Case Report, Clin Oncol Case Rep Vol: 2 Issue: 1
Squamous Cell Carcinoma of the Esophagus after Adalimumab Treatment for Psoriatic Arthritis from Human Papillomavirus Activation
Suraj Sulhan1, Vani Konda2, Shannon Kelley3, Estrellita Ontiveros1 and Steven G Leeds1*
1Department of Minimally Invasive Surgery, Baylor University Medical Center at Dallas, Texas, USA
2Department of Gastroenterology, Center for Esophageal Diseases, Baylor University Medical Center at Dallas, Texas, USA
3Department of Pathology, Baylor University Medical Center at Dallas, Texas, USA
*Corresponding Author : Dr. Steven G. Leeds
Department of Surgery, Baylor University Medical Center at Dallas 3500 Gaston Avenue, 1st Floor Roberts Hospital, Dallas, TX 75246, Texas, USA
Tel: 214-820-0962
Fax: 214-820-4538
E-mail: Steven.Leeds@BSWHealth.org
Received: April 03, 2018 Accepted: February 06, 2019 Published: February 13, 2019
Citation: Sulhan S, Konda V, Kelley S, Ontiveros E, Leeds SG (2019) Squamous Cell Carcinoma of the Esophagus after Adalimumab Treatment for Psoriatic Arthritis from Human Papillomavirus Activation. Clin Oncol Case Rep 2:1.
Abstract
Background: Human Papillomavirus (HPV) is a risk factor that can lead to the development of squamous dysplastic changes and squamous cell carcinoma in patients with coexisting immunosuppression. Such altered immune systems are seen in patients receiving anti-tumor necrosis factor agents for the treatment of various rheumatological disorders. Case presentation: Here we present the case of a 39-year-old female, non-drinker, non-smoker, with the diagnosis of psoriatic arthritis, who presented with new onset dysphagia. Her evaluation showed evidence of pan-esophageal high grade squamous dysplasia. The patient failed organ sparing endoscopic intervention with radiofrequency ablation and cryoablation warranting a near total esophagectomy. Conclusion: In an otherwise low risk patient, this extensive and aggressive esophageal squamous neoplasm is presumed to be from HPV activation following adalimumab use. A review of the literature yielded reports of malignancy following anti- TNF treatment but to our knowledge this is the first reported case of extensive pan esophageal squamous neoplastic in the setting of HPV activation and anti-TNF therapy.
Keywords: Esophageal squamous dysplasia; Adalimumab; Humira; Anti-TNF inhibitor; HPV squamous cell carcinoma
Introduction
Esophageal carcinoma is the sixth most common cause of death due to cancer and the eighth most common cancer overall [1-14]. This includes both esophageal adenocarcinoma and squamous cell carcinoma (SCC). However, the incidence of esophageal adenocarcinoma is rising in developed countries, while SCC is still the most common worldwide. Risk factors for esophageal SCC include tobacco use, alcohol consumption, environmental factors, and infectious pathogenic organisms such as Human Papillomavirus (HPV) [10,11]. Anti-TNF agents have been incredibly effective in managing disorders such as psoriatic arthritis or severe rheumatoid arthritis. There has been investigation into whether anti-TNF agents lead to a higher risk of certain malignancies, including SCC. Here we present a case of a patient treated with adalimumab for psoriatic arthritis activating HPV to cause pan-esophageal multifocal squamous neoplasia [5].
Case Presentation
A 39-year-old non-drinking and non-smoking female with a history of psoriatic arthritis on adalimumab therapy presented with dysphagia to pills. Originally, she had presented with a 3-year history of fatigue and malaise with accompanying foot pains and alopecia. After she was diagnosed with psoriatic arthritis, she was treated with Plaque nil and Azulfadine with little to no symptomatic relief. Subsequent treatment with adalimumab led to a dramatic resolution of her symptoms. She had been on adalimumab for two years with control of her rheumatologic symptoms prior to having dysphagia.
Initial Esophagogastroduodenoscopy (EGD) reported esophagitis and biopsies demonstrated a concern for squamous cell dysplasia. A second endoscopy also found esophagitis with biopsies showing atypical squamous epithelium suspicious for dysplasia. She was referred to a tertiary care referral center. Endoscopy with mapping biopsies demonstrated squamous high grade dysplasia at all levels of the esophagus with foci concerning for intramucosal carcinoma. On one biopsy in the mid esophagus, the pathologist noted a large amount of dysplastic nests that were worrisome for lamina propria invasion. Endoscopic ultrasound was performed and no masses or changes were noted demonstrating progressive disease. Laryngeal and pharyngeal biopsies did not show any abnormality similar to the adjacent squamous epithelium in the esophagus. A CT scan demonstrated no evidence for masses or metastatic disease.
She underwent circumferential balloon radio-frequency ablation (RFA) in an attempt to eradicate the multifocal esophageal squamous dysplasia. She persisted with multifocal dysplasia and went on to have three sessions of cry therapy throughout the esophagus with spray based liquid nitrogen without clearance of the dysplasia.
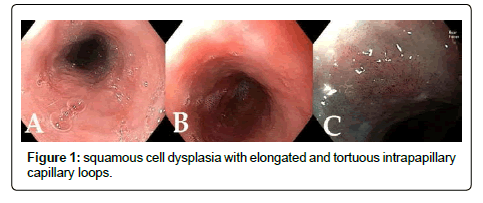
Because she failed endoscopic management, she was referred for surgical consultation and an esophagectomy was recommended prompting her to seek a second opinion. She sought out our institution and underwent repeat endoscopic evaluation to map her disease because it was 3 months since her last endoscopy. The patient had an iodine allergy, so Lugol’s solution, a standard agent for chromo endoscopy for the detection of squamous cell neoplasia, could not be used. Instead, narrow band imaging with near focus was utilized to detect surface abnormalities unapparent on white light endoscopy (Figure 1). Both targeted biopsies of irregular areas and random biopsies demonstrated multifocal high grade dysplasia and the esophageal tissue was positive for high risk HPV.
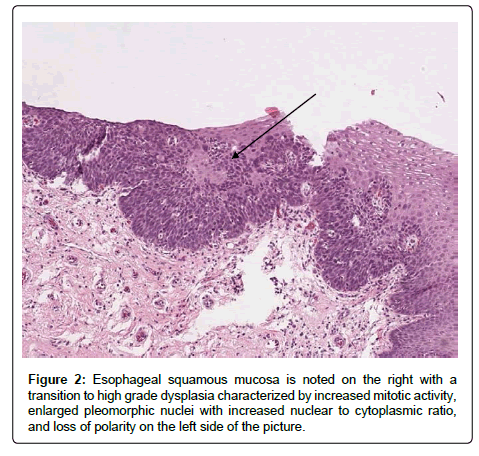
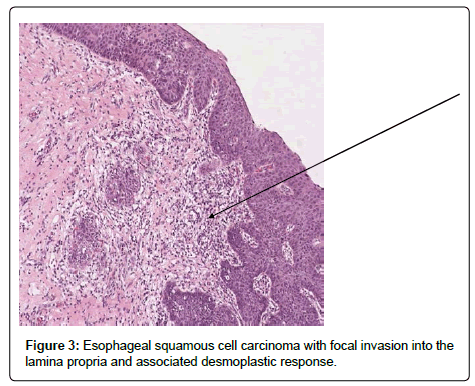
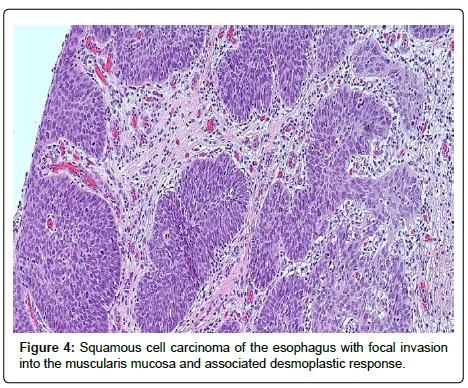
Her case was presented at a multi-disciplinary conference for esophageal diseases and gastrointestinal tumors. Options discussed included continued endoscopic therapy and surveillance, esophagectomy, and radiation therapy and chemotherapy options. Given the multifocal disease and history of failing to respond to endoscopic therapies, the consensus was for an esophagectomy as definitive therapy, and surveillance to the proximal remaining esophageal mucosa left behind to avoid a laryngectomy. It was also decided that if a finding of invasive cancer in the remaining esophageal mucosa should occur, it would prompt radiation or chemotherapy consideration. A repeat round of radiofrequency ablation was performed prior to surgery in the proximal esophagus in order to attempt to clear any dysplasia in the intended area of the anastomosis and allowed to heal. The patient was taken for a minimally invasive three field near total esophagectomy. Pathology of the surgical specimen revealed multifocal high grade dysplasia (Figure 2) and multifocal esophageal squamous cell carcinoma with focal invasion of the muscular is mucosa with associated desmoplastic response (Figures 3 and 4).
The patient was discharged home with an uneventful hospital course following esophagectomy. She was enrolled in an aggressive endoscopic surveillance and treatment plan. Thus far, she has had multifocal low grade dysplasia and one foci of high grade dysplasia at 8 months following surgical resection in the remaining proximal esophageal mucosa. This area of the residual cuff has been treated with radiofrequency ablation, cry therapy using the cry balloon with nitrous oxide, and argon plasma coagulation. She will continue to receive aggressive endoscopic treatment and surveillance for any residual or recurrent dysplasia.
Discussion
Here we report a case of a rare finding of pan-esophageal high grade squamous dysplasia confined to the esophageal mucosa presumed to be from HPV activation related to adalimumab use. The patient had at least 2 years of adalimumab treatment prior to symptoms followed by an atypical, aggressive disease course on presentation. Following surgical resection with near total esophagectomy, the specimen had foci of invasive cancer surrounded by high grade dysplasia. This patient had failed endoscopic intervention with RFA and cry ablation as organ sparing modalities, but will now rely on endoscopic surveillance for the small remaining portion of proximal esophageal mucosa immediately distal to the larynx at the upper esophageal sphincter.
HPV has been shown to be a predisposing factor to the development of squamous dysplasia and carcinoma of the esophagus in patients, especially in a setting of coexisting immunosuppression [12,13]. An altered immune response may potentiate dysplastic development especially in underlying chronic inflammation that may persist in the mucosal lining of the esophagus [14,15]. Such altered immune responses may be seen with the use of anti-TNF agents such as adalimumab and infliximab. TNF-α is a crucial proinflammatory cytokine that promotes migration and activity of T cells in many inflammatory disorders [16-18]. Inhibition of TNF-α could theoretically lead to decreased CD8+ T cells and a subsequent decrease in tumor cell apoptosis which may encourage carcinogenesis. [18].
Although there are no documented cases of esophageal invasive squamous cell cancer due to anti-TNF agents, the closest analogous organ is the oropharynx squamous epithelium which has been reported. In general, most squamous cell carcinomas of the oropharynx begin as noninvasive lesions that slowly progress from hyperplastic epithelial changes to dysplastic carcinoma in situ and culminating as an invasive disease [9]. Various risk factors play a role in the development and maintenance of these lesions including HPV, a virus that has been associated with various dysplastic changes in the oral cavity, pharynx, larynx and even esophagus [9,14]. Multiple reports in the literature have described squamous cell carcinoma of the oropharynx arising in patients receiving anti-TNF agents for treatment of rheumatoid arthritis, ankylosing spondylitis, psoriasis, and psoriatic arthritis [1,3,7,18]. A case of papillary thyroid cancer in a psoriasis patient [8]. However, in a meta-analysis involving 5,014 patients, Bongartz et al. [2] showed an increased risk of malignancies, including squamous cell carcinoma, in those with rheumatoid arthritis receiving infliximab or adalimumab (0.8%) compared with those who received a placebo (0.2%), with a pooled odds ratio of 3.3 (95% CI, 1.2 to 9.1). In regards to malignancies arising from existing HPV infection, trials have suggested a relationship may exist between treatment-induced immunosuppression and cancer development [17]. Probably the most documented case of this conversion is demonstrated in cervical neoplasia. A nationwide register-based cohort study in Sweden showed a double risk of invasive cervical cancer (HR 2.10; 95% CI, 1.04 to 4.23) compared to those not receiving anti-TNF treatment [16].
Current recommendations only recommend screening for skin malignancies before and during treatment with anti-TNF agents [5]. But there are no current recommendations for screening or surveillance of other areas of squamous epithelium with the same use of these agents. Given the rare instance of a malignancy arising from anti-TNF agent use, it would be difficult to recommend that all patients should undergo multiple screening procedures including endoscopy. However, we recommend there should be some consideration for those patients at higher risk for conversion to warrant screening for aero digestive and/or cervical malignancy. Possible high risk groups may include, but are not limited to, patients with high risk HPV infection, documented history of squamous dysplasia in the aero-digestive tract, or smokers. Additionally, patients on anti-TNF therapy should be observed for new symptoms so that appropriate prompt evaluation may be pursued.
Conclusion
To our knowledge, this is the first reported case of esophageal activation of HPV from anti-TNF agents causing a squamous cell carcinoma. This presentation of HPV positive esophageal squamous cell neoplasia is unique and is enhanced by the altered immune state from the anti-TNF therapy. We recommend a heightened awareness of changes in symptoms, or new onset symptoms, in patients while on anti-TNF agents that may warrant prompt upper endoscopy to detect a similar lesion.
References
- Beattie A, Stassen LF, Ekanayake K (2015) Oral Squamous cell carcinoma presenting in a patient receiving adalimumab for rheumatoid arthritis. J Oral Maxillofac Surg 73: 2136-2141.
- Bongartz T, Sutton AJ, Sweeting MJ, Buchan I, Matteson EL (2006) Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. Jama 295: 2275-2285.
- Chainani-Wu N, Chang C, Gross AJ, Yom SS, Silverman S (2014) Oropharyngeal carcinoma arising after methotrexate and etanercept therapy for rheumatoid arthritis. Oral Surg Oral Med Oral Pathol Oral Radiol 117: 261-263.
- Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J cancer 136: 359-386.
- Furst DE, Keystone EC, Braun J, Breedveld FC, Burmester GR (2012) Updated consensus statement on biological agents for the treatment of rheumatic diseases, 2011. Ann Rheum Dis 71 Suppl 2: 12-45.
- Iriki H, Tanese K, Furuichi Y, Takeshita K, Saito M (2016) Marked decrease in serum squamous cell carcinoma antigen level after antitumor necrosis factor alpha therapy in six cases of severe psoriasis. Int J Dermatol 55: 364-366.
- Leao JC, Duarte A, Gueiros LA, Carvalho AA, Barrett AW (2005) Severe oral epithelial dysplasia in a patient receiving adalimumab therapy. J Oral Pathol Med 34: 447-448.
- Lee JJ, Mann JA, Blauvelt A (2011) Papillary thyroid carcinoma in a patient with severe psoriasis receiving adalimumab. J Am Acad Dermatol 64: 999-1000.
- Mehrotra R, Yadav S (2006) Oral squamous cell carcinoma: etiology, pathogenesis and prognostic value of genomic alterations. Ind J cancer 43: 60-66.
- Pastrez PRA, Mariano VS, Costa AM, Silva EM, Scapulatempo-Neto C, (2017) The relation of HPV infection and expression of p53 and p16 proteins in esophageal squamous cells carcinoma. J Cancer 8: 1062-1070.
- Petrick JL, Wyss AB, Butler AM, Cummings C, Sun X (2014) Prevalence of human papillomavirus among oesophageal squamous cell carcinoma cases: systematic review and meta-analysis. Br J Cancer 110: 2369-2377.
- Shimizu M, Ban S, Odze RD (2007) Squamous dysplasia and other precursor lesions related to esophageal squamous cell carcinoma. Gastroenterol Clin North Am 36: 797-811.
- Solomon DH, Mercer E, Kavanaugh A (2012) Observational studies on the risk of cancer associated with tumor necrosis factor inhibitors in rheumatoid arthritis: a review of their methodologies and results. Arthritis Rheum 64: 21-32.
- Tiftikci A, Kutsal E, Altiok E, Ince U, Cicek B (2017) Analyzing esophageal squamous cell papillomas for the presence of human papilloma virus. Turk J Gastroenterol 28: 176-178.
- Verma M, Erwin S, Abedi V, Hontecillas R, Hoops S (2017) Modeling the mechanisms by which HIV-associated immunosuppression influences HPV persistence at the oral mucosa. PLoS One 12.
- Wadstrom H, Frisell T, Sparen P, Askling J, group As (2016) Do RA or TNF inhibitors increase the risk of cervical neoplasia or of recurrence of previous neoplasia? A nationwide study from Sweden. Ann Rheum Dis 75: 1272-1278.
- Werberich GM, Strava T, Vizioli C, Fernandes GDS (2017) Human papillomavirus-induced cancer: late relapse in a patient treated with tumor necrosis factor-alpha inhibitor. J Glob Oncol 3: 275-277.
- Zitelli KB, Zedek D, Ranganathan P, Amerson EH (2013) Squamous cell carcinoma of the lip associated with adalimumab therapy for ankylosing spondylitis: a case report and review of TNF-alpha inhibitors and cutaneous carcinoma risk. Cutis 92: 35-39.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi