Case Report, Clin Dermatol Res J Vol: 8 Issue: 4
Subacute Necrotizing Fasciitis: A Case and Review of Diagnostic Criteria
Nam H Vo*
Department of Osteopathic Medicine, William Carey University, Houston, United States
*Corresponding Author:
Nam H Vo
Department of Osteopathic Medicine,
William Carey University,
Houston,
United States;
E-mail: Nvo346141@gmail.com
Received date: 14 August, 2019, Manuscript No. CDRJ-23-103296;
Editor assigned date: 19 August, 2019, PreQC No. CDRJ-23-103296 (PQ);
Reviewed date: 02 September, 2019, QC No. CDRJ-23-103296;
Revised date: 14 June, 2023, Manuscript No. CDRJ-23-103296 (R);
Published date: 12 July, 2023, DOI: 10. 4172/2576-1439.1000210
Citation: Vo NH (2023) Subacute Necrotizing Fasciitis: A Case and Review of Diagnostic Criteria. Clin Dermatol Res J 8:3.
Abstract
Subacute necrotizing fasciitis is an under-recognized form of necrotizing fasciitis with an indolent course, but rapid deterioration. Early recognition is challenging due to the seemingly benign clinical presentation. If left untreated, subacute necrotizing fasciitis could rapidly progress with systemic involvement and grave outcomes. There have been a limited number of cases reported likely due to the lack of recognition. Discussion is made on a set of proposed diagnostic criteria for early recognition of subacute necrotizing fasciitis. Surgical debridement or amputation is curative of necrotizing fasciitis
Keywords: Subacute necrotizing fasciitis, Subacute; Fasciitis, Serratia marcescens, Cellulitis
Introduction
Necrotizing Fasciitis (NF) is a chronic inflammatory infection of the fascia that is often aggressive and progresses slowly. NF can be caused by a traumatic event or surgical intervention or it can occur on its own. We present a case of monomicrobial subacute necrotizing fasciitis caused by Serratia marcescens. Dermatology was contacted at the local hospital for probable cellulitis that had not resolved despite treatment with suitable medicines. Our patient did not recover with antibiotic therapy and had to have her leg amputated above the knee. We also included a review of the existing literature on S. marcescens and subacute necrotizing fasciitis [1].
A case of identified just a few cases of lower limb NF caused by S. marcescens, with no following COVID-19. As a result, this is the first report of such a case, which should aid in the clinical management of such patients in the future, particularly with COVID-19 growing prevalent in our communities and contributing to delayed presentations and higher mortality in NF [2].
Subacute necrotizing fasciitis is a clinical entity with little definition. Its very existence has been the source of significant debate. Many writers have documented subacute forms of necrotizing fasciitis in the literature, despite the fact that they are infrequently described.
This paper discusses some recently reported cases in the literature, demonstrating that subacute forms of necrotizing fasciitis do exist and may be under-reported due to a lack of awareness and consistent diagnostic criteria [3].
Necrotizing fasciitis, often known as Necrotizing Soft Tissue Infections (NSTIs), is a rare but deadly condition. They are infections of any of the soft tissue compartment's layers (dermis, subcutaneous tissue, superficial fascia, deep fascia or muscle) that are linked with necrotizing alterations. When it first appears, necrotizing fasciitis can be difficult to distinguish from cellulitis and other superficial skin infections. In reality, approximately 15% to 34% of necrotizing fasciitis patients have an appropriate admitting diagnosis. Early detection and treatment with surgical debridement, antimicrobials and supportive measures lower mortality. Even with current ICU treatment, mortality rates range between 16% and 36%; this is due to diagnostic delays and comorbidities. Various scoring systems have been created to aid in diagnosis and stratification of patients [4].
Serratia marcescens-induced necrotizing fasciitis of the abdominal wall, as well as the findings of a focused review of S. marcescens induced necrotizing fasciitis. Our patient had aorto-femoral bypass grafting for severe peripheral vascular disease and presented three weeks later with pain, erythema and drainage from the incision site in the left lower abdominal wall, which required numerous debridements. Pathology of debrided tissue revealed severe necrosis of adipose tissue, fascia and skeletal muscle. Serratia marcescens was found in wound cultures. Antibiotics and several surgical debridements were used to treat her successfully. Because necrotizing fasciitis is a medical and surgical emergency, it is vital to investigate infectivity trends and clinical features in the causal spectrum [5].
We found 17 reported cases of necrotizing fasciitis caused by Serratia marcescens and then looked for trends among them. Serratia marcescens is common in the community and hospital settings and the information offered in this study on infection presentations, risk factors, features, therapy, course and complications should assist identify cases sooner and prevent unfavourable outcomes. Patients with positive blood cultures and those who did not receive or were delayed in receiving surgical intervention had a higher mortality rate. Surgical intervention is a certain approach to establish necrotizing infection and distinguish it from other entities [6].
Necrotizing Fasciitis (NF), also known as Necrotizing Soft Tissue Infections (NSTIs), is a rare but deadly infection. They are infections of any of the soft tissue compartment's layers (dermis, subcutaneous tissue, superficial fascia, deep fascia or muscle) that are linked with necrotizing alterations. NSTIs are not usually associated with abscesses, but they might develop from an untreated or insufficiently drained abscess. Jones originally documented these diseases in 1871, when they were known as hospital gangrene and had a 46% fatality rate. Shortly after, Jean-Alfred Fournier reported Fournier's Gangrene, a kind of soft tissue infection affecting the male perineal region. This term has lately been modified to include necrotizing infections of the male perineum [7].
Necrotizing Fasciitis (NF) is a rapidly progressive soft tissue infection characterized by widespread fascial necrosis and systemic toxicity. The typical presentation entails severe pain and anesthesia of the affected region, along with constitutive symptoms of fever, hypotension and multi-organ failure. There are a limited number of reports that describe a subacute presentation of NF. Subacute NF lack the aggressive clinical features seen with NF and instead, demonstrates an indolent course followed by sudden, rapid deterioration. Vascular insufficiency, cellulitis, or other soft-tissue infections clinically mimic this condition due to the lack of apparent severity at onset. Definitive treatment includes fasciotomy and debridement in order to prevent limb-loss and death. It is therefore critical to establish accepted criteria to aid in early disease recognition. We describe a case of subacute NF resulting in partial amputation with a discussion of the proposed diagnostic parameters [8].
It is extremely uncommon for Pseudomonas aeruginosa to induce necrotizing fasciitis. In the literature, there were just 4 cases mentioned. The authors describe a case of P. aeruginosa necrotizing fasciitis in a girl who initially had a vulval abscess prior to starting induction chemotherapy for acute lymphoblastic leukaemia. This is the second case associated with leukaemia that has been reported to our knowledge. In this instance, early surgical intervention, which confirmed the diagnosis, contributed to a favourable outcome.
Necrotizing fasciitis is a rare and severe type of subcutaneous gangrene that needs prompt detection and urgent care. We describe the case of a 24-year-old lady who presented with necrotizing fasciitis following unresponsive pansinusitis. Pseudomonas aeruginosa was the microbe found. Intensive care, antibiotics and surgical removal of necrotic tissues were used to control the illness. The purpose of this observation is to draw attention to the clinical features of this illness and to emphasise the importance of spotting early symptoms and beginning treatment as soon as feasible.
Necrotizing fasciitis is a rare bacterial infection that spreads quickly in the body and can cause death. Accurate diagnosis, rapid antibiotic treatment and prompt surgery are important to stopping this infection.
Case Presentation
A 73-year-old female presented to the Emergency Department (ED) with a two-week history of weakness and painful swelling in her bilateral lower extremities. Seven days prior, she sought care at a local outpatient clinic where she was treated for a suspected congestive heart failure exacerbation. At that time, examination of her legs revealed erythema, tenderness to palpation and edema that was worse on the right (Figure 1) [9].
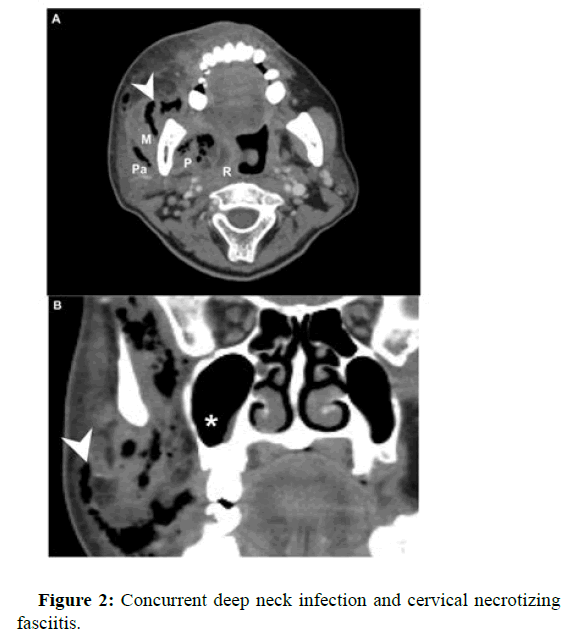
The patient later presented to the ED with erythema, induration and small tense bullae of the right lower leg and foot. Labs on admission demonstrated a white blood cell count of 7.4 × 109/L, a blood glucose level of 65 mg/dL and a lactic acid level of 3.6 mmol/L. She was treated empirically for cellulitis with suspected sepsis. Blood and wound cultures revealed Serratia marcescens, a gram-negative bacillus implicated in wound infections. Despite broad-spectrum antibiotics aztreonam and ceftriaxone her condition continued to deteriorate. Over the course of six days, tense and painful hemorrhagic bullae with significant edema of the dorsum foot developed, extending into the distal phalanges. Induration of the tissue extended beyond apparent erythema (Figure 2) [10].
Dermatology was subsequently consulted and upon examination a diagnosis of necrotizing fasciitis was made. Surgery was immediately consulted and the patient underwent an above the knee amputation of the right lower extremity. No complications were reported at followup.
Results and Discussion
Based on the results of an extensive literature review, Wong proposed a set of diagnostic criteria for subacute NF4:
• Initial indolent course without signs of systemic toxicity.
• Gradual tissue necrosis with possible overlying cutaneous findings.
• Progression despite proper use of anti-microbials.
• Sudden deterioration to NF with septic features.
Our patient demonstrated each of the aforementioned parameters, whereby she experienced a slowly worsening leg pain of two weeks without additional symptoms aside from weakness. She then reported a sudden worsening pain accompanied by the appearance of erythema, induration and bullae of her right lower extremity, prompting her visit to the ED. At presentation, she was tachycardic with laboratory evidence suggestive of possible sepsis. Although appropriate antibiotic therapy was employed, the patient showed no improvement. She ultimately received an above the knee amputation, after which her condition stabilized.
Conclusion
The true incidence of subacute NF is likely misrepresented in the literature. Due to the subtle features and lack of symptomatic severity, the diagnosis of subacute NF is difficult. Furthermore, knowing at what point the clinical decline will occur cannot be predicted. According to Wong et al., the demonstration of NF features occurred as early as six days following the onset of symptoms and as well as longer than a month’s duration. Failure to consider NF as a diagnosis during this indolent period can be detrimental, as early surgical debridement is vital to prevent morbid outcomes.
References
- Jarrett P, Rademaker M, Duffill M (1997) The clinical spectrum of necrotising fasciitis. A review of 15 cases. J Med 27: 29-34.
[Crossref] [Google Scholar] [PubMed]
- Wong CH, Tan SH (2004) Subacute necrotising fasciitis. Lancet 364: 1376.
[Crossref] [Google Scholar] [PubMed]
- Saliba WR, Goldstein LH, Raz R, Mader R, Colodner R, et al. (2003) Subacute necrotizing fasciitis caused by gas-producing Staphylococcus aureus. Eur J Clin Microbiol Infec Dis 22: 612-614.
[Crossref] [Google Scholar] [PubMed]
- Wong CH, Wang YS (2006) What is subacute necrotizing fasciitis? A proposed clinical diagnostic criteria. J Infect 52: 415-419.
[Crossref] [Google Scholar] [PubMed]
- Ahmad H, Haider J, Siddiqui SS, Naz S, Nihal F, et al. (2018) Subacute peristomal necrotizing fasciitis detected during adjuvant chemotherapy for adenocarcinoma rectum: Case report on a unique presentation and description of a simple surgical strategy for treatment. Cureus 10: e2075.
[Crossref] [Google Scholar] [PubMed]
- Puvanendran R, Huey JC, Pasupathy S (2009) Necrotizing fasciitis. Canadian Fam Phys 55: 981-987.
[Google Scholar] [PubMed]
- Wong CH, Wang YS (2005) The diagnosis of necrotizing fasciitis. Curr Opin Infect Dis 18: 101-106.
[Crossref] [Google Scholar] [PubMed]
- Wysoki MG, Santora TA, Shah RM, Friedman AC (1997) Necrotizing fasciitis: CT characteristics. Radiology 203: 859-863.
[Crossref] [Google Scholar] [PubMed]
- Al Shukry S, Ommen J (2013) Necrotizing fasciitis-report of ten cases and review of recent literature. J Med Life 6: 189.
[Google Scholar] [PubMed]
- Lazzeri D, Lazzeri S, Figus M, Tascini C, Bocci G, et al. (2010) Periorbital necrotising fasciitis. Brit J Ophthalmol 94: 1577-1585.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi