyelitis. Eur Radiol 14: 55-64.
- Beck-Broichsitter BE, Smeets R, Heiland M (2015) Current concepts in pathogenesis of acute and chronic osteomyelitis. Curr Opin Infect Dis 28: 240-245.
- Funk SS, Copley LA (2017) Acute Hematogenous Osteomyelitis in Children: Pathogenesis, Diagnosis, and Treatment. Orthop Clin North Am 48: 199-208.
- Carek PJ, Dickerson LM, Sack JL (2001) Diagnosis and management of osteomyelitis. Am Fam Physician 63: 2413-2420.
- Labianca L, Montanaro A, Turturro F, Calderaro C, Ferretti A (2013) Osteomyelitis caused by Pantoea agglomerans in a closed fracture in a child. Orthopedics 36: 252-256.
- Ebong WW (1980) Acute osteomyelitis three years after a closed fracture in an adult with sickle-cell anemia. A case report. J Bone Joint Surg Am 62: 1196-1198.
- Veranis N, Laliotis N, Vlachos E (1992) Acute osteomyelitis complicating a closed radial fracture in a child. A case report. Acta Orthop Scand 63: 341-342.
- Govender S, Charles RW, Ballaram RS, Achary DM (1988) Vertebral osteomyelitis after a closed fracture of the spine. A case report. S Afr Med J 73: 124-126.
- Canale ST, Puhl J, Watson FM, Gillespie R (1975) Acute osteomyelitis following closed fractures. Report of three cases. J Bone Joint Surg Am Apr 57: 415-418.
- Hardy AE, Nicol RO (1985) Closed fractures complicated by acute hematogenous osteomyelitis. Clin Orthop Relat Res 201: 190-195.
- Marshman LA, Allison D, Molloy CJ (2009) Acute haematogenous infection of a closed vertebral fracture. J Clin Neurosci 16:1643-1646.
- Dunsmuir RA, Barnes SJ, McGarrity G (2006) "Goalkeeper's hip": acute haematogenous osteomyelitis secondary to apophyseal fractures. Br J Sports Med 40: 808-809.
- Fellmeth BD, DaSilva RM, Spengler DM (1988) Hematogenous osteomyelitis complicating a closed compression fracture of the spine. J Spinal Disord 1:168-171.
- Watson FM, Whitesides TE (1976) Acute hematogenous osteomyelitis complicating closed fractures. Clin Orthop Relat Res 117: 296-302.
- Aalami HB (1978) Acute osteomyelitis following a closed fracture. Injury 9: 207-208.
- Baharuddin M, Sharaf I (2001) Acute haematogenous osteomyelitis: an unusual complication following a closed fracture of the femur in a child. Med J Malaysia 56: 54-56.
- Baskaran S, Nahulan T, Kumar AS (2004) Close fracture complicated by acute haematogenous osteomyelitis. Med J Malaysia 59: 72-74.
- COZEN L (1958) Four unusual cases of osteomyelitis in adults. West J Surg Obstet Gynecol 66: 36-39.
- Cuschieri J, Kralovich KA, Patton JH, Horst HM, Obeid FN, et al. (1999) Anterior mediastinal abscess after closed sternal fracture. J Trauma 47: 551-554.
- Stevens QE, Seibly JM, Chen YH, Dickerman RD, Noel J, et al. (2007) Reactivation of dormant lumbar methicillin-resistant Staphylococcus aureus osteomyelitis after 12 years. J Clin Neurosci 14: 585-589.
- Milgram JW, Romine JS (1982) Spontaneous osteomyelitis complicating a compression fracture of the lumbar spine: a case report. Spine 7: 179-182.
- Sefton GK (1982) Osteomyelitis after closed femoral fracture in a child. J R Coll Surg Edinb 27: 113.
- Nade S (1983) Acute haematogenous osteomyelitis in infancy and childhood. J Bone Joint Surg Br 65: 109-119.
- Shehab D1, Elgazzar AH, Collier BD (2002) Heterotopic ossification. J Nucl Med 43: 346-353.
- Jensen LL1, Halar E, Little JW, Brooke MM (1987) Neurogenic heterotopic ossification. Am J Phys Med 66: 351-363.
- Kurer MH, Khoker MA, Dandona P (1992) Human osteoblast stimulation by sera from paraplegic patients with heterotopic ossification. Paraplegia 30: 165-168.
- Rossier AB, Bussat P, Infante F, Zender R, Courvoisier B, et al. (1973) Current facts of para-osteo-arthropathy (POA). Paraplegia 11: 38-78.
- Chantraine A, Minaire P (1981) Para-osteo-arthropathies. A new theory and mode of treatment. Scand J Rehabil Med 13: 31-37.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi