Case Report, J Blood Res Hematol Dis Vol: 7 Issue: 4
Management of neuroendocrine tumour of the appendix in a patient with moderate haemophilia B: a rare coincidence
Beatriz Oliveira Sousa1*, Diogo Carrola Gomes2, Alexandra Santos1, Margarida Antunes1 and Maria Joao Diniz1
1Department of Immunology, Central Lisbon University Hospital Center, Lisbon, Portugal
2Department of Colorectal Surgery, Central Lisbon University Hospital Center, Lisbon, Portugal
*Corresponding Author: Beatriz Oliveira Sousa
Department of Immunology,
Central Lisbon University Hospital Center,
Lisbon,
Portugal,
Tel: +351 962 741 865;
E-mail: beatrizoliveirasousa@outlook.pt
Received date: 10 June, 2022, Manuscript No. JBRHD-22-66317;
Editor assigned date: 13 June, 2022, PreQC No. JBRHD-22-66317 (PQ);
Reviewed date: 27 June, 2022, QC No. JBRHD-22-66317;
Revised date: 29 August, 2022, Manuscript No. JBRHD-22-66317 (R);
Published date: 07 September, 2022, DOI:10.4172/JBRHD.1000156.
Citation: Sousa BO, Gomes DC, Santos A, Antunes M, Maria Diniz J (2022) Management of Neuroendocrine Tumour of the Appendix in a Patient with Moderate Haemophilia B: A Rare Coincidence. J Blood Res Hematol Dis 7:4.
Abstract
Haemophilia B is a rare X linked congenital bleeding disorder characterized by a deficiency in coagulation Factor IX (FIX). Its estimated prevalence is 5 cases per 100.000 male births. In haemophilia, the bleeding events severity usually correlates with the degree of the clotting factor deficiency. Patients with moderate haemophilia (1-5%) endure prolonged bleeding with minor trauma or surgery and occasional spontaneous bleeding. We report the case of a thirty four year old male with moderate haemophilia B (no FIX inhibitors) and acute onset of mild right iliac abdominal pain, persistent for 24 hours and associated with loss of appetite. No history of recent abdominal trauma. No systematic prophylactic therapy. The patient was diagnosed with acute appendicitis and underwent laparoscopic appendectomy. Histopathology revealed an appendix neuroendocrine tumour and the patient was scheduled for robotic assisted laparoscopic right hemicolectomy. During his hospital stay, under cautious haematological controls, he progressed favourably with gradual resolution of the hemoperitoneum and abdominal wall hematoma, haemoglobin rise and decreased need for factor IX replacement therapy.
Keywords: Haemophilia B, Neuroendocrine tumour, Appendix, Surgery Factor replacement therapy
Introduction
Haemophilia B is a rare X linked congenital bleeding disorder characterized by a deficiency in coagulation Factor IX (FIX). Its estimated prevalence is 5 cases per 100.000 male births [1].
In haemophilia, the bleeding events severity usually correlates with the degree of the clotting factor deficiency. Patients with moderate haemophilia (1-5%) endure prolonged bleeding with minor trauma or surgery and occasional spontaneous bleeding.
When surgery is required, must be performed on a comprehensive haemophilia treatment centre. It needs additional planning and early schedule for optimal laboratory and blood bank support. Pre and postoperative assessment should include inhibitor screening. Replacement therapy for at least 3 days for minor and 7-10 days for major procedures is recommended by the world federation of haemophilia.
Case Presentation
We report the case of a thirty four year old male with moderate haemophilia B (no FIX inhibitors) and acute onset of mild right iliac abdominal pain, persistent for 24 hours and associated with loss of appetite. No history of recent abdominal trauma. No systematic prophylactic therapy. On the emergency room, he was febrile (armpit temperature 38.1°C), hypertensive (177/92 mmHg), tachycardia (heart rate of 119/minute), with no signs of respiratory distress (respiratory rate of 15/minute and oxygen saturation of 98% on room air). Conscious (glasgow coma scale 15), oriented in time and space, and collaborative. His abdomen was tender to palpation with rebound tenderness in the right iliac region, but no rigidity.
Blood count showed no anaemia with 14,9 g/dL haemoglobin (normal range 13-17), normal platelet count of 245.000 (normal range 150.000-450.000) and leucocytosis of 16.910 (normal range 4.500-11.000). Normal renal function. Elevated Lactate Dehydrogenase (LDH) of 228 U/L (normal range 125-220) and C reactive protein of 64.9 mg/L (normal range <5). Coagulation times were abnormal: Prothrombin Time (PT) 13.7 seconds (normal range 9,4-12,5) and activated Thromboplastin Time (aPTT) 47.6 seconds (normal range 25,1-36,5). Previous factor IX activity was 4% (normal range 65-150).
The patient was diagnosed with acute appendicitis and underwent laparoscopic appendectomy. He received 5.000 IU (≈80 UI/Kg) of recombinant Factor IX (rFIX) during the induction of anesthesia. The procedure was without complications or significant blood loss, with no need for blood transfusion.
Postsurgical treatment included 5.000 IU rFIX every 12 hours and Intravenous (IV) tranexamic acid, 1.000 mg every 8 hours, during the following 4 days. At that time, he was discharged without any complications.
Five days later, he presented to the emergency room with rectal bleeding over the previous 24 hours. Blood count showed mild anaemia with 12.8 g/dL haemoglobin and factor IX activity was 32%. He was discharged with oral tranexamic acid, 1.000 mg every 8 hours, and returned the same day reporting persistent rectal bleeding and mild hypogastric pain. New blood count showed 1 g/dL decrease in haemoglobin to 11.4 g/dL. He was admitted and initiated 3.000 IU rFIX (≈50 UI/Kg) every 12 hours.
Results and Discussion
Total colonoscopy showed active bleeding from the appendicular orifice. Haemostasis was achieved after the placement of a clip and local injection of adrenaline (1:20.000, 8 mL). No other changes were identified. He was discharged 5 days later with no pain or bleeding.
Histopathology revealed an appendix 9.5 cm long and 1.5 cm maximum diameter, with acute inflammatory signs, abscess, and extensive necrotic areas with haemorrhage. The distal end presented a white and firm nodule measuring 2.2 x 1.5 x 1.3 cm, consisting of a neuroendocrine tumour (well differentiated G1) with infiltration of the mesoappendix (≈1 cm, pT3Nx–AJCC 8th edition) [2]. In addition, there were lymphatic, vascular and perineural invasions present. Synaptophysin was positive and Ki-67<3%. Resection margins were free (R0).
A staging octreotide scan performed on the patient revealed an enhanced radionuclide uptake in the right colon with no increased expression of somatostatin receptors in lymph nodes or other organs and tissues (Figure 1).
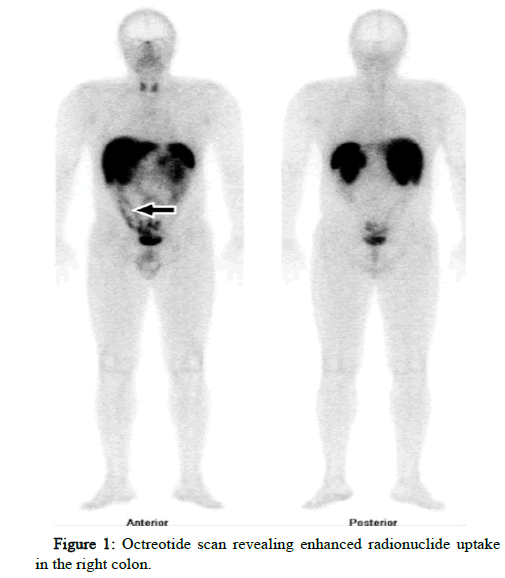
Figure 1: Octreotide scan revealing enhanced radionuclide uptake in the right colon.
Due to the presence of these high risk features, the case was discussed in a multidisciplinary tumour board and offered completion surgery. The patient was scheduled for robotic assisted laparoscopic right hemicolectomy. Pre intervention and before infusion of coagulation factor, the analytical report presented a normal haemoglobin of 15.9 g/dL, normal platelet count of 254.000, normal
PT of 11.8 seconds and prolonged aPTT of 48.9 seconds. Immediately prior to surgery, he received 6.000 IU rFIX (≈100 UI/Kg). Haemostasis was continuously monitored and estimated blood losses were only 100 mL with no need for blood transfusion. No operative complications were reported.
He was admitted to the intensive care unit for continuous monitoring and support. Postsurgical factor replacement therapy consisted in 4.000 IU rFIX (≈65 UI/Kg) every 12 hours. Next day, factor IX trough level was 47% and was infused extra 1.000 IU rFIX. The factor replacement therapy was adjusted to 5.000 IU rFIX (≈80 UI/ Kg) every 12 hours.
On post operative day 2, the patient presented with nausea, bilious vomiting, intestinal colic, abdominal distension and absence of flatus. He was febrile (armpit temperature 38°C), normotensive (119/70 mmHg), normocardic (heart rate of 90/minute), with no signs of respiratory distress (respiratory rate of 22/minute and oxygen saturation of 98% on room air). The volume in the surgical drain was 100 mL in 24 hours. Factor IX activity was 59.2% and the patient received an extra 1.000 IU rFIX. The treatment was newly adjusted to 6.000 IU rFIX (≈100 UI/Kg) every 12 hours and IV tranexamic acid, 500 mg every 8 hours.
CT scan showed dilated loops of small bowel and transverse colon, moderate abdominopelvic hemoperitoneum with rectus sheath hematoma (Figure 2). Blood results of haemoglobin were showing a gradual reduction from 12.1 g/dL until 6,6 g/dL and factor IX activity of 87.5%.
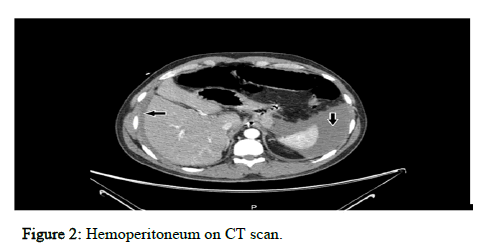
Figure 2: Hemoperitoneum on CT scan.
He was transfused with 2 units of red blood cells and 3 units of plasma.
During his hospital stay, under cautious haematological controls, the patient progressed favourably with gradual resolution of the hemoperitoneum and abdominal wall hematoma, haemoglobin rise and decreased need for factor IX replacement therapy.
Twelve days after surgery, he was discharged home with a scheduled follow up appointment. No further related bleeding episodes are known. No FIX inhibitors developed.
Neuroendocrine tumours are rare neoplasms of the gastrointestinal tract and pancreas [3].
Non functioning tumours are usually asymptomatic in early stages and discovered incidentally (1 in 300 appendectomies). When located in the appendix, even when relatively small they can occlude the appendiceal lumen and cause appendicitis, leading to an early diagnosis.
According to the European neuroendocrine tumour society guidelines 5, all tumours >2 cm, involving the appendiceal base, with positive resection margins after appendectomy or more than 3 mm of mesoappendix extension, should undergo completion right hemicolectomy. For tumours between 1-2 cm on the tip or mid portion of the appendix, right hemicolectomy should be considered if vascular or lymphatic invasion is present and Ki-67 3-20% [4-6].
Conclusion
Lymph node metastases occur infrequently and, when present, all patients reach 10 year survival. Therefore, the prognosis of well differentiated neuroendocrine tumours of the appendix is good.
References
- Srivastava A, Santagostino E, Dougall A, Kitchen S, Sutherland M, et al. (2020) WFH Guidelines for the Management of Hemophilia, 3rd edition. Haemophilia 26:1-158.
- Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, et al. (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a populationâ?based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67:93-99.
[Crossref] [Googlescholar] [Indexed]
- Bonds M, Rocha FG (2020) Neuroendocrine Tumors of the Pancreatobiliary and Gastrointestinal Tracts. Surg Clin N Am 100:635-648.
- Patel N, Barbieri A, Gibson J (2019) Neuroendocrine Tumors of the Gastrointestinal Tract and Pancreas. Surg Pathol Clin 12:1021–1044.
- Pape UF, Niederle B, Costa F, Gross D, Kelestimur F, et al. (2016) ENETS consensus guidelines for neuroendocrine neoplasms of the appendix (excluding goblet cell carcinomas). Neuroendocrinology 103:125-138.
- Rorstad O (2005) Prognostic indicators for carcinoid neuroendocrine tumors of the gastrointestinal tract. J Surg Oncol 89:151-60.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 