Research Article, Clin Res Orthop Vol: 3 Issue: 1
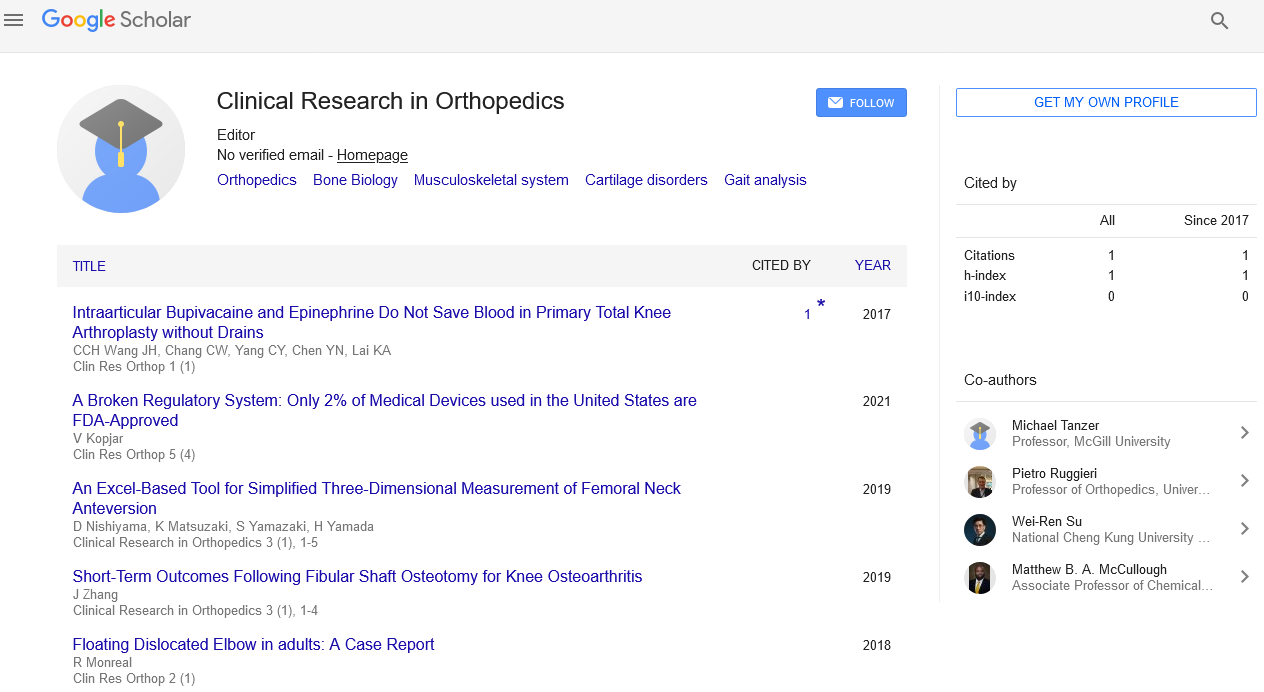
Short-Term Outcomes Following Fibular Shaft Osteotomy for Knee Osteoarthritis
Haibo Lu1,2, Kejian Wu1, Jian Zhang1*, Xiaoning Wang1, Junjun Tang1, Xin Huang1, Yonggang Zhang1, Guanglin Wang1, Yingbo Zhu1 and Jinchang Wang1
1Department of Orthopaedics, the First Affiliated Hospital of Chinese PLA General Hospital, Beijing, China
2Department of Clinic, Hospital of PLA Hong Kong Garrison, Hong Kong SAR, China
*Corresponding Author : Jian Zhang
Department of Orthopaedic Trauma, the First Affiliated Hospital of Chinese PLA General Hospital, Beijing, China
Tel: +86- 13691133526
E-mail: quanyiguodocy@163.com
Received: August 15, 2019 Accepted: September 12, 2019 Published: September 17, 2019
Citation: Haibo L, Kejian W, Xiaoning W, Junjun T, Xin H, et al. (2019) Short-Term Outcomes Following Fibular Shaft Osteotomy for Knee Osteoarthritis. Clin Res Orthop 3:1.
Abstract
Purpose: To evaluate short-term outcomes following fibular shaft osteotomy (FSO) for knee osteoarthritis.
Methods: We retrospectively reviewed data from 15 patients (20 knees) undergoing FSO between April 2016 and April 2017. We measured the ratio of bilateral distances of the knee compartment (Rd) pre- and post-FSO, and conducted clinical evaluations using a visual analog pain scale (VAS) and the Knee Society Score. In addition, operation time, blood loss, and length of hospitalization of FSO patients were compared with those of 17 patients (20 knees) undergoing total knee
arthroplasty (TKA).
Results: Rd showed a non-significant increase from a mean of 0.32 pre-FSO to 0.50 post-FSO (p=0.056). However, VAS was significantly decreased (mean of 7.72 pre-FSO versus 1.89 at 48 h postoperatively, p=0.000) and average pain, knee, and functional scores were all significantly increased. Compared with TKA, operation time and length of hospitalization were significantly shorter with FSO (respectively, 131.3 versus 55.3 min, p=0.000; and 11.72 versus 5.76 days, p=0.000), and blood
loss was significantly lower (16.0 versus 122.22 ml, p=0.000).
Conclusion: FSO has an instant pain-relieving effect and is associated with rapid patient recovery. The use of FSO might be one step of staircase therapy for knee osteoarthritis.
Keywords: Fibular shaft osteotomy; Knee osteoarthritis; Osteoarthritis
Introduction
Patients are increasingly presenting with unicompartmental knee arthritis at an age and activity level that are less than ideal for total knee arthroplasty (TKA) [1]. For isolated medial unicompartmental knee osteoarthritis (OA), both unicompartmental knee arthroplasty and high tibial osteotomy are viable options [2-5]. Most clinicians would likely agree that either technique would be appropriate in active, non-obese patients, aged 60-65 years, who have well-preserved joint alignment (less than 5-10 degrees varus), stability, and range of motion, and a lack of significant patella femoral and/or contracompartmental OA. However, for these patients making up an increasing proportion of OA patients and, with their higher expectations for pain relief and function rehabilitation, it might be better to be treated with more minimally invasive techniques.
In this study, we present a more minimally invasive technique, fibular shaft osteotomy (FSO), for the treatment of relatively young patients with isolated medial unicompartmental knee OA.
Materials and Methods
Study design
The ethics committee of our hospital approved this study. We retrospectively reviewed data from 15 patients (20 knees) who underwent FSO and 17 patients (20 knees) who underwent TKA for OA of the knee from April 2016 to April 2017. The mean follow up was 135.47 days (range 12-381 days).
Our inclusion and exclusion criteria were similar to those of Lee et al [6]. Patients with symptomatic isolated femorotibial (FT) medial OA were included. Patients were required to have: (1) Kellgren–Lawrence grades 2-4 radiographic FT medial OA with varus malalignment and an intact radiographic joint space at the lateral FT compartment; and (2) significant and disabling pain originating from the medial side of the knee that had not responded to more than 3 months of conservative measures. (Kellgren-Lawrence grades of OA severity: 0 = no OA present; 1 = doubtful narrowing of joint space and possible osteophytic lipping; 2 = definite osteophytes, definite narrowing of joint space; 3 = moderate multiple osteophytes, definite narrowing of joint space, some sclerosis and possible deformity of bone contour; 4 = large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone contour [7].)
Patients with conditions other than isolated FT medial OA, such as rheumatoid arthritis, ligament injuries (posterolateral corner injury of the knee and anterior cruciate ligament injury), developmental deformity of the knee, or malunion of a proximal tibial fracture, were excluded from this study. Patient demographics are shown in Table 1.
| Characteristics | FSO group, n (%) | TKA group, n (%) |
|---|---|---|
| Age, years | ||
| 51–55 | 4 (26.7) | 0 (0) |
| 56–65 | 5 (33.3) | 5 (29.4) |
| 66–75 | 6 (40) | 9 (52.9) |
| 76–85 | 0 (0) | 3 (17.6) |
| Men | 6 (40) | 7 (41.2) |
| Operation side | ||
| Left | 3 (20) | 6 (35.3) |
| Right | 7 (46.7) | 8 (47.1) |
| Bilateral | 5 (33.3) | 3 (17.6) |
| Kellgren–Lawrence grade | ||
| 2 | 6 (30) | 5 (25) |
| 3 | 10 (50) | 9 (45) |
| 4 | 4 (20) | 6 (30) |
Table 1: Patient demographics, FSO-fibular shaft osteotomy; TKAtotal knee arthroplasty
Surgical technique
All patients undergoing FSO were treated with the same protocol. At 1 h before surgery and every 12 h postoperatively for 48 h, each patient was given a prophylactic intravenous injection of cefuroxime sodium (1.5 g). All FSO procedures were performed using a 5 cm longitudinal skin incision, 10 cm distal to the fibular head. Through the space between the musculus peroneus brevis and the longus, the fibula shaft was exposed and a 1-1.5 cm defect was made using a goose saw.
After the osteotomized bone block was removed, two holes of 2.5 mm diameter were made 0.5 cm adjacent to the proximal and distal ends of the defect. One nylon suture (1.0 mm diameter) was passed through the two holes and tied tightly. The incision was closed using an interrupted suture. Wound drainage strips were applied for 48 h. All patients received a single intravenous dose of analgesic (100 ml flurbiprofen) at 2 h postoperatively. All patients were allowed to walk with full weight-bearing after the surgery.
X-ray evaluation
X-ray evaluation was performed by measuring the distance ratio (Rd) in pre- and postoperative standing full-limb anteroposterior (AP) radiographs. As described previously by Lee et al [6], we obtained standing full-limb AP radiographs on a 14×51 inch (36×130 cm) grid cassette at a source-to-image distance of 240 cm using a UT 2000 Xray machine (Philips Research, Eindhoven, The Netherlands) set to 90 kV and 50 mA/s. To control the rotational position of the AP radiograph, the foot rotation angle was held constant with a reference foot template on the platform of our plane radiographic system. In addition, the appropriate knee position (patellar facing forward) was confirmed using a preview monitor before final acquisition of the whole-limb AP radiograph.
All radiographic images were digitally acquired using a picture archiving and communication system (PACS). The images were assessed using a 24 inch (61 cm) monitor (U2412 M; Dell, Round Rock, TX, USA) in portrait mode using PACS software (Infinite, Seoul, Korea), which allowed the investigator to detect the bisecting point of any area on the femur or tibia and to measure the angle between any two lines drawn on the digital image. The minimum differences that the software could detect were 0.1 mm in length.
For X-ray measurement, we first drew a vertical line (line a) laterally to the knee joint, and then found the nearest point to line a (point A) in the lateral edge of the femoral condyle. We then drew a line segment AB perpendicular to line a, which had a crossover point B with the medial edge of the femoral condyle. The line segment AB was divided into 10 equal parts by nine points (points 1-9). Two vertical lines (CD and EF) were drawn separately from points 2 and 8, and had four crossover points (points C, D, E, and F), with a bottom margin of the femoral condyle and top margin of the tibia plateau in the lateral and medial compartments, respectively (Figure 1).
Rd was defined as the ratio of the length of line segment EF to that of line segment CD (Figure 1).
Clinical evaluation
Clinical evaluation was performed using the visual analog pain scale (VAS) and the Knee Society Score (KSS). For each patient, VAS scores were obtained preoperatively and at 48 h postoperatively, while the KSS was obtained preoperatively and when the patient was followed up.
The KSS, which is one of the most frequently used measures in knee orthopedics, is subdivided into three scores: the KSS pain score (KPS), the KSS knee score (KKS), and the KSS functional score (KFS) [8]. The KPS rates pain only. The KKS rates pain, stability, and range of motion, allotting a maximum of 100 points to a well-aligned knee with no pain, 125° of flexion, and negligible AP and mediolateral instability. The KFS rates a patient’s ability to walk and climb stairs, with a maximum score of 100 points attained by walking an unlimited distance without aids and climbing stairs without using a handrail [8].
We also retrieved and compared data on operation time, blood loss, and length of hospitalization between the FSO group and 17 patients who had undergone TKA during the same time period.
Statistical Methods
All statistical analyses were performed using SPSS for Windows (Version 13.0; SPSS, Chicago, IL, USA) and p values <0.05 were considered significant. Values of Rd, VAS, KPS, KKS, and KFS were compared before and after FSO using a paired t-test. Values of operation time, blood loss, and length of hospitalization were compared between FSO and TKA using a one-sample t-test.
Results
Rd showed a non-significant increase from a mean ± standard deviation of 0.32 ± 0.27 preoperatively to 0.50 ± 0.15 after FSO (p=0.056). At postoperative 48 h, VAS scores were significantly decreased and, as patients were followed, the values of KPS, KKS, and KFS significantly increased (Table 2).
| Scale | Pre-FSO | Post-FSO | p-value |
|---|---|---|---|
| VAS | 7.72±0.44 | 1.89±0.78* | 0.000 |
| KPS | 7.78±6.67 | 46.11±2.21 | 0.000 |
| KKS | 57.78±6.67 | 96.11±2.21 | 0.000 |
| KFS | 21.11±7.41 | 55.00±16.58 | 0.001 |
Table 2: Clinical evaluation outcomes following FSO, FSO- Fibular shaft osteotomy; KFS- Knee Society functional score; KKS- Knee Society knee score; KPS- Knee Society pain score; VAS- visual analog pain scale, *Obtained at 48 h postoperatively; Values are mean ± standard deviation.
Operation time and length of hospitalization were significantly shorter with FSO compared with TKA, and blood loss was significantly lower with FSO (Table 3).
| Variable | FSO | TKA | p-value |
|---|---|---|---|
| Operation time (min) | 55.3±14.0 | 131.3±36.0 | 0.000 |
| Blood loss (ml) | 16.0±14.0 | 122.22±56.96 | 0.000 |
| Length of hospitalization (d) | 5.76±2.42 | 11.72±2.59 | 0.000 |
Table 3: Comparison of operation time, blood loss, and length of hospitalization between FSO and TKA, FSO- fibular shaft osteotomy; TKA- total knee arthroplasty, Values are mean ± standard deviation.
Discussion
FSO, once only one of several steps performed during lateral closing-wedge high tibial osteotomy for management of the varus knee [9], has not previously been reported as a method of treating isolated FT medial OA of the knee. The aim of this study was to demonstrate the use of FSO alone for relatively younger patients with isolated medial unicompartmental knee OA. The technique was evaluated by X-ray analysis, VAS, and KSS. The primary findings of this study were: (a) on X-ray evaluation, the ratio of the width of the medial interval to that of the lateral interval was found to be significantly higher after FSO; and (b) patients experienced significant improvements in KSS and VAS scores after FSO. This study represents a preliminary evaluation of FSO for isolated FT medial OA of the knee.
The most important finding of our study is that, during a short-term follow up, FSO could effectively alleviate a patient’s knee pain and enhance quality of life. Interestingly, patients reported significantly decreased VAS scores for knee pain at 48 h postoperatively; that is to say, FSO almost instantly relieved knee pain. Why might this surgical technique achieve instant pain relief? This question drove us to take changes of alignment into consideration because, to the best of our knowledge, mechanical changes might induce instant effects. We hypothesized the following.
As we know, in the human body, the fibula is not a completely degenerative tissue because it can still bear at least one-sixth of our body weight [10,11]. According to the theory of force reaction, this one-sixth of body weight (W1/6) can be reversely conducted along the fibula, from the lateral ankle to the proximal TF joint.
The proximal TF joint is divided into two types according to the angle α, which is between the surface of the proximal TF joint and the horizontal line. In type I, the inclined type, α is less than 20°; in type II, the horizontal type, α is more than 20° (Figure 2) [12]. At the joint surface, according to the parallelogram law, W1/6 should decompose into two forces: one parallel to the surface and the other perpendicular to the surface (Figure 2). Furthermore, the force perpendicular to the surface can also decompose into two forces: one perpendicular to the horizontal line and the other parallel to the horizontal line (Fp) (Figure 2).
Figure 2: Schematic diagram of possible cause of degeneration of the medial compartment in an AP view of a Kellgren–Lawrence grade 3 knee before operation. A, the angle α is between the surface of the proximal TF joint and the horizontal line; B, W1/6 should decompose into two forces; C, one force can also decompose into Fp; D, Fa can decompose into Fpʹ, which might be a balancing force against Fp, and Fq, which might be a cause of degeneration.
The force perpendicular to the horizontal line can be balanced by force from above. To balance Fp, the body might have to make some changes in alignment, one of which might be knee varus. Through knee varus, a force might be created from the articular surface of the femoral medial condyle to that of medial tibial plateau (Fa), which is commonly directed laterodistally. Fa can decompose into Fpʹ, which might be a balancing force against Fp, and Fq, which might be a cause of degeneration (Figure 2). In our study, Fp might have diminished instantly after FSO, with Fpʹ and Fq diminishing at the same time. This, in turn, might have caused the alleviation of the patients’ pain.
The other advantage of FSO, as compared with TKA, is its minimally invasive property. In this study, we compared the operation time, blood loss, and length of hospitalization between FSO and TKA. Our data revealed that, compared with TKA, FSO significantly decreased each of these variables, indicating that FSO is a more tolerable surgery for relatively younger patients. Although the longterm outcomes following FSO are currently unknown, patients receiving FSO can still undergo TKA, and FSO might be helpful in postponing this surgery.
This study had limitations. First, the follow up was short term. Second, we did not record comparative data between FSO and other surgical techniques, such as TKA, unicompartmental arthroplasty, and high tibial osteotomy. Third, the number of patients was limited. Fourth, this was a single-center study; multicenter randomized controlled trials should be considered for future studies. Finally, the hypothesis described above should be verified by biomechanical and finite analyses.
Nevertheless, this is the first clinical study to investigate short-term outcomes following FSO for the treatment of isolated FT medial OA. Results from the 4.5-month follow up lead us to conclude that FSO is effective and more tolerable than more invasive techniques. The use of FSO might be one step of staircase therapy for knee osteoarthritis. Additional investigations need to be performed to further evaluate this technique.
References
- Gomoll AH (2011) High tibial osteotomy for the treatment of unicompartmental knee osteoarthritis: a review of the literature, indications, and technique. Phys Sportsmed 39: 45-54.
- Dettoni F, Bonasia DE, Castoldi F, Bruzzone M, Blonna D, et al. (2010) High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J 30: 131-140.
- Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM (2002) Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am 84: 2235-2239.
- Rossi R, Bonasia DE, Amendola A (2011) The role of high tibial osteotomy in the varus knee. J Am Acad Orthop Surg 19: 590-599.
- Stukenborg-Colsman C, Wirth CJ, Lazovic D, Wefer A (2001) High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-year follow-up prospective randomised study. Knee 8: 187-194.
- Lee KM, Chang CB, Park MS, Kang SB, Kim TK, et al. (2015) Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthritis Cartilage 23: 232-238.
- Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthritis. Ann Rheum Dis 16: 494-502.
- Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248: 13-14.
- Uquillas C, Rossy W, Nathasingh CK, Strauss E, Jazrawi L, et al. (2014) Osteotomies about the knee: AAOS exhibit selection. J Bone Joint Surg Am 96: 199.
- Lambert KL (1971) The weight-bearing function of the fibula. A strain gauge study. J Bone Joint Surg Am 53: 507-513.
- Yun L, Dongcai L, Xijing H (2001) Finite element analysis on crural bone stress changes after partial fibulectomy. Chin J Sport Med 20: 41-42.
- Ogden JA (1974) The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 101: 186-191.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi