Case Report, Clin Dermatol Res J Vol: 3 Issue: 1
Long-Term Antibiotic Treatment with Minocycline and Sulfamethoxazole-Trimethoprim in Acne Keloidalis Nuchae Associated with Crohn’s Disease Development: A Case Report
1University of North Texas Health Science Center, Fort Worth, Texas, USA
2Independent Researcher, Houston, Texas, USA
*Corresponding Author : Daniel A. Nguyen
University of North Texas Health Science Center, Fort Worth, Texas, 76107, USA
Tel: 832-692-3263
E-mail: daniel.nguyen@my.unthsc.edu
Received: January 17, 2018 Accepted: February 23, 2018 Published: February 27, 2018
Citation: Nguyen DA, Vo CN (2018) Long-Term Antibiotic Treatment with Minocycline and Sulfamethoxazole-Trimethoprim in Acne Keloidalis Nuchae Associated with Crohn’s Disease Development: A Case Report. Clin Dermatol Res J 3:1. doi: 10.4172/2576-1439.1000124
Abstract
Systemic antibiotic treatments for an extended period of time have greater potential for adverse effects. Acne keloidalis nuchae is a chronic disorder characterized by inflammation and scarring. The management approach for acne keloidalis nuchae includes antibiotic regimen durations consisting largely on clinical expertise. This case reports a 27-year-old male who developed bloody diarrhea and diagnosed with Crohn’s disease after more than 9 months of antibiotics, minocycline and sulfamethoxazoletrimethoprim. By writing this up, new evidence is provided for the association between these two specific antibiotics and Crohn’s development, while highlighting the need for cautious attention during acne keloidalis nuchae management. Clinicians should be aware that antibiotics may contribute to the pathogenesis of inflammatory bowel disease and careful consideration should be given to this development in treatment regimens.
Keywords: Sulfamethoxazole; Trimethoprim; Minocycline; Acne keloidalis nuchae; Inflammatory bowel disease; Crohn’s disease; Antibiotics
Abbreviations
AKN: Acne Keloidalis Nuchae;IBD: Inflammatory Bowel Disease;SMX/TMP: Sulfamethoxazole-Trimethoprim
Introduction
Acne keloidalis nuchae (AKN) is a chronic disorder characterized by inflammation and scarring that can lead to significant cosmetic defects [1]. The treatment data is limited with no consensus guidelines, and management approach consisting largely of clinical expertise. This patient was treated with antibiotics for an extended period of time. A potential adverse effect of long-term systemic antibiotics, minocycline and sulfamethoxazole-trimethoprim (SMX/ TMP), may have manifested as an incidence of Crohn’s disease. By writing this up, new evidence is provided for the association between antibiotic use, specifically SMX/TMP, and inflammatory bowel disease (IBD) development while calling for careful attention during AKN management.
Case Synopsis
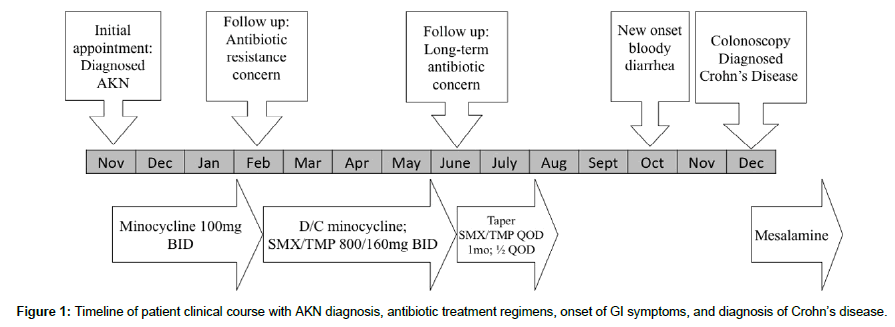
A 27-year-old male presented to a dermatology clinic in an urban United States city for a chief complaint of skin lesions on the scalp described as itchy and irritating. Physical exam findings showed keloidal papules and pustules distributed on the scalp. The patient was diagnosed with AKN and treated with oral minocycline 100 mg capsules taken twice daily with resolution of symptoms (Figure 1). Patient presented for follow up visit three months later with concerns of antibiotic resistance as lesions started to reoccur on the lower occipital scalp. Patient’s minocycline discontinued and oral SMX/ TMP 800mg-160mg tablets twice daily prescribed with subsequent improvement in symptoms. Patient presented for follow up visit four months later with long-term antibiotic use concern. Patient’s lesions were well controlled at the time and antibiotic use was tapered down over the next 2 months. The patient remained off antibiotics with scalp lesions of mild to moderate severity, periodically recurring. Two months after discontinuing antibiotics, patient reported new onset gastrointestinal symptoms as bloody diarrhea. The following months involved workup with a primary care provider and gastroenterologist, leading to a colonoscopy diagnosed Crohn’s disease of the sigmoid and rectum. Patient’s Crohn’s has been disease being controlled with mesalamine.
Case Discussion
Acne keloidalis nuchae treatment approach can include an indeterminate period of long-term systemic antibiotics which could have significant implications, including contribution to inflammatory bowel disease development [2].
Several population studies in the literature have shown an association between tetracycline antibiotics and inflammatory bowel disease. A retrospective cohort study using The Health Improvement Network database of the United Kingdom identified 94,487 individuals with acne, in which given a prescription for minocycline (24,085 individuals), tetracycline/oxytetracycline (38,603 individuals), or doxycycline (15,032 individuals) resulted in hazard ratio for developing IBD with any exposure to a tetracycline antibiotic as 1.39 (1.02, 1.90) [3]. A nested case-control study using the University of Manitoba Inflammatory Bowel Disease Epidemiologic Database identified 2,234 subjects diagnosed with IBD and showed 12% of cases had ≥ 3 prescriptions 2 years before the case date, with an odds ratio for an IBD diagnosis of 1.5 (1.3,1.8; P<0.0001), compared with 7% of controls [4]. Similar associations in pediatric populations diagnosed with IBD had resultant increased odds ratio, if antibiotic use occurred during first year of life (2.9; 1.2, 7.0) or an episode of otitis media occurred (surrogate for antibiotic use) in the first 5 years of life (2.8; 1.5-5.2; P=.001) [5,6]. Bernstein suggests that antibiotics could be a risk factor for the development of inflammatory bowel disease due to the impact on gut microbiome in genetically susceptible individuals [7,8]. Many of the studies have made the IBD association with tetracycline antibiotics, but no study has correlated inflammatory bowel disease with the sulphonamide and dihydrofolate reductase inhibitor combination antibiotic, SMX/TMP.
This case report details a prolonged use of multiple antibiotics due to the uncertain clinical course of AKN. We defined long-term antibiotics as ≥ 6 months. The strength of this report is the continuous period of 9 months antibiotic duration that can more directly attribute minocycline and SMX/TMP use to increased adverse drug events by predisposing patients to drastic impacts on gut microbiome, which could accelerate development of IBD [7]. No direct causal relationship can be drawn from antibiotic use as the pathogenesis of IBD is unclear and likely multifactorial [7]. Limitations revolve around patient demographics (young adult male from well-developed nation) which generally support the development of IBD.
Conclusion
Acne keloidalis nuchae treatment regimens are widely variable and can include an extended course of multiple antibiotics [1]. There are limited studies on the safety of long-term antibiotic use with known short and long-term effects on gut microbiome [8]. Antibiotics have been associated with inflammatory bowel disease and are a risk factor in the pathogenesis of disease [2-7]. Clinicians should be aware that various antibiotics may contribute to the pathogenesis of inflammatory bowel disease and careful consideration should be given to this development in AKN treatment regimens.
References
- Maranda EL, Simmons BJ, Nguyen AH, Lim VM, Keri JE (2016) Treatment of Acne Keloidalis Nuchae: A Systematic Review of the Literature. Derma Therapy 6: 363-378.
- Card T, Logan RF, Rodrigues LC, Wheeler JG (2004) Antibiotic use and the development of Crohn's disease. Gut 53: 246-250.
- Margolis DJ, Fanelli M, Hoffstad O, Lewis JD (2010) Potential association between the oral tetracycline class of antimicrobials used to treat acne and inflammatory bowel disease. American J Gastro 105: 2610-2616.
- Shaw SY, Blanchard JF, Bernstein CN (2011) Association between the use of antibiotics and new diagnoses of Crohn's disease and ulcerative colitis. American J Gastro 106: 2133-2142.
- Shaw SY, Blanchard JF, Bernstein CN (2010) Association between the use of antibiotics in the first year of life and pediatric inflammatory bowel disease. American J Gastro 105: 2687-2692.
- Shaw SY, Blanchard JF, Bernstein CN (2013) Association between early childhood otitis media and pediatric inflammatory bowel disease: an exploratory population-based analysis. J Pediatrics 162: 510-514.
- Bernstein CN (2013) Antibiotic use and the risk of Crohn's disease. Gastro Hepato 9: 393-395.
- Jernberg C, Lofmark S, Edlund C, Jansson JK (2010) Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology 156: 3216-3223.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi