Case Report, Clin Oncol Case Rep Vol: 6 Issue: 7
Squamous Cell Carcinoma with Verrucous Features of the Tongue: A Case Report
Jihane Chouef 1*, Lamiae Amaadrour 1 , Hajar Medyouni 1 , Oumaima Siyouri 1 , Oumaima Talbi 1 , Khadija Hinaje 1 , Samia Mhirech2 , Samia Elhakym 1 , Mohamed Sinaa3 , Karima Oualla 1 , Zineb Benbrahim1 , Samia Arifi 1, Nawfel Mellas1
1Department of Medical Oncology, Hassan II University Hospital, Fez, Morocco.
2Department of Radiotherapy, Hassan II University Hospital, Fez, Morocco.
3Department of Pathological Anatomy, Moulay Ismaïl military hospital, Meknes, Morocco
*Corresponding Author: Jihane Chouef
Department of Medical Oncology
Hassan II University Hospital, Fez, Morocco.
E-mail: drchouefjihane@gmail.com
Received: July 13, 2023; Manuscript No: COCR-23-106200;
Editor Assigned: July 14, 2023; PreQC Id: COCR-23-1062009 (PQ);
Reviewed: July 20, 2023; QC No: COCR-23-106200 (Q);
Revised: July 22, 2023; Manuscript No: COCR-23-106200 (R);
Published: July 28, 2023; DOI: 10.4172/cocr.6(7).300
Citation: Chouef J, Amaadrour L, Medyouni H, Siyouri O, Talbi O, et al. (2023) Squamous Cell Carcinoma with Verrucous Features of the Tongue: A Case Report. Clin Oncol Case Rep 6:7
Abstract
Squamous cell carcinomas with verrucous features of the tongue are rare and distinct tumors that arise from the mucosa of the tongue. They are often associated with smoking and alcohol use, but can also occur in patients with no history of tobacco or alcohol consumption. This type of cancer is considered a subtype of squamous cell carcinoma, but has distinct characteristics that differentiate it from other forms of squamous cell carcinomas. Several treatment options are available, but there is no consensus on the best approach. We report a case of squamous cell carcinoma with verrucous features of the tongue in a 68-year-old patient and study the peculiarities of managing this type of lesion. Our patient underwent an MRI and biopsy confirming the histological type of the lesion. Surgical intervention was not feasible due to the size of the tumor, so we opted for a systemic neoadjuvant treatment with methotrexate followed by radiotherapy.
Keywords: Verrucous carcinoma; Squamous cell carcinoma; Methotrexate; Neoadjuvant treatment; Radiotherapy
Introduction
Verrucous carcinoma is a rare malignant tumor of the oral cavity that often develops from the oral mucosa and is characterized by slow growth and local infiltration. It is a rare and aggressive variant of squamous cell carcinoma of the tongue. Although it can develop in people of all ages, it is more common in men over 50 years old. It was first described by Ackerman in 1948 [1]. The pathogenesis of oral verrucous carcinoma is debated [2]. Chronic inflammatory lesions such as old lichen planus and post-lichen planus state could progress to verrucous carcinoma [3]. The standard treatment for verrucous carcinoma of the tongue is surgery with sufficient safety margin, followed by radiotherapy if necessary. However, some patients may not be able to undergo surgery due to the location of the tumor, age, or presence of comorbidities.
Case Presentation
In such cases, neoadjuvant treatment with chemotherapy followed by radiotherapy may be considered. This article examines the efficacy of this treatment in verrucous carcinoma of the tongue. Clinical presentation we report here the case of a 68-year-old female patient, with no notable pathological history, who presented to our clinic with whitish budding lesions throughout the entire right half of her tongue (Figures 1 A and B). A biopsy was performed and a histological examination revealed a microinvasive verrucous carcinoma (Figure 2).
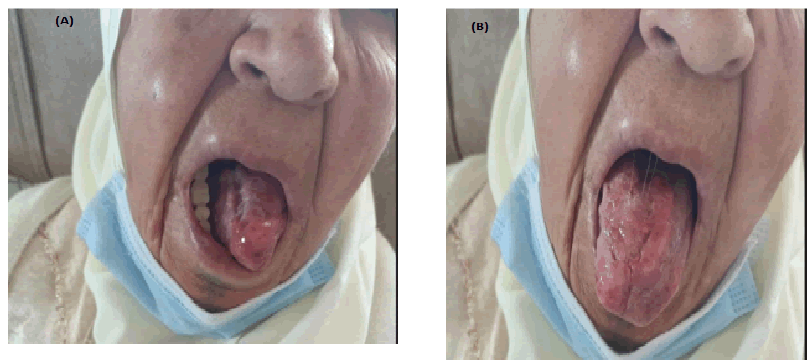
Figure 1 A and B: Clinical appearance of verrucous carcinoma of the tongue.
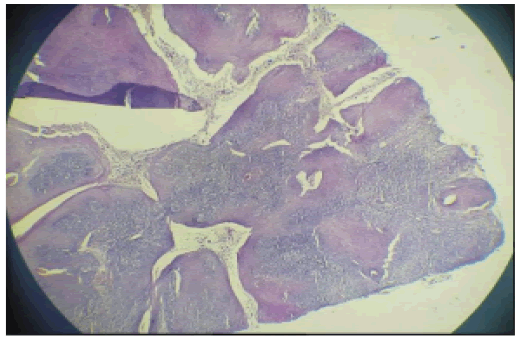
Figure 2: Histological aspect of microinvasive verrucous carcinoma of the tongue.
The MRI revealed the presence of a tumoral process at the free edge of the mid and paramedian right hemi-tongue, measuring 40*20 mm, invading the midline of the tongue, and accompanied by subcentimeter bilateral submandibular and right high jugulo-carotid lymph nodes measuring 15*12 mm (Figure 3). The cervical CT scan had confirmed the presence of multiple bilateral jugulo-carotid adenopathies, more numerous on the left, with the largest measuring 15*12 mm (Figure 4).
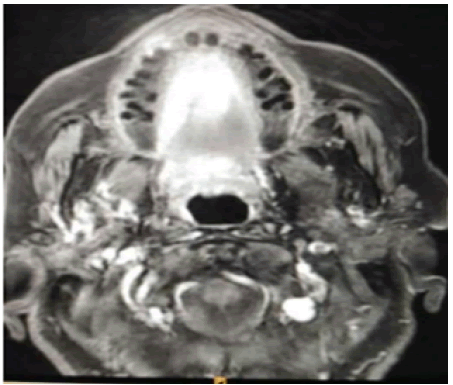
Figure 3: MRI slice showing the lingual lesion.
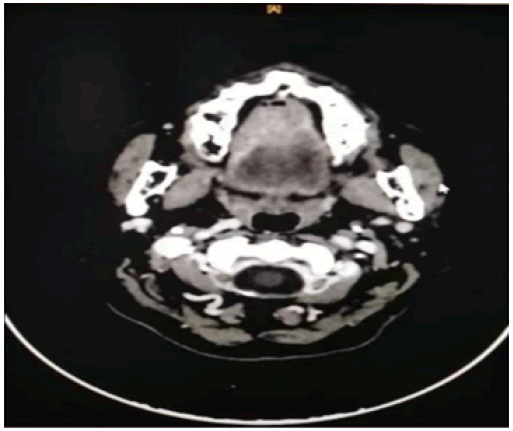
Figure 4: The cervical CT scan showing the multiple bilateral jugulo-carotid adenopathies.
The decision was made to treat the patient with neoadjuvant therapy using weekly methotrexate at a dose of 30 mg/m2 for 2 months, followed by radiotherapy. There was a clear regression of the lesion after the first 3 cycles of treatment (Figure 3), which encouraged us to continue with the remaining cycles. However, the benefit did not last long as by the 8th cycle, the lesion began to spread and the patient reported difficulty eating. Therefore, it was decided to stop the chemotherapy, perform an evaluation imaging, and start radiotherapy urgently. The MRI showed an increase in the size of the lesion in the right hemi-tongue, measuring 55*20mm, extending to the base of the tongue with doubt of involvement of the floor of the mouth
The patient received conformal radiotherapy with intensity modulation at a dose of 70 Gy in 35 fractions, with a fractionation of 2 Gy per fraction. The side effects were marked by the installation of recurrent mucositis and pain in the right side of the face. The MRI and CT scan performed after the completion of radiotherapy suggested local progression with the appearance of an abscess collection near the lateral border of the tongue,
and at a distance, several suspicious parenchymal and subpleural lung nodules. It was decided to start systemic chemotherapy using carboplatin AUC 2 with paclitaxel. After two months, the patient died in a state of multi-visceral failure.
Discussion
Verrucous carcinoma is a true well-differentiated low-grade cancer, and its clinical and histopathological properties make it a distinct entity. Ackerman identified the oral location of VC from 31 cases in 1948, and since then, over 400 other cases have been reported [1]. Various names have been used.
Oral verrucous carcinoma begins as a well-defined thin white keratotic plaque, which will then thicken and develop a papillomatous surface, with rounded or pointed ends. Some lesions may present as a pink or erythematous mass. The color of the lesion, white-grayish and more or less tinted by an erythematous aspect, depends on the amount of keratosis produced and the degree of inflammatory response to the tumor [4].
Many factors are implicated in the etiopathogenesis of oral verrucous carcinoma, among which smoking is strongly associated with it and has long been proven to have a carcinogenic role, noted in 80 to 90% of cases. Alcohol is not a carcinogen, but its association with smoking intoxication has a synergistic character and leads to a multiplicative effect of risks. The predominant responsibility of the alcohol-tobacco pair is demonstrated by important epidemiological studies. Poor oral hygiene and low socioeconomic status are associated with oral verrucous carcinoma [5,6].
Rajendran records the association of leukoplakia and verrucous carcinoma in 48% of his patients. The occurrence on lichen planus may seem classic, but it is rarely found in the literature since Eva Schleicher-Gottron's original description [5, 7].
Histologically, verrucous carcinoma shows both endophytic and exophytic growth patterns, and is a well-differentiated hyperplastic epithelial lesion. The tumor has a densely keratinized (parakeratinized) surface and deep margins that are precisely circumscribed, appearing to push rather than infiltrate the basal membrane (see Figure 4). In the depth, there are wide subepidermal extensions and projections into the underlying dermis formed by tumor masses often filled with keratin. Cytologically, this variant of squamous cell carcinoma appears benign with low mitotic activity and normal cell maturation aspects. There is a chronic inflammatory reaction of mononuclear cells of lymphohistiocytic origin in the edematous stroma immediately adjacent to the margins (Figure 5).
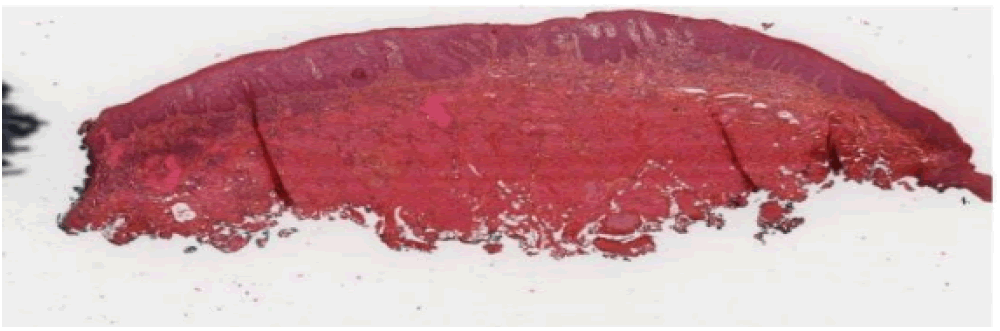
Figure 5: Histological section of a grade 1 verrucous carcinoma of the lateral border of the tongue. H&E staining. Magnification x0.4: An epithelial hyperplasia with a budding appearance can be observed. The basal membrane is continuous.
Therapeutic management is not standardized [8], and surgery remains the treatment of choice [9]. The therapeutic strategy is difficult to specify because it mainly depends on the age and general condition of the patients, as well as the clinical appearance and extent of the lesions. Most therapeutic trials have been conducted on small patient series, and their conclusions are contradictory.
For extensive lesions, eligibility for surgery may be questioned when the lesions are too extensive, complicating post-excision reconstruction. One possible option in the treatment of these large lesions is chemotherapy based on methotrexate. In a case series, Karazoglu et al.110 present the results of treating 12 patients with oral verrucous carcinoma ranging from T2 to T4 [9].
The retrospective study spanning from the 1970s to the 2000s references several protocols due to the evolution of therapies. Of the 12 patients, 7 had a good response to treatment, meaning a regression of the lesion greater than 50%. Of these 7 patients, 4 received intravenous treatment with complementary radiotherapy for one of them and complementary CO2 laser excision for another. The other 3 patients received treatment with intra-muscular injection. The author concludes that the use of methotrexate as first-line treatment does not necessarily avoid secondary excision or radiotherapy
Conclusion
Neoadjuvant treatment with methothrexate followed by radiotherapy may have demonstrated its effectiveness in certain cases in the literature, however this was not the case for our patient. Although this treatment may be effective for other types of cancer, it does not appear to be effective for this rare form of oral cancer. Further studies are needed to determine the most effective treatment options for this difficult-to-treat disease.
References
- Ackerman LV (1948) Verrucous carcinoma of the oral cavity. Surgery 23: 670-678. [Google Scholar] [Cross Ref]
- Wu CF, Chen C, Shen Y, Huang I, Chen C, et al. (2008) Effective eradication of oral verrucouscarcinoma with continuous intraarterial infusion chemotherapy. Head Neck 30: 6117. [Google Scholar] [Cross Ref]
- Warshaw EM, Templeton SF, Washington CV (2000) Verrucous carcinoma occurring in a lesion of oral lichen planus. Cutis 65: 219-222. [Google Scholar] [Cross Ref]
- Verrucous carcinoma of the oral cavity
- Rajendran R, Sugathan C, Augustine J, Vasudevan D, Vijayakumar T (1989) Ackerman’s tumour (Verrucous carcinoma) of the oral cavity: A histopathologic study of 426 cases. Singapore Dent J 14: 48-53. [Google Scholar] [Cross Ref]
- Shear M, Pindborg J (1980) Verrucous hyperplasia of the oral mucosa. Cancer 46: 1855-1862. [Google Scholar] [Cross Ref]
- Tomb R, Grosshans E. (2001) The rediscovery of previously described dermatoses. Arch Dermatol 137: 715-718. [Google Scholar] [Cross Ref]
- Tomb R, El-Hajj H, Nehme E, Haddad A (2003) Carcinome verruqueux de la langue survenu sur des lésions de lichen plan. Annales Dermatol Venereol 130: 55-57. [Google Scholar] [Cross Ref]
- Miller CS, Johnstone BM (2001) Human papillomavirus as a risk factor for oral squamous cell carcinoma: A meta-analysis, 1982-1997. Oral Surg, Oral Med, Oral Path, Oral Radiol, Endodontol 91: 622-635. [Google Scholar] [Cross Ref]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 