Research Article, Vector Biol J Vol: 6 Issue: 1
Impact of intestinal parasite/malaria co-infection on haemoglobin in patients of Melong and Denzo health facilities, Littoral region,Cameroon
Ebanga Echi Joan Eyong*, Makebe Sylvie, Gangue Tiburce, Yana Wenceslas
Department of Biological Sciences, University of Bamenda, Bambili, North West Region, Cameroon
*Corresponding Author:Ebanga Echi Joan Eyong, Department of Biological Sciences, University of Bamenda, Bambili, North West Region, Cameroon, Tel: (+237) 677 67 07 24; E-mail: joan.ebangaechi@gmail.com
Received: September 21, 2020; Accepted: October 5, 2020; Published: January 15, 2021
Citation: Eyong et al. (2020) Impact of intestinal parasite/ malaria co-infection on haemoglobin in patients of Melong and Denzo health facilities, Littoral region, Cameroon. Vector Biol J 5:5.
Abstract
Objective: To assess the impact of intestinal parasite/malaria coinfection on haemoglobin in patients of Melong and Denzo health facilities, Littoral region, Cameroon.
Materials and methods: This study took place from November2019-March 2020. Blood samples were collected from patients after informed consent by finger pricking. Stool samples were examined using normal saline and the Kato-Katz technique for the presence and intensity of IPs. Thick blood films were prepared, Giemsa-stained and examined under x100 to detect the presence of parasites and estimate GMPD. Hb values were determined using a haemoglobinometer. Data was analysed using SPSS version 23 and the significance level was set at P<0.05.
Results: The overall prevalence of IP was 28.3% (113/400).Entamoeba histolytica was the most prevalent IP 22.0% (88/400) while Taenia spp 0.3% (1/400) and Trichuris trichiura 0.3% (1/400) recorded the lowest prevalences. E. histolytica was significantly more in Melong (27.7%, 76/274) than in Denzo (9.5%, 12/126), (P=0.001). Ascaris lumbricoides was significantly more in Denzo (10.3%, 13/126) than in Melong (0.3%, 1/274), P=0.001. Trichomonas hominis was the only parasite which was significantly different (p=0.009) between age groups. The overall prevalence of malaria was 66.5% (266/400). The prevalence of malaria was higher in Denzo (79.3%, 100/126) than in Melong (60.5, 166/274), P=0.001. Children ≤ 5 years recorded the highest (75.4%, 83/110) prevalence of malaria, and the difference between age groups was significant, p=0.016. The overall prevalence of co-infection and anaemia were 16.3% (65/400) and 58.8% (235/400), respectively. Higher prevalence (20.6%, 37/180) of intestinal parasites/malaria was seen in anaemic patients than in non-anemic (12.7%, 28/220) p=0.035.
Conclusion: Malaria was a strong predictor of anemia and the malaria intensity was highly correlated with anemia in patients from Melong and Denzo localities. Interventions targeting groups at risk will help reduce morbidity and mortality caused by these diseases in Melong and Denzo localities.
Keywords: Malaria; Intestinal parasites; Co-Infection; Anemia;Melong; Denzo; Littoral Region, Cameroon
Keywords: Malaria; Intestinal parasites; Co-Infection; Anemia; Melong; Denzo; Littoral Region, Cameroon
Background
An intestinal parasitic infection is a condition in which a parasite infects the gastrointestinal tract of humans and animals. Intestinal parasitic infections comprise both helminthes and protozoans which form the most common infections worldwide [1]. According to the London School of Hygiene and Tropical Medicine [2], the most frequent helminths species are Ascaris lumbricoides, Enterobius vermicularis, Hymenolepis spp, Trichuris trichiura, Strongyloides stercolaris, Schistosoma mansoni, Taenia spp and Hookworm. While most frequent protozoans areEntamoeba histolyticaand Giardia intestinalis. These parasites modify gastrointestinal conditions and produce a variety of symptoms in infected persons such as, inflammation of the small and large intestine, diarrhoea/dysentery, abdominal pain and nausea/vomiting [3]. It has also been estimated that about 3.5 billion people in the world are infected with intestinal parasites of which 450 million are ill [4,5]. Malaria is endemic in all the 10 Regions of Cameroon with a percentage prevalence of about 20% [6].
Five species of Plasmodium cause malaria; Plasmodium malariae, P. vivax, P. ovale, P. knowlesi and P. falciparium with the last one being the most virulent accounting for the majority of malaria deaths [7]. Coinfection of malaria and intestinal parasites is common in individuals in developing countries [8] and severe infections can lead to blood loss, tissue damage, spontaneous abortion and death. However, variation in the prevalence of intestinal parasites and malaria can be related to some factors such as, Climate, geographical localization, hygiene as well as a variety of cultural, economic and social variables [9].
Most intestinal parasites cause infection that lead to acute and chronic diarrhoea in healthy individuals and December lead to life threatening illness in patients with immunosuppressive disease like HIV/AIDS. The inhabitants of Melong and Denzo localities are faced with the challenge of the factors that favour the transmission of these parasites which are poor sanitation, poor drainage and poor quality of water. In addition to these factors, Melong is located at a crossroad from Bamenda to other major towns like Nkongssamba, Douala, Buea and Limbe and it is where travelers usually stop to take a break consuming different types of food which might promote propagation of intestinal parasites.
The findings from this study will provide a better understanding of intestinal parasites/malaria co-infection as predictors of anaemia so as to generate baseline data on the parasites as this will add knowledge about malaria transmission and influence policy to improve community health. The aim of this study was to assess the prevalence of intestinal parasites and malaria co-infection as well as to determine its association with anemia in patients of Melong and Denzo, Littoral Region of Cameroon.
Materials and Methods
Description of study site
Melong is a semi-urban area found in the Littoral Region of Cameroon. Located at Latitude 5o 7’18 N; longitude 9o 57’41”E with an of altitude of 760 m a.s.l. It has an average temperature of 19oC and the climate is marked by two seasons, the rainy and dry seasons. It has an estimated population of 102,000 inhabitants [10] and the area is characterized by poor hygienic conditions due to presence of bushes and poor drainage systems. Inhabitants are engaged in various socio-economic activities.
Denzo, also known as New Melong is a rural area, one of the 40 villages found in Melong sub-division. It is divided into two ethnic groups (New Melong A and New Melong B) headed by a chief. It is made up of 5,099 inhabitants [10].
Farming and trading are the main economic activities of the people in these localities.
Ethical considerations
An ethical clearance was obtained from the University of Bamenda review board. Administrative clearances to carry out this study in Melong district hospital and Denzo integrated Health centre were obtained from the Director of the respective medical facilities. Participation in this study was voluntary. Participants had to fill and sign the informed consent form which explained the benefits of the study (that is, those found infected would be treated). Parents/legal guardians had to fill and sign the informed consent form for minors (children below 18 years).
Study design and study population
This study was a cross-sectional examination in which the prevalence of intestinal parasites and malaria were determined. The study population was made of patients of all age groups, both males and females, that presented stool and blood samples for analysis in the Melong District Hospital and Denzo Integrated Health Centre.
Inclusion criteria
Only patients that brought stool samples for analysis and blood for malaria parasite examination in Melong District Hospital and in Denzo Integrated Health Centre and had signed the informed consent form participated in the study.
Exclusion criteria
Patients who did not present stool samples for analysis and blood for malaria parasite examination in Melong District Hospital and Denzo integrated Health Centre were excluded. Patients who did not bring the required quantity of stool sample and those who did not sign the informed consent form were excluded. Those who signed the informed consent form but wanted to withdraw were not forced to participate in this study.
Sample size estimation
The sample size of this study was calculated based on a similar prevalence study by Williams et al. [11] and the Cochran formula [12], were used. The formulation is:
n=Z2pq/e2
Where Z=standard number deviate (1.96 for a 95% confidence value).
n=desired sample size
P=prevalence of intestinal protozoan 42.9% [11].
q=1-p (proportion in the population that does not have the characteristics being measured).
e=desired level of precision 0.05.
n=(1.96)2(0.429)(0.571)/(0.05)2
n=376 participants.
It was calculated that a minimum sample size of 376 participants was required. A total of 400 participants were sampled to minimize bias.
Stool collection and examination
Patients were given clean, dry and air tight bottles labeled with their initials. They were given instructions on how to collect the required stool sample. A macroscopic examination was done to determine the presence of adult worms in the stool, consistency, and the colour. Direct microscopy examination was done using normal saline. The slides were observed under x10 objective and x40 objective lens of the microscope to detect trophozoite and cyst forms especially the motile forms. The Kato-katz concentration technique was used following the Tadesse et al. [13] and WHO [14] methods to determine the presence and intensity of helminth eggs.
Blood collection, preparation and staining of blood smears
Prior to blood sample collection demographic information such as the age, sex, area of residence were recorded. Using sterile disposable lancets, finger pricks were performed. Thick and thin blood films were prepared using the method described by Cheesbrough [15]. The code number of each individual was written on the slide and the blood films were allowed to air dry protected from dust and flies. In the laboratory, the thin films were fixed with 100% methanol for one minute and both thick and thin blood films were stained with 5% Giemsa stain solution for 30 minutes [15].
Detection and estimation of parasitaemia of Plasmodium species
The slides were read under x100 (oil immersion) objective of the microscope for the detection of malaria parasites by an experienced microscopist. A second experienced microscopist, blinded to the first reading, read all thick smears and any discrepancies (positive vs. negative; results that did not match each other; >25% difference in parasite density) were resolved by a third microscopist. Parasite densities were determined from thick blood smears by counting the number of asexual parasites or sexual parasites per 200 WBCs and converted to number of parasites/μ l blood assuming a standard WBC count of 8,000/μ l. A smear was considered negative if no parasites were seen after a review of 100 high-powered fields.
Haemoglobin concentration
Haemoglobin concentration was detected by putting a drop of blood on the mission digital Hb haemoglobin testing machine. The results were recorded after 15 seconds according to methods described by Crawley [16]. Anemia was defined as Hb<11.0 g/dL [17].
Data Analysis
Data collected were recorded in the Microsoft excel. The data was analysed using the Statistical package for social sciences (SPSS) version 23. Proportions were calculated to obtain the prevalences of infection. Chi Square contigency test was used to test for significant differences in proportions. Binary logistic Regression was used to assess the association between intestinal parasites and malaria-intestinal parasites co-infection and anemia. The Pearson’s correlation coefficient (r) was calculated to determine if anemia is linked with co-infection malaria and intestinal infections. The Mann-Whitney test was to check for significant differences in the geometric mean parasite density (GMPD) between localities and also between males and females. The Kruskal-Wallis test was used to test for significant differences in GMPD between age groups. All the tests were performed at the 5% significance level.
Results
Demographic characteristics of the study population
A total of 400 persons were enrolled into the study. In Melong, 274(68.8%) were sampled while 126(31.5%) were sampled in Denzo, (Table 1). More females (248, 62%) were enrolled into the study than men (152, 38%), (Table 1). The highest number of participants 110(27.5%) belonged to the ≤ 5 years age group while the lowest number 48, 12% was in the age group ≥ 51 years, (Table 1).
Table 1: Demographic characteristics of the study population
Prevalence of intestinal parasites in the study
The overall prevalence of intestinal parasites was 28.3% (113). Out of the 113 patients infected with intestinal parasites, 31.8% (87/113) were from Melong and 20.6% (26/113) from Denzo. E. histolytica had a prevalence of 27.7% (76/274) in Melong and Denzo 9.5% (12/126) and the difference in the prevalence of E. histolytica between the 2 localities was highly significant (χ2=16.68, P<0.001), (Table 2). The prevalence of Ascaris lumbricoides was higher in Denzo 10.3% (13/126) than in Melong 0.3% (1/274) and the difference was highly significant (χ2=25.31, P<0.001), (Table 2). The prevalence of the other intestinal parasites observed can be seen in (Table 2).
Table 2: Prevalence of intestinal parasites in the study
With respect to sex, the overall prevalence of intestinal parasites in males was 24.3% (37/152) and females 30.6% (76/248). Females were more infected with E. histolytica than males although the difference was not significant (χ2=0.13, P=0.720), (Table 2). Trichomonas hominis was found only in females 2.4% (6/248) with no significant difference (χ2=3.73, P=0.05). Females were more infected with Ascaris lumbricoides 3.6% (9/248) than males 3.2% (5/152) but the difference was not statistically significant (χ2=0.32, P=0.858). T. hominis, Giardia lamblia, Taenia spp and Trichuris trichiura were not found in males (0%), while females had varied prevalence; T. hominis 2.4% (6/248), G. lamblia 1.2% (3/248), Taenia spp 0.4% (1/248) and T. trichiura 0.4%(1/248) the difference was not significant (χ2=3.73, P=0.053; χ2=1.85, P=0.173; χ2=4.27, P=0.370; χ2=0.61, P=0.433), respectively in Table 2.
The overall prevalence of intestinal parasites was highest 35%, (21/60) in adults aged 31-50 years and the lowest 20.9% (23/110) in participants aged ≥ 51 years. The prevalence of E. histolytica was highest in adults 16-30 years 27.4% (29/106) and the lowest in children ≤ 5 years 14.5% (16/110) although the difference was not significant (χ2=5.72, P=0.221). The prevalence of A. lumbricoides amongst the different age group highest in children ≤ 5 years 4.5% (5/110) and lowest in patients ≥ 51 years 2.0% (1/48). There was no significant difference (χ2=3.63, P=0.458). Trichomonas hominis which was least in age group ≤ 5 years (0%) and ≥ 51 years (0%) while most of the parasites was seen in 31-50 years patients (6.6%, 4/60) and the difference was statistically highly significant (χ2=13.49, P=0.009), (Table 2). Giardia lamblia, Taenia spp, T. trichiura had no significant difference in the prevalence amongst the various age groups (P>0.05), (Table 2).
Intensity of intestinal parasites in the study
Participants in Melong recorded a higher parasite load (range) 38(24- 384) than those in Denzo 38(24-96) although the difference was not significant (Mann Whitney U Test, P=0.466), (Table 3). In relation to sex, females, had a higher parasite load (range) 39(24-384) than males 36(24-144) but the difference was not significant (Mann Whitney U Test, P=0.541), (Table 3). With respect to age, the highest parasite load (range) was recorded in patients aged 16-30 years 41(24-384) and the least in patients 31-50 years 34(24-96) and ≥ 51 years 34(24-96) and the difference was significant (Kruskal Wallis Test, P=0.041), (Table 3).
(Range)Level of SignificanceSiteMelong7938(24-384)Mann Whitney
UTest, P=0.466Denzo3038(24-96)SexMale3936(24-144) Mann Whitney
U Test, P=0.541Female7039(24-384)Age groups
(Yrs) ≤52347(24-144) Kruskal wallis
Test, P= 0.0416-152138(24-120)16-303341(24-384)31-501834(24-96)≥511426(24-96)Mean EPG±SEM(range) Total 109 48±44 (24-48)
EPG= Egg per gram, CPG= cyst per gram, SEM=standard error of mean
Table 3: Intensity of intestinal parasites in the study
Prevalence and intensity of malaria in the study
The overall prevalence of malaria was 66.5% (266). With respect to localities, Denzo recorded a higher prevalence 79.3% (100/126) of malaria than Melong 60.5% (166/274) and the difference was highly significant (χ2=13.666 P=0.001), (Table 4). The prevalence of malaria was higher in males 72.3% (110/152) than in females 60.5% (166/248), although the difference was not statistically significant (χ2=3.790, P=0.052), (Table 4). The highest prevalence of malaria, 75.4% (83/110) was recorded in the age group ≤ 5 years while the lowest, 56.6% (34/60) was recorded in patients aged 31-50 years and the difference was significant (χ2=12.249, P=0.016), (Table 4).
p-value> GMPD
[trophozoites/µl ]
(range)>P-value>Site>Melong>274>166(60.5)>χ2=13.67
P<0.001>762(160-200,000)>Mann-Whitney U Test,
P<* 0.001>Denzo>126>100(79.3)>444(40-10,000)>Sex>Male152110(72.3)>χ2=3.79
P= 0.052>620(40-8,000)>Mann-Whitney U test, p=0.477> Female>248>156(62.9)>624(40-200,000)>Age groups
(years)≤511083(75.4)χ2=12.25
P= 0.016>645(40-200,000)>Kruskal - wallis Test, P=0.1616-157657(75.0)>827(120-8,000)16-3010664(60.3)>578(40-40,000)> 31-506034(56.6)> >557(80-4,000)> ≥514828(58.3)>425(40-1,600)>Total 400266(66.5)> > >
GMPD = Geometric mean parasite density, n= Number positive, N= Number examined, SD= standard deviation
Table 4: Prevalence and intensity of malaria in the study
Participants in Melong recorded a higher GMPD, 762 (160-200,000 trophozoites/ μ l of blood) than those in Denzo, 444 (40-10,000 trophozoites/ μ l of blood) and the difference was highly significant p<0.001, (Table 4) Females had a higher 624(40-200,000 trophozoites/ μ l) GMPD than males 620(40-8,000 trophozoites/ μ l), although the difference was not significant (P=0.477), (Table 4). Based on age, the highest GMPD range was found in children ≤ 5 years old 645(40- 200,000 trophozoites/ μ l of blood) and the lowest in adults ≥ 51 years old 425(40-1,600 parasites/ μ l of blood), although there was no significant difference (p=0.161), (Table 4).
Haemoglobin (Hb) profile in the study population
The mean Hb in the study population was 11.38 ± 1.86 (range: 4.8- 17.7 g/dL). A total of 165 (41.3%) participants recorded normal Hb values while 235 (58.8%) were anaemic. Of those anaemic, 12(3.0%) suffered from severe anaemia (<7 g/dL), 142(35.5%) from moderate anaemia (7.0-9.9 g/dL) and 81(20.3%) from mild anaemia (10.0-10.9 g/dL). More persons were anemic in Denzo 53.2% (67/126) than in Melong 41.2% (113/274) and the difference was statistically significant (χ2=4.97, P=0.026), (Table 5). Males recorded a higher prevalence of anaemia 45.4% (69/152) than females 44.8% (111/248) with no significant difference (χ2=0.02, P=0.901), (Table 5). Children ≤ 5 years old were more anaemic 58.2% (64/110) while the least anemic cases were adults 31-50 years old 26.7% (16/60). Prevalence of anemia according to age range had a highly significant difference (χ2=18.32, P=0.001), (Table 5).
Table 5: Prevalence of anaemia in the study population
Prevalence of co-infection Malaria-intestinal parasites
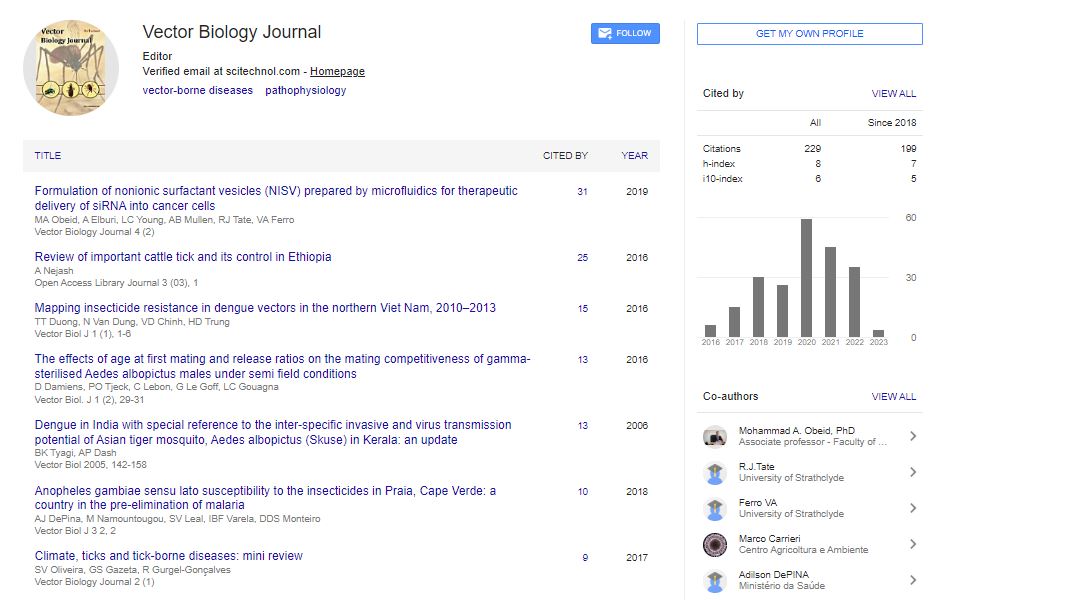
The overall prevalence of malaria-intestinal parasite coinfection was 16.3(65). Out of the 6 intestinal parasites seen in the study population, four species were co-infected with malaria (E. histolytica, A. lumbricoides, G. lamblia and T. hominis). The prevalence of E. histolytica malaria co-infection 12.3% (49/400) was the highest and the lowest was G. lamblia-malaria co-infection 0.3% (1/400), (Figure 1).

Figure 1: Co-infection of malaria and intestinal parasites (M.P= malaria parasite)
There was no significant difference in the prevalence of co-infection according to site, sex and age, but according to anemic status, anemic patients had a higher prevalence 20.6% (37/180) than those nonanemic patient 12.7% (28/220) and the difference was significant difference (χ2=4.46, P=0.035), (Table 6).
Table 6: Prevalence of co-infection of malaria/intestinal parasite with respect to site, sex, age and anaemic status
Association of malaria parasite/intestinal parasites/co-infection with anemia
The prevalence of anemia in malaria positive patients was higher 49.2% (131/226) than in malaria negative patients 36.6% (49/134). The risk of being anemic was reduced in malaria negative patients when compared to malaria positive patients with an odds ratio OR=0.6(0.39-0.91). The association between malaria and anemia was statistically significant, p=0.017. There was no significant association of intestinal parasite and co-infection intestinal parasite with anemia as shown in (Table 7).
OR(CI)>P-value>Mp status >Positive>266>131(49.2)>Reference>0.017>negative>134>49(36.6)>0.6(0.39-0.91)>E. h>Positive>88>41(46.6)>Reference>0.734>Negative>312>139(44.6)>0.9(0.57-1.48)>A. l>Positive >14>8(57.1)>Reference>0.357>negative>386>172(44.6)>0.6(0.21-1.77)>T. h>Positive>6>4(66.7)>Reference>0.298>negative>394>176(44.7)>0.4(0.07-2.23)>G. l>Positive>3>2(66.7)>Reference>0.454>negative>397>178(44.8)>0.4(0.04-4.52)>Taenia spp>Positive >1>0(0.0)>->->negative>399>180(45.1)>->T. t>Positive>1>1(100)>->->negative>399>179(44.9)>->M.P/E. h>Positive >49>28(57.1)>Reference>0.071>negative>351>162(43.3)>0.6(0.31-1.05)>M.P/ A. l>Positive >10>6(60.0)>Reference>0.341>negative>390>174(44.6)>0.5(0.15-1.93)>MP/T. h>Positive >4>2(50.0)>Reference>0.840>negative>396>178(44.9)>0.8(0.11-5.86)>MP/G. l>Positive >1>1(100)>->->negative>399>179(44.9%)>->CI=Confidence level, OR=odds ratio, Mp = malaria parasite, E. h =Entamoeba histolytica, A. l =Ascaris lumbricoides, T. h =Trichomonas hominis, G. l = Giardia lamblia, T. t = Trichuris trichiura,>
Table 7: The association of malaria parasite, intestinal parasites and co-infection with anaemia
Discussion
Our study sought to determine the prevalence and impact of coinfection between intestinal parasites, malaria with anemia in people from Melong and Denzo localities. Our findings are explained below.
The overall prevalence of intestinal parasites was 28.8% and it varied with the location. This was lower compared to what was reported by Fusi-Ngwa et al. [18] in Dschang, a locality of West region of Cameroon where the prevalence of intestinal parasites was 34.7% and Omar et al. [19] who recorded intestinal parasites prevalence of 45.38% in Northwestern Saudi Arabia. The prevalence of intestinal parasites was higher in Melong, the semi-urban area than in Denzo, rural area. Although these infections are usually associated with poor sanitary habits, lack of access to safe water and improper hygiene which is more prominent in rural areas. Melong is at a cross road to most major towns where travelers usually stop to take a bite and consume different types of food which can encourage the propagation of intestinal parasites in this area than in Denzo, which is far off. This was in contrast to a study carried out by Kimbi et al. [20] with higher prevalence in rural area than in urban area due to urbanization.
Entamoeba histolytica had the highest prevalence amongst the intestinal parasites, with the prevalence of Entamoeba histolytica in Melong being significantly higher than that in Denzo (P<0.001). Entamoeba histolytica is an indicator organism of faecal contaminated food or water and it is mostly present in unhygienically prepared food which leads to the outbreak of amoebiasis. The higher prevalence in Melong might be because of the high level of consumption of fish and meat along the road, which is likely to be undercooked or contaminated with faecal matter or the consumption of contaminated water. Also, semi-urban markets might sell contaminated vegetables which are sometimes eaten raw, undercooked to retain taste and preserve heatlabile nutrients. It could also be due to the presence of resistant cysts in Melong. Ascaris lumbricoides was significantly higher in Denzo than in Melong P<0.001. This difference might be because; Ascaris lumbricoides is a soil-transmitted helminth and can be acquired by ingesting its eggs in contaminated food or rarely water. Most of the people of Denzo are farmers and this might have increased their chances of ingesting the egg directly from soil via dirty hands. This was similar to what was observed by Kimbi et al. [20] in the Mount Cameroon region, with higher prevalence of A. lumbricoides due to lower level of sanitation in the rural areas. Entamoeba histolytica was highest in adults aged 16-30 years although the difference was not significant (P=0.221). This could be because, this age group 16-30 years are the most active working group, some could be food handlers who do not take hand washing seriously, their level of education especially on knowledge of transmission of amoebiasis is low and they are most likely to keep long finger nails which will serve as a transmission medium. The findings of this study were in contrast with that observed by Zaglool et al. [21] where children less than five years of age had the highest prevalence of E. histolytica due to poor hand hygiene in both children and caregivers and lack of portable water supply. It was higher compared to studies done by Banke et al. [22], Akingbade et al. [23] Ismail, [24] who recorded 7.06%, 19.4% and 2%, respectively.
Trichomonas hominis was higher in adult age 31-50 years and least in children ≤ 5 years and ≤ 51 years and the difference was significant (P=0.009). This is a zoonotic infection that can be transmitted through the faeco-oral route or from formites and adults are more exposed as they play with animals than children. Also, adults are engaged with farm activity more which exposes them to fecal matter. This is in contrast with an experiment carried out by Inoue et al. [25] on marmosets where the infection of Trichomonas hominis was not due to age or sex.
According to the results of this survey, it was noticed that people of Melong and Denzo localities of Cameroon are more infected by malaria than intestinal parasites. This can be explained by the failure to prevent malaria infection in the two localities. The overall prevalence of malaria was 66.5% which was higher than that reported by Nkuo- Akenji et al. [26] in Mount Cameroon region and Oboth et al. [27] in Mid-Western Uganda, which was 64% and 55.04%, respectively. This indicates that the prevalence of malaria in Cameroon is still high despite the intermittent prevention and control measures put in place. Our study reveals that the prevalence of malaria was higher in Denzo (rural area) than in Melong (semi-urban) and the difference was highly significant (P<0.001). The higher prevalence in the rural area could be due to greater risk of vector contact and infection as a result of no bed nets, most of them lack screens on doors and windows of their houses, poor living conditions, stagnant water and bushes around the house. Also, the high prevalence could be due to insufficient knowledge and practice of good behaviour towards malaria prevention and control measures. These results are similar to study carried out by Kimbi et al. [20] and M’bondoukwe et al. [28] who also noticed that rural areas have a higher prevalence than semi-urban and urban areas because their houses were made of plank with crevices on the walls.
This study revealed that that the prevalence of malaria in males was higher than in females, although the difference was not significant (P=0.052). This could probably be because males are more exposed to the malaria vector than females as they work in the fields at peak biting time or move to malarious areas for work. This finding was similar to that in studies carried out by Das et al. [29] and Yusof et al. [30] who also noticed higher prevalence of malaria in males than females due to the nature of their jobs as they are mainly into agriculture such as farming, forestry workers and loggers, who have higher risk of exposure to the Anopheles mosquitoes.
The prevalence of malaria varied significantly (P=0.016) with age with children aged ≤ 5 years having the highest prevalence. This might be because young children are more vulnerable to malaria parasite infection as they have gotten little or no partial immunity to the parasite. The severity of the attack of Plasmodium spp depends on circumstances such as the state of immunity and the general health and nutritional status of the infected individuals. Older patients have probably had several attacks of malaria which help them develop acquired immunity that can protect them from severe attacks or death [31]. Although no one develops complete immunity against malaria that can fully protect the person from infection.
The overall prevalence of co-infection was 16.3%. The prevalence of co-infection in Denzo was higher than Melong; the risk factors associated to single infection might have been the same reason for coinfection. This was in contrast with what was reported by Shapiro et al. [32] in a study conducted in Uganda which showed no association of malaria with intestinal parasites. This was probably because in areas of frequent exposure to malaria, immunity is developed and so the effect of helminthes co-infection was minimal when transmission intensity is low. Also, the disparity might have been due to the genetic makeup of individuals, which December confound the nature of relationship between malaria parasite and intestinal parasites [33].
The prevalence of co-infection in those anemic was higher than in those non-anemic and the difference was significant (P=0.035). Coinfection lead to malabsorption of nutrients which are required for hematopoiesis, meaning if there is lack of nutrients caused by coinfection, the process of haematopoiesis will be affected leading to decreased haemoglobin production resulting in anemia. This probably means that co-infection increase the anaemic level of the individual, this might not be directly due to intestinal/malaria co-infection but other confounding factors like immunosuppression, malnourishment or other viral, bacterial, parasitic or chronic infection. Some of the factors that support co-infection could be humidity, bushes and poor sanitary disposal.
This study revealed that, malaria parasite is a strong predictor of anaemia, where the prevalence of anemia in malaria positive patients was higher than in malaria negative patients and the difference was significant, p=0.017. Based on the odds ratio (OR=0.6), it indicates that those who did not have malaria were less likely to be anemic. This could be because fever in malaria usually leads to the rupture of erythrocytes. There is evidence that Ascaris lumbricoides associated vitamin a defficiency December further increase risk of anemia in those co-infected with malaria [34]. This was not the case in this study were there was no association of Ascaris lumbricoides/malaria with anemia. There was no statistical relationship of co-infection malaria and intestinal parasites with anaemia (P>0.05) which was in contrast with studies done in Rwanda, Kenya and Uganda [35-37]. This might be because most of the intestinal parasites that are known to cause high risk of anaemia such as hookworms, Schistosoma species were not found in the study population.
Conclusion
The overall prevalence of intestinal parasites in Melong was 31.7% and in Denzo 20.6% and the overall prevalence of malaria in Melong was 60.5% and Denzo was 79.3%. This study showed that the prevalence of co-infection of malaria-Entamoeba histolytica was the highest coinfection in the study area and the overall prevalence of co-infection malaria-intestinal parasites was 16.3%. Intestinal parasites and coinfection malaria-intestinal parasite had no impact on anaemia but malaria had an impact.
The Ministry of Public Health should therefore consider the redistribution of insecticide treated bed nets and sensitised the people on the importance of using the bed nets which will help reduce the risk of malaria as most of the people complained of no bed nets. There is a need of the Ministry of Public Health to institute some control measures such as intermittent preventive treatment of malaria and intestinal parasites in Melong and Denzo, Cameroon.
Authors’ Contributions
EEJE and YW conceived and designed the study; MSW collected data and took part in data analysis. GT analysed the data. All authors wrote the manuscript. EEJE and YW supervised, reviewed and provided inputs to the manuscript.
All the authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank the parents/legal guardians who willingly consented to their children participating in this study. Many thanks go to the hospital staff where blood samples were collected for maximum cooperation.
Funding was partly from the researchers’ individual salaries and partly from the Allowances for Research Modernization from the Ministry of Higher Education in Cameroon.
Competing Interests
The authors declare that they have no competing interests.
References
- Quattara M, Nguessan N, Yapi A, N’goran E (2010) Prevalence and spatial distribution of Entamoeba histolytica /dispar and Giardia lamblia among school children in Agboville area (cote d’ivoire). Plos Neglected Tropical Disease 4(1):574.
- London School of Hygiene and Tropical Medicine. Global atlas of helminth infections.
- World Health Organization. (2017). Intestinal worms.
- Brooker S, Kabatereine N, Smith J, Mulpfasoni D, Mwanje M, Ndayishimiye O (2009) An updated atlas of human helminths infections, the example of East Africa. International Journal of Health Geographics 8: 42.
- Keisser J, Utzinger J (2010) The drugs we have and the drug we need against helminths infections. Advanced Parasitology 73:197-230.
- Mangham LJ, Bonnie C, Achonduh OA, Ambebila A, Lele AK, Metoh TN, Ndive SN, Ndong IC, Nguela RL, Nji AM, Orang B, Wiseman V, Pamen-Ngako J, Mbacham W (2012) Malaria prevalence and treatment of febrile patients at health facilities and medicine retailer in Cameroon. Tropical Medicine and International Health 17(3):330-342.
- Olupot OP, Maltland K (2013) Result from recent trials. Advance in Experimental Medicine and Biology 764: 241-250.
- Steinmann P, Utzinger J, Duz W, and Zhou XN (2010) Multiparasitism. A neglected reality on global, regional and local scale. Advanced Parasitology 73: 21-50.
- Nematian J, Gholamrezanezhad A, Nematian E (2008) Giardiasis and other intestinal parasitic infections in relation to anthropometric indicators of malnutrition a large, population- based survey of school children in Tehran. Annual of Tropical Medicine and Parasitology 102 (2):209-214.
- Hugor EE (2016) Project to set up a tourist office in the town of Melong.
- William W, Samuel CK, Philip T, Juventus BZ (2014) Prevalence of intestinal protozoan infestation among primary school children in urban and peri-urban communities in Kumasi, Ghana. Science Journal of Public Health 2(2):52-57.
- Cochran WG (1963). Sampling techniques 2nd edition. New York: John Wiley and sons, Inc.
- Tadesse A, Araya G, Abraham A, Arega A, Alemayehu W, Negessse D, Dawit Y, Moges D (2008) Intestinal parasitosis for the Ethiopian health centre team 126:85-87.
- World Health Organization. (1991). Basic laboratory methods in Parasitology. p. 25-28
- Cheesbrough M (2000) District Laboratory Practice in Tropical Countries. Part 1. Cambridge low price editions, Cambridge University Press, London. 454 p.
- Crawley J (2004) Reducing the burden of anemia in infants and young children in malaria-endemic countries of Africa: from evidence to action p.25.
- World Health Organization.(1967). Nutritional anemia’s. Report of WHO scientific group, Geneva.
- Fusi-Ngwa C, Besong E, Pone JW, Mbida M (2014) A cross–sectional study of intestinal parasitic infections in children in Ghettoed, diverse and affluent, communities in Dschang, West Region Cameroon. Open Access Library Journal, 01: 1-14.
- Omar HM, Ibraheem M, Najoua Al (2015) Prevalence of intestinal parasite infections among patients in local public hospitals of hail Northwestern Saudi Arabia. Asian Pacific Journal of Tropical Medicine 9: 44-48.
- Kimbi HK, Lum E, Wanji S, Mbuh JV, Ndamukong-Nyanga J, Ebanga EJ, Joanne L (2012) Co-infection of Asymptomatic malaria and soil- transmitted helminths in school children in localities with different levels of urbanization in the mount Cameroon Region. Journal of Bacteriology and Parasitology 3: 134.
- Zaglool DA, Khodari YA, Gazzaz ZSM, Dhafar KO, Shaker HA, Farooq MU (2011) Prevalence of intestinal parasites among patients of Al-Noor specialist Hospital, Makkah, Saudi Arabia. Oman Medical Journal 26: 182-185.
- Banke R, Omudu EA, ikenwa DA, Feese IJ (2006) Prevalence of gastrointestinal parasites in five communities south-west Nigeria. Animal Rresearch International 3: 489-493.
- Akingbade OA, Akinjinmi AA, Ezechukwu US, Okenrentugba PO, Okonko IO (2013) Prevalence of intestinal parasites among children with diarrhoea in Abeokuta, ogun states, Nigeria researcher. World Rural Observation 5: 66-73
- Ismail KA (2018) Prevalence of intestinal parasitic infection among school children in Taif. Insight Biomedicine 3(2):10.
- Inoue T, Hayashimoto N, Yasuda M, Sasaki E, Itoh T (2015) PentaTrichomonas hominis in laboratory-bred common marmosets. Experimental Animals 64(4):363-368.
- Nkuo-Akenji TK, Chi PC, Cho JF, Ndamukong KK, Sumbelele I (2006) Malaria and helminths co-infection in children living in malaria endemic setting of mount Cameroon and Predictors of anemia. Journal Parasitology, 92(6):1191-1195.
- Oboth P, Yahaya G, Banson JB (2019) Prevalence and clinical outcomes of Plasmodium falciparium and intestinal parasitic infection among children in Kiryandongo refugee camp, mid-western Uganda. Journal BMC Infectious Disease 19(1):295
- M’bondoukwe NP, Kendjo E, Mawili-mbounba DP, Koumba LJ, Offouga MC, Nkoghe D, Fousseyni T, Bouyou-Akotet M (2018) Prevalence and risk of malaria, filariasis and intestinal parasites as single infections or co-infctions in different settlements of Gabon, Central Africaa. Infectious Disease of Poverty 7(1):6
- Das NG, Talukdar PK, Kalita J, Baruah I, Sribastava RB (2007) Malaria situation in forest fringed villages of sonitpur district (Assam). India borderin`g Arunachal Pradesh during an outbreak. Journal of Vector Borne Diseases, 44(3):213-218
- Yusof R, Lau YL, Mahmud R, Fong MY, Jelip JM, Ngian HU, Sahlawati M, Hussin HM, Marzuki N, Mohd MA (2014) High proportion of knowlesi malaria in recent malaria cases in Malaysia. Malaria Journal 13:168
- Quakyi IA, Leke RG, Befidi-Mengue R, Tsafack M, Bomba- Nkolo D, Tchinda V, et al. (2000) The epidemiology of Plasmodium falciparum malaria in two Cameroonian villages. Sombok and Etoa. American Journal of Tropical Medicine and Hygiene, 68(3):222-230.
- Shapiro AE, Erdridah MT, Kasten J, Sian EC, Magnussen P, Oslen A, Narcus BK, Ndyomugyenji R, Brooker S (2005) Epidemiology of helminth infections and their relationship to clinical malaria in Southwest Uganda. Transactions of the Royal Society of Tropical Medicine and Hygiene 99(1):18-24.
- Abraham D, Berhanu E (2016). Epidemiology of Plasmodium and Helminth co-infection and possible reasons for heterogeneity. Journal of Biomedicine and
- Pullan R, Brooker S (2008) The health impact of polyparasitism in humans; are we under-estimating the burden of parasitic diseases? Parasitology, 135(7):783-794.
- Marcelline U, Noella U, Tharcise M, Joshephat M, Banson JB Karema C (2016) The impact of malaria and gastrointestinal helminthiasis co-infection on anemia and severe malaria among children in bugesera. District, Rwanda. International Journal of Tropical Disease and Health. 13(4):1-7
- Brooker S, Peshu N, Warn PA, Mosobo M, Guyatt HL, Marsh K, Snow RW (1999) The epidemiology of hookworm infection and its contribution to anemia among pre-school children on the Kenyan coast. Transactions of Royal Society of Tropical Medicine and Hygiene 93(2):240-246.
- Standley CL, Adriko M, Alinaitive M, Kazibwe F, Kabatereine NB, and Stothard JR (2009) Intestinal Schistosomiasis and soil transmitted helminthiasis in Ugandan School children: rapid mapping assessment. Geospatial Health 4(1):39-53
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi