Research Article, J Nurs Patient Care Vol: 2 Issue: 2
Nurse-Midwives on the Front Lines: Serving the Rural and Medically Underserved
Patterson E1*, Hastings-Tolsma M2, Dunemn K3, Callahan TJ4, Tanner T5, Anderson J6 and HensleyJ7
1Kaiser Permanente Colorado, Denver, USA
2Baylor University, Louise Herrington School of Nursing, Dallas TX, USA
3University of Northern Colorado, School of Nursing, Greeley CO, USA
4University of Colorado Denver, School of Public Health, Aurora, CO, USA
5Frontier Nursing University, Hyden KY, USA
6University of Colorado Denver, Anschutz Medical Campus, School of Medicine, Aurora, CO, USA
7Vanderbilt University, School of Nursing, Nashville TN, USA
*Corresponding Author : Patterson E
Certified Nurse-Midwife, Kaiser Permanente Colorado, 1535 Taft CT, Louisville CO, USA, 80027
E-mail: epattcnm@gmail.com
Received: June 13, 2017 Accepted: June 22, 2017 Published: June 29, 2017
Citation: Patterson E, Hastings-Tolsma M, Dunemn K, Callahan TJ, Tanner T (2017) Nurse-Midwives on the Front Lines: Serving the Rural and Medically Underserved. J Nurs Patient Care 2:2. doi: 10.4172/2573-4571.1000117
Abstract
Background: Access to affordable, quality healthcare is a problem across the globe - especially for those in rural and medically underserved areas. Midwives have the potential to fill a significant void in access to quality maternal care providers. Objective: The purpose of this study was to examine differences in the scope and nature of nurse-midwifery care when working in rural or medically underserved areas, thus providing insight into needed changes in education, practice and health policy.
Design: This research used secondary data derived from a larger prospective descriptive workforce study of practicing nurse-midwives. Setting: Participants practicing as a nurse-midwife in one western state in the United States were recruited through the national certifying body, the American Midwifery Certification Board. Participants: All certified nurse-midwives (N=328) practicing in one large state in the United States were eligible to participate. The response rate was 32% (n=104) with 20% (n=21) of respondents working in rural or medically underserved areas of the State. Methods: A previously developed midwifery workforce survey was adapted for use. Following revision, the online survey was distributed and accessible for 3 weeks in 2014. RED CapTM was utilized for data management.
Results: Nurse-midwives working in non-medically underserved areas had significantly more collaborative practice guidelines, formal obstetrician/gynecologist and maternal foetal medicine consulting relationships, and in-house collaborating physicians. Nurse-midwives in rural or medically underserved areas primarily worked for community health centres or large safety-net medical facilities.
Conclusions: Healthcare systems are challenged to fully utilize nurse-midwives, eliminating practices that restrict them from working to their full-scope and excluding midwives from holding full medical staff membership. Strategies promoting long-term placement in rural and underserved areas also are needed.
Keywords: Nurse-midwives; Midwives; Nursing; Workforce; Rural; Medically underserved; Access to health care
Introduction
Affordable, quality healthcare has been a problem in the United States (U.S.) and across the globe where there has been ongoing struggle with healthcare provider shortages [1]. Differences in health and healthcare between population groups, referred to as health disparities, can be on the basis of age, gender, race/ethnicity, socioeconomic level, sexual orientation, disability, or geographic location [2]. Not only do healthcare disparities place significant burden on those impacted, but they also limit quality of care improvements and increase healthcare costs [3,4]. The challenge is to determine the best means of closing the gap where health disparities exist.
While passage of the Affordable Care Act (ACA) of 2010 provided a partial solution for issues related to healthcare access in the U.S.,[3] there remains an urgent need to consider strategies for the provision of services in Medically Underserved Areas (MUAs), as well as rural areas, which are often designated as health professional shortage areas [5]. With passage of this legislation, increasing numbers of patients moved into the healthcare system [6]. Supply of healthcare professionals, as well as maldistribution, impact inequities to needed healthcare services, especially in rural and MUAs, where shortages are often profound [7,8]. An increase in workforce capacity and increased access to quality healthcare have been recommended [9].
MUAs were originally designated in the U.S. as a method to identify areas and populations having limited access to primary care services [10]. Shortages are determined from an Index of Medical Underservice (IMU), which involves physician supply, infant mortality, percent of elderly, and poverty levels. MUAs are used mostly to qualify for state and federal programs aimed at providing increased healthcare services to MUAs and populations such as Community Health Centres (CHC), Federally Qualified Health Centres (FQHC), and certification as a rural health clinic [10].
Research has been conducted to ascertain challenges and opportunities in maintaining an maternity workforce in underserved areas [11]. Despite overall improvement in access to health care following passage of the ACA, the U.S. is faced with a shortage of obstetric providers; 46% of U.S. counties have no obstetrician/ gynecologist (OB/GYN) physician and 56% have no Certified Nurse- Midwives (CNM) [12]. This shortage, coupled with a projected 18% growth in the number of women in the U.S. by 2030 and an expected increase in births [13], raises significant concern for the healthcare of women [14]. Of note is a recent report of an increase in maternal mortality in the U.S. – a disturbing trend when rates have decreased in other countries [15]. Research has largely failed to address the role that CNMs play in sustaining reproductive healthcare services though utilization has been suggested as one solution to the problem of inequitable distribution of qualified women’s healthcare providers [6,14,16-18].
CNMs are capable of providing a full range of healthcare services for women including primary care, gynecologic and family planning services, preconception care, care throughout pregnancy and the postpartum, newborn care, and treatment of male partners for sexually transmitted infections [19]. Holding graduate degrees and nationally certified, CNMs provide care in varied settings including private practices, public health facilities, birth centres, and hospitalbased settings. The ability to provide full-scope practice is paramount to ensuring population-based access to high quality health care [20].
Access to reproductive services is of particular concern for those in rural and medically underserved areas. It has been noted that rural women have reduced access to health services and poorer health status than urban women [21]. CNMs, who provide a disproportionate amount of care to the vulnerable and underserved [22,23], are able to substantially impact availability of reproductive care – safely and at lower cost. Midwifery-led care has demonstrated lower rates of interventions than where care is provided solely by physicians [24], demonstrating its value to public health. This value is of particular importance where CNMs interface with FQHCs, CHCs, and certified rural health clinics, playing a central role in access to care.
During times of increasingly restrictive healthcare resources, understanding the care that CNMs provide is crucial. The purpose of this study was to examine the nature and scope of care provided by Colorado CNMs practicing in rural and MUAs. This research performed a more robust analysis of a larger workforce study [25].
Aims
Study aims were to 1) detail differences in the scope of care for CNMs practicing in rural or MUAs and CNMs practicing in nonrural or non-MUAs and 2) compare payer sources, employers, and collaborative agreements with physicians for CNMs practicing in rural or MUAs and CNMs in non-rural or non-MUAs.
Materials and Methods
Study design
A prospective descriptive study of CNMs practicing in the U.S. state of Colorado was completed in 2014. We performed a secondary analysis of the existing data set to examine differences in the scope and nature of nurse-midwifery care for those practicing in rural or MUAs and those practicing in other areas. The research was approved by the AMCB Research Committee and Executive Board, the Colorado Multiple Institutional Review Board (IRB) (#13-1394), and the IRBs of Frontier Nursing University (#20140214F), and the University of Northern Colorado (#564870-1).
Target population and sampling
Parent study: The main study conducted a statewide survey of all nurse-midwives (N=328) certified by the American Midwifery Certification Board (AMCB), the national certifying body in the U.S. Certification is required for nurse-midwifery practice in the U.S. Other midwife groups were excluded from participation, such as certified professional midwives, lay midwives, and midwifery students. An email of invitation, sent by the AMCB to those currently practicing in the state of Colorado, contained a URL link allowing access to the survey for a period of 3 weeks. The survey took less than one hour to complete and could be completed in more than one sitting. The survey that was used had been developed in a previous study [25]; it was then adapted and piloted prior to distribution. The survey contained 118 items related to demographics, employment, clinical practices, midwifery leadership, consultation/credentialing/ liability, prescriptive authority, teaching, professional satisfaction and future practice plans. REDCapTM (Research Electronic Data Capture) tools were used to provide a secure, web-based design to capture and manage data [26].
Current study: A subset of survey questions was used in this secondary research to examine differences in CNM practice when working in rural or MUAs or in other areas. Survey responses related to employment, zip code and county of practice, payer sources, care provided, employer, collaborating physicians, and self-identification of clinical practice in a rural area, were selected for subsequent analysis.
Survey responses were categorized based on location of CNM service. Two categories were identified: medically underserved (CNMs working in a rural setting ≤ 50,000 population) and/or where the practice zip code fell within a Federally-designated medically underserved area), and non-medically underserved (CNM working in an urban setting > 50,000 population) and/or where the practice zip code was not within a Federally-designated medically underserved area. These categories were selected as they were theoretically consistent and numbers of respondents working in rural areas precluded separate analyses and threatened respondent anonymity.
Data Analysis
Data preparation and statistical analyses were conducted using SPSS [21,27]. Descriptive analyses included Fishers Exact tests (comparing two independent proportions with small sample sizes) and Mann-Whitney U tests (comparing means from two independent populations with small sample sizes) to examine differences in birth attendance (yes/no), prescriptive authority (yes/no), written collaborative practice guidelines (yes/no), formal consulting relationships (yes/no; OB/GYNs, maternal foetal medicine specialists, family medicine physicians), physician collaborative (yes/ no; in-house physicians and physicians coming to facility), average level of patient risk, average amount of provided reproductive care, average number of received benefits, and average annual (pre-tax) salary by whether or not CNMs resided in or outside of a MUA.
Results
Sample characteristics
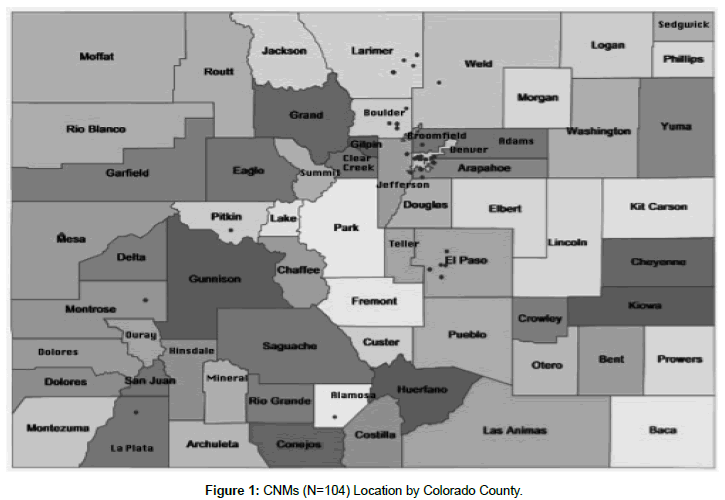
A total of 104 CNMs completed the survey for a response rate of 31.7%. Of this total, 20% worked in rural or MUAs. Most respondents were white, 56-65 years of age, and held a master’s degree. These demographic characteristics are likely representative of the CNM workforce in Colorado as findings are similar to those found on other state workforce survey [28]. While close to 15% were working on advanced degrees, few held doctoral degrees. Almost all who had doctoral preparation worked in non-MUAs (n=9, 13.6%). Most CNMs worked full-time; over a quarter were employed part-time or per diem (Table 1). All respondents practiced clinical midwifery as their primary employment. Survey respondents reported practicing in 15 of Colorado’s 64 counties. Twelve of these 15 counties are designated as MUAs. However, only 20.2% (n=17) of CNMs worked in rural or small towns ( ≤ 50,000 population) (Figure 1).
| Variable | N | % |
|---|---|---|
| Age (years) 25-35 36-45 46-55 56-65 66-75 |
14 21 20 39 10 |
13.5 20.2 19.2 37.5 9.6 |
| Race Asian/Pacific Islander White Hispanic/Latino/Spanish Missing |
1 99 3 1 |
1.0 95.2 2.9 1.0 |
| Professional Degree Associate’s Degree ND/DNP Degree Master’s Degree EdD Degree PhD Degree Other Missing |
1 6 88 1 6 1 1 |
1.0 5.8 84.6 1.0 5.8 1.0 1.0 |
| Pursing Advanced Degrees Yes No |
15 89 |
14.4 85.6 |
| Employment Status Full time Part time Per diem Retired Unemployed Not employed as a nurse-midwife Other |
57 18 12 4 3 9 1 |
54.8 17.3 11.5 3.8 2.9 8.7 1.0 |
Table 1: Demographic Characteristics of Nurse-Midwifery Respondents (N=104).
Scope of practice differences
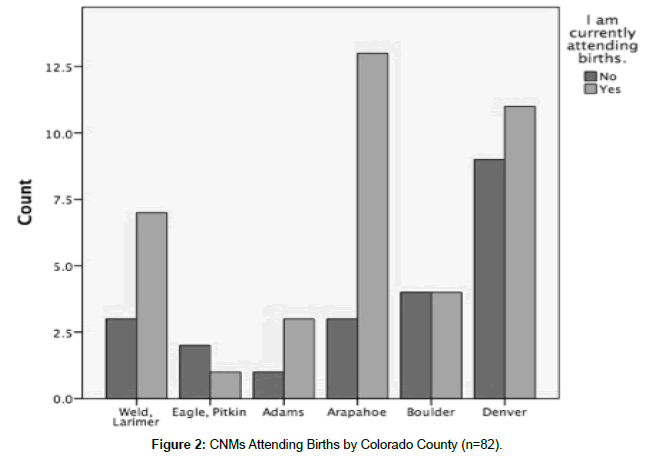
Fewer than 4% of respondents were non-white and all but one worked in non-MUAs. Births were attended by 64.9% (n=63) (Figure 2). When examined by practice location, births were attended by 76.5% (n=13) of those who worked in MUAs and 72.7% (n=48) of those who worked in non-MUAs. Births were most frequently attended in the hospital (n=53, 84.1%) although 6.3% (n=4) of respondents attended births in a free-standing birth centre. For CNMs attending birth, numbers ranged from fewer than 10 to over 100 per month. Additionally, 30.8% (n=4) of CNMs who worked in MUAs had full or associate medical staff membership compared to 23.4% (n=11) of CNMs in non-MUAs. Respondents reported caring for obstetrical patients of either low-moderate or moderate medical risk (n=71, 84.5%) but there was no significant difference in the average risk level when comparing MUA and non-MUA working CNMs (U=502.00, p=0.53). Additionally, there was no significant difference in birth attendance when comparing MUA and non-MUA working CNMs (p=1.00).
Over three-quarters of respondents held prescriptive authority (n=76, 78.4%) but there was no significant difference in having prescriptive authority when comparing CNMs who worked in MUAs or non-MUAs (p=0.29). However, CNMs who worked in non-MUAs were more likely to have written collaborative practice guidelines than those who worked in MUAs (p= 0.01).
Of those who provided primary care services, 35.3% (n=6) worked in MUAs and 25.4% (n=17) in non-MUAs. Other certifications (e.g., family nurse practitioner) were held by 50% (n=2) of those providing primary care in MUAs and 40% (n=4) in non-MUAs. On average, CNMs who worked in MUAs provided significantly more reproductive care than those who worked in non-MUAs (U=245.00, p=0.04).
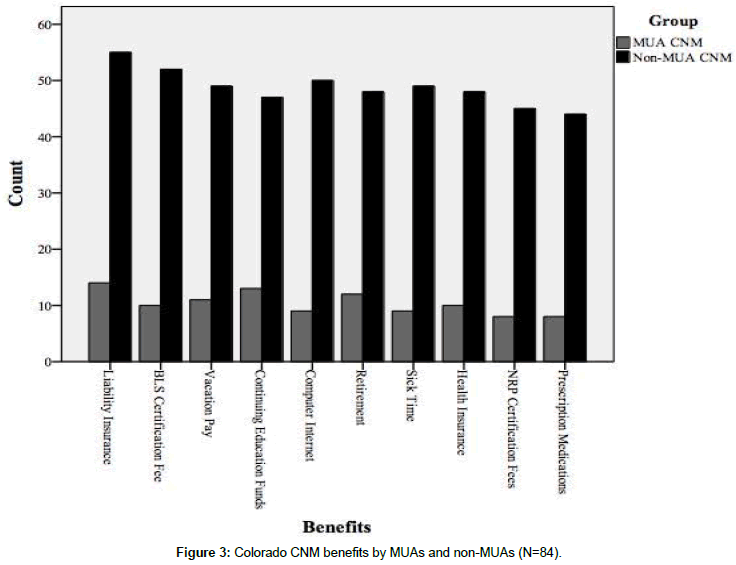
Loan forgiveness was reported by 12% of all respondents (n=11) but CNMs who worked in MUAs reported receiving less of such benefits (n=5, 33.3%) than those who worked in non-MUAs (n=6, 9.8%). The number of benefits received did not significantly differ when comparing CNMs who worked in an MUA versus non-MUA (U=632.00, p=0.22). There was no significant difference in the average annual (pre-tax) salary when comparing CNMs who worked in an MUA versus non-MUA (U=511.50, p=0.70) (Figure 3).
Comparison of payer, employers and collaborating physicians
Over 35% (n=38) of CNMs served populations where 50% or more of their patients were enrolled in government Medicaid and 70.6% (n=12) of respondents who worked in MUAs cared for such populations. Of note, CNMs who worked in MUAs were largely employed by either large safety-net medical facilities or community health centres (n=9, 53%). Over three-quarters of those who worked in MUAs attended births (n=13, 76.5%) and close to half held hospital membership as allied health providers (n=6, 46.2%); those who worked in non-MUAs were also most likely to hold hospital membership as allied health (n=25, 53.2%).
More than half of all CNMs (n=48, 52.2%) believed that a collaborative practice agreement with a physician was necessary though some indicated difficulty in developing a relationship with a physician. One respondent noted “Although I have attempted to engage local obstetricians, none were interested in working with me.” Significantly fewer CNMs who worked in MUAs had written collaborative practice guidelines than non-MUA working CNMs (p=0.01).
CNMs who worked in non-MUAs had significantly more formal consulting relationships with OB/GYNs (p=0.02) or maternal foetal medicine (MFM) specialists (p=0.03) and had more collaborating physicians in-house (p=0.03) than those who worked in MUAs. CNMs working in MUAs did not significantly differ in the number of collaborating physicians who come to the facility for consultation from non-MUA working CNMs (p=0.50). There was no significant difference in consultation with family medicine (FM) physicians when comparing MUA and non-MUA working CNMs (p=0.47).
Discussion
Limitations
Several limitations constrain the generalizability of study findings. First, only Colorado CNMs were surveyed and findings cannot be generalized to other U.S. states or countries. Only CNMs with a viable email address were included; it was unknown how many might have never received the invitations. No effort was made to follow up on non-respondents. Of those who responded, significant response bias may pose a threat. Additionally, the survey was retrospective in nature and accuracy of responses (e.g., number of births, payer mix for services provided and other perinatal outcomes) was not validated.
Respondents working in rural areas were grouped with those working in federally designated MUAs. Such grouping may have failed to identify characteristics that might differ between the two groups. Further, the grouping of respondents by urban (>50,000 population) and rural (≤ 50,000 population) setting resulted in small sample sizes; thus, results may lack generalizability. Future studies should aim to validate the current findings by recruiting larger subgroup sample sizes.
Findings provide insight into workforce differences for CNMs practicing in MUAs. Results underscore the need to re-examine two key factors crucial in the promotion of CNM care in those areas. These factors relate to midwifery access and quality care.
Access to midwifery care
Colorado has 64 counties with 16 designated as urban, 27 rural, and 21 frontier [29] with one in 5 Coloradans living in primary care health professional shortage areas [5]. Another Colorado survey found 4,590 advanced practice registered nurses (APRNs) in Colorado with 7% (n=312) self-identified as a CNM [30]. Colorado’s geographic diversity in the face of a paucity of CNMs underscores the challenge of delivering high quality, accessible health care. A scarcity of comprehensive data specifically related to CNM services further compounds the problem.
Timely access to affordable, quality healthcare reflects the aim of the ACA. With large numbers of U.S. counties lacking maternity care providers, there results significant access issues, long appointment wait-times, and long travel times for obstetrical care [31]. Colorado mirrors this problem where there is uneven distribution of the healthcare workforce [32] with 53% (n=34) of 64 counties lacking an OB/GYN physician and 33 counties (51%) lacking CNM access [31]. The numbers of OB/GYNs and CNMs are often closely aligned with interdisciplinary practice common for CNMs [33]. This study found that CNMs working in MUAs had fewer consulting arrangements with OB/GYNs and MFM specialists though consultation with FM physicians did not differ. This latter finding is of serious concern since the proportion of FM physicians providing maternity care has decreased from 23.3% in 2000 to 9.7% in 2010 [34].
The lack of maternity care providers in MUAs is significant. The ACA aspires to provide more primary and preventive care by expanding CHCs. And, between 2007 and 2012, there was a 61% increase in the number of FQHCs nationally, but only a 31% increase in the number of physicians [35]. Whether or not there has been an increase in the number of CNMs is unknown though there has been a 22% increase in newly certified nurse-midwives since 2000; [36] 8.4% of CNMs were found to work in CHCs [37]. Reduced access to maternity services impacts the ability to participate in crucial services such as prenatal care [38] - an important factor in decreasing the incidence of low-birth weight babies and premature births, [18,39-42] which in turn can decrease lifelong sequelae and increase healthcare costs. Further, where births are attended by a CNM, safety, less use of interventions, and fewer Cesarean births have been demonstrated [43] -all important considerations at a time where containment of healthcare cost is needed. Strategies to increase the number of CNMs and distribution to areas of greatest need are urgent especially since young women and children substantially represent those seen in CHCs [44].
Successful recruitment and retention of healthcare providers to MUAs, particularly rural settings, emphasizes loan forgiveness, training programs, as well as competitive salaries including economic incentives [45,46] Colorado CNMs who worked in MUAs were offered less loan repayment while their salaries did not significantly differ from those who worked in non-MUAs - a finding that suggests the need for alternate strategies that promote service to areas of high need for care. While Federal legislation has been enacted to increase the primary care workforce through support of select facilities that train CNMs and other APRNs [47] this program is currently limited to 5 hospital facilities. Program expansion to include non-hospital facilities could accelerate the education of well-qualified maternity care providers for both rural and MUAs. Research exploring issues of retention and recruitment for rural and MUA areas have stressed the importance of matching provider educational experiences with the proposed practice setting [45].
Finally, an important corollary is the need for increased numbers of racial/ethnic minority CNMs who more closely mirror populations served – a concern that has been noted on national study [48]. A small number of respondents in this survey were of racial/ethnic minority (n=4, 3.9%) though 32% of the Colorado population is non-Caucasian [49]. Despite a population of growing diversity, Colorado CNM demographics have changed little for nearly a decade, [50] an issue that has plagued nurse-midwifery across U.S. states [51]. Also of note was the lack of male respondents in this survey; small numbers in midwifery demonstrate the importance of recruitment efforts which promote openness. It is unknown how improvements in midwifery workforce diversity might impact care in MUAs but warrants further investigation.
Midwifery practice restrictions
The need to ease restrictions on CNM practice is clear. Current restrictive prescriptive authority regulations impact the decision to work in rural areas [52,53] and rigorous healthcare policy is needed to eliminate unnecessary control [30,54]. Conover and Richards [52] cited a 24% increase in APRN workforce when practice barriers were removed. Furthermore, offering a guaranteed salary draws APRNs to rural communities [55]. Standardization of practice laws for CNMs would cultivate a transformation for rural and underserved areas, strengthening health systems and improving outcomes.
Final considerations impacting CNM accessibility in MUAs are requirements for collaborative agreement with a physician to practice, and obtain hospital privileges. CNMs practicing in MUAs were less likely to have written collaborative practice agreements than CNMs who worked in non-MUAs, a finding that may reflect difficulty in arranging collaborative practice though survey methodology precluded further analysis. Most CNMs who worked in MUAs felt that a requirement for collaborative practice with a physician was necessary. This finding may reflect a desire for interdisciplinary collaboration and inclusion into existing healthcare system structures. Collaborative practice agreements are a requirement currently mandated by many hospitals for credentialing and for third-party reimbursement. These facts, however, create economic disadvantage for CNMs, limit patient access to reproductive care, and send a clear message that nurse-midwifery is not an independent profession. The ACA has been key in bringing attention to the need for increased access to CNM care and the importance of removing practice restrictions [56].
Access to quality care
While this study made no effort to determine quality of midwifery care, there is a need to strengthen not only access to the nurse-midwifery workforce but also the capacity to deliver quality care. In this study, few CNMs in MUAs held other certifications, such as family nurse practitioner, which might strengthen the capacity to provide expanded primary and preventative healthcare services. In addition, while most respondents working in MUAs worked for CHCs and large safety-net hospitals, fewer than 6% (n=1) of those working in MUAs held a doctoral degree. Research has found that APRNs working in rural Colorado are less likely to be educated to the highest level of the profession [28]. However, the study included nurse-midwives within the larger grouping of ‘nurse practitioner’ providing limited insight into the CNM workforce. Regardless, wellprepared CNMs who are capable of providing healthcare leadership within interdisciplinary teams are needed. The doctor of nursing practice (DNP) degree is now recommended for all APRNs in the U.S.; it holds much potential where adopted globally to place midwives at the forefront in working with integrated interdisciplinary teams in rapidly changing healthcare environments. The need for quality maternity services has been noted to be as important as access to care and the need is across high- and low-income countries [57]. To achieve such coupling of care, a paradigm shift is required to include transformative education promoting inter-professional collaboration and supportive practice environments.
Building teams to provide excellent patient outcomes is an essential goal of the ACA and mandates innovative approaches to achieve. Inter-professional education is important in recruiting new graduates to underserved areas and in cultivating a collaborative team practice that can strengthen health systems and improve outcomes [58,59], though more rigorous study is needed [41]. Models that situate the CNM as an equitable partner in healthcare decisionmaking are urgently needed, as are strategies to align education and healthcare delivery [60]. One instructive example is Project ECHO [61], which takes advantage of learning networks of expertise that are team-based, bringing specialized knowledge and best practices from the academic setting to clinical care sites. This model is of particular value to providers in MUAs, including rural settings.
Policy implications
Estimates that demand for healthcare services for women will grow over the next decade will require restructuring of health care. Solutions have been proposed to include easing of restrictions on CNM practice and strategies to encourage distribution to areas of shortage [14]. Research demonstrates that where the practice environment is restrictive for midwives, there is a smaller CNM workforce and a smaller number of CNM-attended births [62]. Policy makers are challenged to consider elimination of practices that restrict CNMs from working to their full-scope, as well as hospital privileges that exclude CNMs from holding full medical staff membership. Hospital bylaws that restrict full medical staff membership to physicians creates a power differential that is disingenuous in the creation of equitable partnerships that promote inter-professional collaboration [63]. Many aspects of practice regulation have been noted to relate to retention of professional privilege, status and power [64]. The scope of organization and delivery of healthcare services need to meet the needs of the public rather than the interests of professions.
Strategies that encourage long-term placement in MUAs are also needed, including CNM employment by health systems. Funding rural education programs or practicum experiences in rural communities with emphasis on CNM doctoral education is needed. Nurse-midwifery, an advanced practice nursing role in the U.S., is not uniformly delineated across states or across the globe. This lack of clarity about the role has hindered midwifery services and is crucial if maternity care is to be transformed for the underserved and most vulnerable [65]. Such emphasis would contribute to the development of midwifery leaders able to direct high impact services in a full-scope clinical practice.
Organizations in Colorado have established an educational program for rural APRNs [30] that should increase the numbers of APRNs practicing in such areas, including CNMs. A variety of strategies for increasing healthcare provider services in rural and MUAs have demonstrated limited success and innovative strategies are yet needed [66]. While research examining predictors of U.S. physicians in providing care to underserved populations found four factors (i.e., member of an underserved ethnic or minority group, participation in the National Health Service Corps, strong interest in the underserved, and from an underserved area), [67] it is unknown if these factors also apply to CNMs. In the U.S., robust and systematic nurse-midwifery workforce data are absent, making it difficult to determine the specific contribution CNMs make to healthcare. A strategy for the systematic collection and analysis of midwifery workforce data is crucial both in the U.S. as well as across the globe. Research approaches using the Internet could easily be used [68] and national and international health organizations are challenged to target such efforts.
If non-physician providers were fully utilized and effectively integrated into health systems, the projected shortage of primary care providers could be significantly reduced [69]. As designated maternity care and primary healthcare providers, [19] strong healthcare policy is needed to ensure access to CNMs who are capable of providing such services in a cost-effective manner.
Summary
Workforce study of midwives – often the largest group of maternity care providers across the globe – needs to be of high national and international priority [70] if access and quality of care for the medically underserved women of childbearing age is to be improved. Projected shortages of maternity care providers will disproportionately impact those in rural and medically underserved areas and is a looming crisis [71]. Results from this research shed light on the care provided by CNMs in MUAs in one U.S. state.
Access to CNMs who practice to the full extent of their preparation is crucial if the demands for obstetrical and primary care services are to be met. Further, robust data that disentangles the care provided by CNMs from that of other nurse providers is requisite to fully understand the extent and quality of service to those who are medically underserved and in great need of midwifery care.
Acknowledgements
The authors acknowledge support of the American College of Nurse Midwives CNM Colorado Affiliate, as well as the University of Colorado Denver, College of Nursing Center for Nursing Research. They would also like to thank Lori Haven, Data & Research Manager at the American Midwifery Certification Board and Susan K, Purcell MA, Project Specialist at the University of Colorado College of Nursing for her work in survey development and administration.
Funding
This research was supported by an award from the American Midwifery Certification Board, as well as an NIH/NCRR Colorado CTSI Grant (#UL1 TR001082).
References
- World Health Organization (2011) World Conference on Social Determinants of Health: Fact file on health inequities.
- Ubri P, Artiga S (2016) Disparities in health and health care: Five key questions and answers.
- Agency for Healthcare Research and Quality (2014) National Healthcare Quality and Disparities Report; Rockville, MD, Agency for Healthcare Research and Quality.
- Ayanian JZ (2015) The costs of racial disparities in health care.
- U.S. Department of Health and Human Services Health Resources and Services Administration. HRSA designated primary care health professional shortage areas (2016).
- Donelan K, DesRoches CM, Dittus RS, Buerhaus P (2013) Perspectives of physicians and nurse practitioners on primary care practice. N Engl J Med 368: 1898-1906.
- Grumbach K, Hart LG, Mertz E, Coffman J, Palazzo L (2003) Who is caring for the underserved? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Ann Fam Med 1: 97-104.
- Rural Health Information Hub (2016) Rural Healthcare Workforce.
- National Prevention Council (2011) National Prevention Strategy.
- U.S.Department of Health and Human Services Health Resources and Services Administration. Medically underserved areas (MUAs) and populations (MUPs) (2015).
- Kozhimannil KB, Casey MM, Hung P, Han X, Prasad S, et al. (2015) The rural obstetric workforce in US hospitals: Challenges and opportunities. J Rural Health 31: 365-372.
- American College of Nurse-Midwives (2015) The role of certified nurse-midwives and certified midwives in ensuring women's access to skilled maternity care.
- Colby SL, Ortman JM (2015) Projections of the size and composition of the U.S. population: 2014 to 2060.
- Ollove M (2016) A shortage in the nation's maternal health care.
- MacDorman MF, Declercq ER, Cabral H, Morton C (2016) Recent Increases in the U.S. maternal mortality rate: Disentangling trends from measurement issues. Obstet Gynecol 128: 447-455.
- Garson A (2013) New systems of care can leverage the health care workforce: How many doctors do we really need? Acad Med 88: 1821.
- MacDowell M, Glasser M, Fitts M, Nielsen K, Hunsaker M (2010) A national view of rural health workforce issues in the USA. Rural Remote Health 10: 1531.
- Munro S, Kornelsen J, Grzybowski S (2013) Models of maternity care in rural environments: Barriers and attributes of interprofessional collaboration with midwives. Midwifery 29: 646-652.
- American College of Nurse-Midwives (2011) Definition of midwifery and scope of practice of certified nurse-midwives and certified midwives.
- Institute of Medicine (2011) The Future of Nursing: Leading Change, Advancing Health.
- American College of Obstetricians and Gynecologists (2014) ACOG Committee Opinion No. 586: Health disparities in rural women. Obstet Gynecol 123: 384-388.
- Declercq ER, Williams DR, Koontz AM, Paine LL, Streit EL, et al. (2001) Serving women in need: Nurse-midwifery practice in the United States. J Midwifery Womens Health 46: 11-16.
- Newhouse RP, Stanik-Hutt J, White KM et al. (2011) Advanced practice nurse outcomes 1990-2008: A systematic review. Nurs Econ 29: 230-250.
- Johantgen M, Fountain L, Zangaro G, Newhouse R, Stanik-Hutt J, et al. (2012) Comparison of labor and delivery care provided by certified nurse-midwives and physicians: a systematic review, 1990 to 2008. Womens Health Iss 22: e73-e81.
- Blinded for review.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, et al. (2009) Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42: 377-381.
- IBM Corporation (2012) IBM SPSS Statistics for Macintosh. Version 21.0; Armonk, NY, IBM Corp.
- Colorado Health Institute (2012) A Profile of Colorado's Advanced Practice Nurse Workforce.
- Colorado Department of Public Health and Environment (2016) Maternal and child health snapshot.
- Colorado Center for Nursing Excellence (2015) Colorado's future healthcare workforce and the role of advanced practice registered nurses
- U.S. Department of Health and Human Services Health Resources and Services Administration. Health workforce (2013).
- Colorado Center for Nursing Excellence (2010) The nursing and health care workforce in Colorado: Driver of prosperity or an economic roadblock?.
- Kozhimannil KB, Henning-Smith C, Hung P (2016) The practice of midwifery in rural US hospitals. J Midwifery Womens Health 61: 411-418.
- Tong ST, Makaroff LA, Xierali IM (2012) Proportion of family physicians providing maternity care continues to decline. J Am Board Fam Med 253: 270-271.
- Proser M, Bysshe T, Weaver D, Yee R (2015) Community health centers at the crossroads: Growth and staffing needs. JAAPA 28: 49-53.
- American Midwifery Certification Board (2015) American Midwifery Certification 2015 Annual Report.
- American College of Nurse-Midwives (2010) ACNM compensation & benefits survey: Key findings among certified nurse-midwives and certified midwives.
- U.S. Department of Health and Human Services HRaSAMaCHB (2013) Child Health USA 2013; Rockville, MD, U.S. Department of Health and Human Services.
- Gortmaker SL (1979) The effects of prenatal care upon the health of the newborn. Am J Public Health 69: 653-660.
- Kotelchuck M (1994) The adequacy of prenatal care utilization index: Its US distribution and association with low birthweight. Am J Public Health 84: 1486-1489.
- Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M (2013) Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database Syst Rev CD002213.
- Varney H, Kriegs J, Gegor CL (2004) Varney's Midwifery. Jones & Bartlett Publications, USA.
- Sandall J, Soltani H, Gates S, Shennan A, Devane D (2013) Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev CD004667.
- Adashi EY, Geiger HJ, Fine MD (2010) Health care reform and primary care--the growing importance of the community health center. N Engl J Med 362: 2047-2050.
- Daniels ZM, Vanleit BJ, Skipper BJ, Sanders ML, Rhyne RL (2007) Factors in recruiting and retaining health professionals for rural practice. J Rural Health 23: 62-71.
- Roy V, Hurley K, Plumb E, Castellan C, McManus P (2015) Urban underserved program: An analysis of factors affecting practice outcomes. Fam Med 47: 373-377.
- Centers for Medicare & Medicaid Services (2015) Graduate nurse education demonstration.
- Fullerton J, Sipe TA, Hastings-Tolsma M et al. (2015) The midwifery workforce: ACNM 2012 and AMCB 2013 core data. J Midwifery Womens Health 60: 751-761.
- U.S. Census Bureau (2015) QuickFacts: Colorado.
- Hastings-Tolsma M, Tasaka Y, Burton A, Goodman S, Emeis CL, et al. (2009) A profile of Colorado nurse-midwives: Implications for health care. West J Nurs Res 31: 24-43.
- DeLibertis J (2016) American College of Nurse-Midwives (ACNM). Shifting the frame: A report on diversity and inclusion in the American College of Nurse-Midwives.
- Conover C, Richards R (2015) Economic benefits of less restrictive regulation of advanced practice nurses in North Carolina-an analysis of local and statewide effects on business activity.
- Phillips SJ (2014) 26th annual legislative update: Progress for APRN authority to practice. Nurse Pract 39: 29-52.
- Kleinpell R, Scanlon A, Hibbert D, Ganz F, East L, et al. (2014) Addressing issues impacting advanced nursing practice worldwide Online J Issues Nurs 19: 5.
- Fellows J (2015) Following physician compensation trends? Read this first.
- Walker D, Lannen B, Rossie D (2014) Midwifery practice and education: Current challenges and opportunities. Online J Issues Nurs 19: 4.
- Campbell J, Sochas L, Cometto G, Matthews Z (2016) Evidence for action on improving the maternal and newborn health workforce: The basis for quality care. Int J Gynaecol Obstet 132: 126-129.
- Deutschlander S, Suter E, Grymonpre R (2013) Interprofessional practice education: Is the 'interprofessional' component relevant to recruiting new graduates to underserved areas? Rural Remote Health 13: 248.
- World Health Organization (2015) Framework for action of interprofessional education & collaborative practice.
- Institute of Medicine (2015) Measuring the Impact of Interprofessional Education (IPE) on Collaborative Practice and Patient Outcomes.
- Arora S, Kalishman S, Dion D et al. (2011) Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care. Health Aff 30: 1176-1184.
- Yang YT, Attanasio LB, Kozhimannil KB (2016) State scope of practice laws, nurse-midwifery workforce, and childbirth procedures and outcomes. Womens Health Issues 26: 262-267.
- Shamian J (2014) Interprofessional collaboration, the only way to save every woman and every child. Lancet 384: e41-e42.
- Cameron PA, Thompson DR (2005) Changing the health-care workforce. Int J Nurs Pract 11: 1-4.
- Dowling M, Beauchesne M, Farrelly F, Murphy K (2013) Advanced practice nursing: A concept analysis. Int J Nurs Pract 19: 131-140.
- Grobler L, Marais BJ, Mabunda SA, Marindi PN, Reuter H, et al. (2009) Interventions for increasing the proportion of health professionals practising in rural and other underserved areas. Cochrane Database Syst Rev 21: CD005314.
- Rabinowitz HK, Paynter NP (2000) The role of the medical school in rural graduate medical education: Pipeline or control valve? J Rural Health 16: 249-253.
- Huntington A, Gilmour J, Schluter P, Tuckett A, Bogossian R, et al. (2009) The Internet as a research site: establishment of a web-based longitudinal study of the nursing and midwifery workforce in three countries. J Adv Nurs 65: 1309-1317.
- U.S. Department of Health and Human Services Health Resources and Services Administration (2013) Projecting the supply and demand for primary care practitioners through 2020.
- Perry L (2015) Working well? Studying the nursing workforce. Int J Nurs Pract Practice 21: 337-338.
- Blanchette H (2012) The impending crisis in the decline of family physicians providing maternity care. J Am Board Fam Med 25: 272-273.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi