Research Article, Clin Dermatol Res J Vol: 9 Issue: 5
Psychiatric comorbidities and impaired daily living in Pityriasis Rubra Pilaris
Donald K. Lei1*, Scott Worswick2, Nolan J Maloney3, Mindy M Kim3 and Lauren Cutler2
1Department of Dermatology, University of Chicago Pritzker School of Medicine, USA
2Department of Dermatology,University of Southern California, USA
3Department of Dermatology, Stanford University, USA
*Corresponding Author: Donald K. Lei MS,Department of Dermatology, University of Chicago Pritzker School of Medicine, 5841 S. Maryland Ave, IL 60637Chicago, USA Tel: 630-532-1559 E-mail: Donald.lei@uchospitals.edu
Received: October 16, 2020 Accepted: November 18, 2020 Published: November 25, 2020
Citation: Lei DK, Worswick S, Maloney NJ, Kim MM, Cutler L (2020) Psychiatric comorbidities and impaired daily living in Pityriasis Rubra Pilaris. Clin Dermatol Res J 5:3.
Abstract
Objective: To investigate the impact of Pityriasis Rubra Pilaris (PRP) on psychosocial health and daily life. Methods: Members of the PRP Facebook support group and an email listing (approximately 1979 patients) were invited to complete the study. Results: Of 625 responses, 307 patients met inclusion criteria. The mean Dermatology Life Quality Index (DLQI) score for PRP patients was 11.5 ± 8.4. 23.1% of patients reported anxiety, and 61.9% of patients reported depression. 58.6% of patients reported that their disease significantly impacted their ability to work or attend school, and 69.4% reported mobility issues. 60.9% of patients had a > 50% reduction in sleep. Only 9.1% reported that their dermatologist referred to a psychologist or psychiatrist. Mean DLQI scores were higher for patients who reported anxiety, depression, or had work/school, mobility, and sleep issues compared to those who did not. Patients referred to psychiatrists or psychologists had mean DLQI scores of 16.4, compared to 11.0 in those who were not (P=0.0012). Conclusion: Psychiatric comorbidities and impairment of daily life are highly prevalent in PRP patients, and contribute to poor Quality of Life (QOL). In spite of this, few patients are referred to psychiatry or psychology, and those who are score significantly higher on the DLQI.
Keywords: Pityriasis Rubra Pilaris, Psych, Anxiety, Depression, QOL, DLQI
Keywords
Pityriasis Rubra Pilaris;Psych; Anxiety;Depression; QOL; DLQI
Introduction
Adult-onset Pityriasis Rubra Pilaris (PRP) is a rare papulosquamous inflammatory dermatosis that can present with many debilitating symptoms, including hyperkeratotic follicular papules, ectropion, pruritus, palmoplantar keratoderma, and joint pain [1-3]. Since the clinical presentation of PRP can be variable and mimic atopic dermatitis or psoriasis, patients are often initially misdiagnosed. Once diagnosed, PRP is often resistant to topical and systemic therapy and even in cases of spontaneous regression it often takes 1-3 years to enter remission [1].
PRP has a significant impact on patient quality of life (QOL) [4]. However, which aspects of PRP contribute the most to impaired QOL are poorly characterized. Though disease features undoubtedly play a large role, the psychosocial and occupational consequences of living with a chronic dermatologic condition cannot be understated. In a large study of common dermatologic conditions, patients were found to have higher rates of depression and anxiety than the general population [5]. Additionally, many patients with skin conditions can become too disabled to work or suffer from decreased productivity at work [6]. One study of 22 common skin diseases in 2004 estimated that skin disease contributed to a 10.2-billion-dollar loss of productivity in the United States alone [7].
Since these concepts have never been investigated in PRP cohorts, we performed a large, survey-based study to quantify the burden of co-morbid psychiatric illness and the degree to which their disease impacts daily life. In addition, we hypothesized that these factors would be relevant and important contributors to overall quality of life QOL.
Methods
We performed a retrospective, online, anonymous Qualtrics survey study of PRP patients. We recruited participants through the PRP Facebook Support Group and a separate email listing from the PRP Alliance. An IRB exemption was in place for this project at UCLA during data collection and initial data analysis, and at USC during data analysis to retrospectively study rashes including Pityriasis rubra pilaris. In total, 625 patients, of which 307 qualified for inclusion. Inclusion criteria were: diagnosis of PRP by a dermatologist, >18 years of age at survey completion, and completion of the Dermatology Life Quality Index (DLQI) instrument [8]. Participants self-reported current age, age at diagnosis, sex, and ethnicity. They were also asked to complete the DLQI and answer questions about psychiatric co-morbidities such as anxiety and depression, as well as how their disease affected their ability to go to work or school, perform daily activities, or sleep.
Analyses were performed in SAS 9.4 (Cary, NC) and graphs created in Graphpad Prism 7. Univariate analyses comparing mean DLQI scores were performed using the Kruskal-Wallis test. Normality of data was tested using the Shapiro-Wilks test.
Results
Study participants were 58.0% female, 92.2% Caucasian, had a mean age at survey completion of 57.1 ± 13.4 years, and a mean age at diagnosis of 52.7 ± 16.4 years. Overall, the mean DLQI score was 11.5 ± 8.4 on a scale of 0 to 30, with higher scores suggesting greater QOL impairment (Table 1).
| Patient Characteristics | |
| (n = 307) | |
| Current Age | |
| Mean ± SD | 57.09 ± 13.40 |
| Age at Diagnosis | |
| Mean ± SD | 52.70 ± 16.44 |
| < 18 | 25 (8.14%) |
| 18 - 40 | 34 (11.07%) |
| 41 - 65 | 181 (58.96%) |
| > 65 | 61 (19.87%) |
| Gender | |
| Male | 129 (42.02%) |
| Female | 178 (57.98%) |
| Race | |
| Caucasian | 283 (92.18%) |
| African American | 6 (1.95%) |
| Hispanic | 1 (0.33%) |
| Asian | 1 (0.33%) |
| Other/Unreported | 7 (2.28%) |
| DLQI Score (mean ± SD) | 11.50 ± 8.42 |
Table 1: Patient Characteristics.
71 patients (23.1%) reported anxiety and 190 (61.9%) reported feeling depressed (Table 2). When asked about their anxiety or depression, 62/71 (87%) felt the most anxious and 168/190 (88.4%) felt the most depressed about or due to their PRP. In addition, 180 patients (58.6%) reported that PRP had a substantial impact on their ability to work or attend school, 213 (69.4%) had mobility issues severe enough to interfere with daily activities, and 187 (60.9%) had severe sleep disturbance (>50% reduction in sleep). However, only a minority of patients – 28 (9.1%) – were referred to see either a psychiatrist or psychologist.
| Number | Proportion of All Patients | |
|---|---|---|
| Anxiety | 71 | 23.13% |
| Anxiety due to PRP | 62 | 20.20% |
| Other reasons | 9 | 2.93% |
| Depression | 190 | 61.89% |
| Depression due to PRP | 168 | 54.72% |
| Other reasons | 22 | 7.17% |
| Work or school impacted | 180 | 58.63% |
| Mobility impacted | 213 | 69.38% |
| Sleep impacted | 187 | 60.91% |
| Referred to a psychiatrist or psychologist | 28 | 9.12% |
Table 2. Prevalence of psychiatric co-morbidities and impaired daily living.
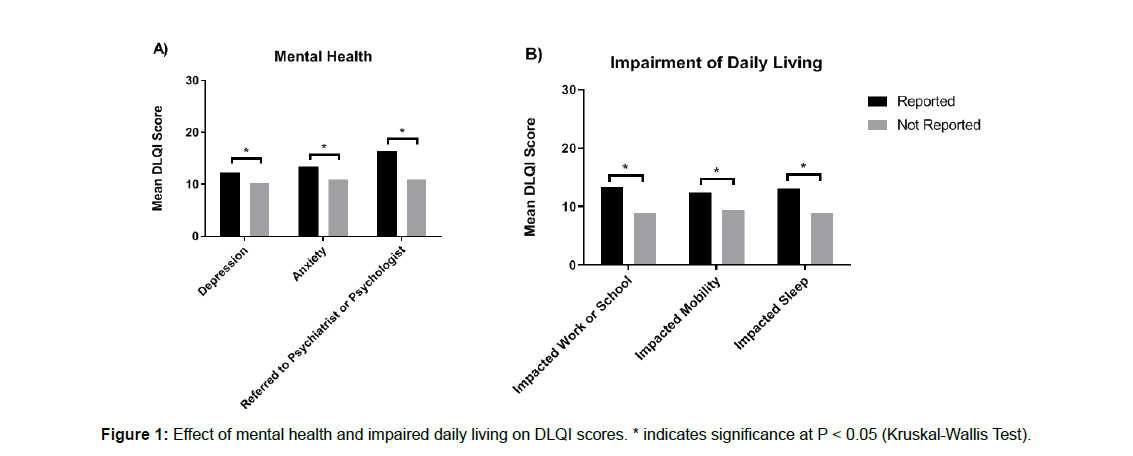
Mean DLQI scores were compared based on whether patients reported depression, anxiety, impaired work/school, mobility, sleep, or referral to psychiatry/psychology (Figure 1). Patients reporting depression had mean DLQI scores of 12.2 compared to those 10.3 for those who did not (P = 0.045). Those who reported anxiety had mean DLQI scores of 13.4 vs. 10.9 for those who did not (P = 0.026). Those referred to either a psychiatrist or psychologist had mean DLQI scores of 16.4 vs 11.0 for those who were not (P=0.0012). Patients who reported an impairment of their ability to work or attend school reported mean DLQI scores of 13.3 vs. 9.0 for those who did not (P<0.0001). Those who had mobility issues impacting daily activities had mean DLQI scores of 12.4 vs. 9.4 (P=0.0132), and those who had significant (>50% reduction) in sleep had mean DLQI scores of 13.1 vs. 8.9 (P<0.0001).
Discussion
Psychological disorders are highly prevalent in patients with skin disease. A large, multinational study of common skin diseases demonstrated higher rates of clinical depression and anxiety disorder than healthy controls (10.1% vs. 4.3% and 17.2% vs. 11.1% respectively) [5]. In comparison, we see a much higher proportion of depression or anxiety (61.9% and 23.1%) in patients with PRP. Though patients who self-report depression and anxiety may not meet DSM-V criteria, those who reported depression or anxiety had significantly higher DLQI scores than those who did not. This highlights the high burden of psychologic distress on patients, as well as the relevance of psychiatric comorbidity to QOL. Furthermore, very few patients (9.1%) were referred to psychologists or psychiatrists, and those that did had substantially higher DLQI scores than those who did not (16.4 vs. 11.1). This suggests that many patients who could benefit from mental health interventions are not receiving them, and that many patients are only being referred once their QOL has substantially deteriorated.
Our study also identifies a high burden of functional impairment and sleep disturbance in PRP. Over half of all patients reported a > 50% reduction in sleep or that their disease greatly affected their mobility or ability to work and attend school. These patients also had significantly higher DLQI scores than unaffected PRP patients, highlighting the relevance of these sequelae. It is unclear what aspects of PRP contribute the most to these impairments. Palmoplantar keratoderma and joint pain may impact mobility and make occupational tasks difficult to complete, and nocturnal skin pruritus may lead to sleep disturbance.
Our cohort had a mean DLQI score of 11.5, which would be classified as having a “very large effect on patient’s life” [9]. To put this into perspective, other studies common skin diseases have shown lower mean DLQI scores (Atopic Dermatitis (AD) – 5.30 to 11.94 from mild to severe AD [10], pemphigus – 10.18 [11], acne – 7.22 [12], psoriasis – 6.78 [13]). This is consistent with a prior study by Eastham et al., which similarly showed worse QOL in PRP than these conditions via Skindex-29 scores. It is worth noting that the Minimum Clinically Important Difference (MCID) for DLQI scores in inflammatory skin diseases was determined to be 4 points [14]. Most of the inter-group differences in DLQI scores in our study were less than 4 points, though the significance of these differences still speaks to the relevance of each factor and does not take into account the possible additive or multiplicative interactions these factors may have with one another.
One of the biggest strengths of our study is the large cohort of PRP patients. However, we recognize the following limitations. First, the results of our study may be affected by response bias as patients voluntarily completed the survey. Recall bias is likely, as well as selection bias, with patients with more severe disease or longer disease course more likely to seek out online support groups. Additionally, our cohort is primarily Caucasian, which limits generalizability to non-Caucasian PRP patients. Finally, patients self-reported all information. Though participants were only included if they noted a dermatologist-confirmed diagnosis of PRP, self-reports of depression and anxiety may not meet clinical diagnostic criteria, and therefore the true prevalence of these conditions may be lower than what we observed.
Conclusion
Many patients with PRP report anxiety or depression, as well as an impairment of their ability to work, attend school, and perform daily activities. Patients who are affected in these ways experience worse overall quality of life, though they are seldom referred to psychologists or psychiatrists for management.
Further work is necessary to fully understand the impact of PRP and to develop effective management strategies, but dermatologists should be encouraged to routinely screen PRP patients for psychiatric comorbidities and help coordinate the appropriate interventions.
References
- Klein A, Landthaler M, Karrer S (2010) Pityriasis rubra pilaris: a review of diagnosis and treatment. Am J Clin Dermatol 11:157-170.
- Griffiths WA (1975) Pityriasis rubra pilaris- an historical approach. Trans St Johns Hops Dermatol Soc 61: 58-69.
- Eastham AB (2019) Pityriasis Rubra Pilaris. JAMA Dermatology 155: 404.
- Eastham AB, Tkachenko EY, Femia AN, Pappas-Taffer LK, Rosenbach M et al. (2019) Pityriasis rubra pilaris: A study evaluating patient quality of life in 2 populations. J Am Acad Dermatol 81: 638-640.
- Dalgard FJ, Gieler U, Tomas-Aragones L, Lien L, Poot F et al. (2015) The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol 135: 984-991.
- Hong J, Koo B, Koo J (2008) The psychosocial and occupational impact of chronic skin disease. Dermatol Ther 21: 54-59.
- Bickers DR, Lim HW, Margolis D, Weinstock MA, Goodman C et al. (2006) The burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. J Am Acad Dermatol 55: 490-500.
- Finlay AY, Khan GK (1994) Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin Exp Dermatol 19: 210-216.
- Hongbo Y, Thomas CL, Harrison MA, Salek MS, Finlay AY (2005) Translating the science of quality of life into practice: What do dermatology life quality index scores mean? J Invest Dermatol 125: 659-664.
- Holm JG, Agner T, Clausen ML, Thomsen SF (2016) Quality of life and disease severity in patients with atopic dermatitis. J Eur Acad Dermatol Venereol 30: 1760-1767.
- Sung JY, Roh MR, Kim SC (2015) Quality of Life Assessment in Korean Patients with Pemphigus. Annals of dermatology 27: 492-498.
- Hazarika N, Rajaprabha RK (2016) Assessment of Life Quality Index Among Patients with Acne Vulgaris in a Suburban Population. Indian J Dermatol 61: 163-168.
- Rencz, F, Gulácsi L, Péntek M, Szegedi A, Remenyik E (2020) DLQI-R scoring improves the discriminatory power of the Dermatology Life Quality Index in patients with psoriasis, pemphigus and morphea. Br J Dermatol 182: 1167-1175.
- Basra MK, Salek MS, Camilleri L, Sturkey R, Finlay AY (2015) Determining the minimal clinically important difference and responsiveness of the Dermatology Life Quality Index (DLQI): further data. Dermatology 230: 27-33.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi