Case Report, Clin Oncol Case Rep Vol: 6 Issue: 1
Successful Closure of the Post Tracheostomy Tracheoesophageal Fistula with Sternohyoid Muscle Interposition
Arsheed Hussain Hakeem1*, Hassaan Javaid 2, Hemanth Vudayaraju3, Usaamah Javaid4
1Department of Head and Neck Oncology, Apollo cancer Institute, Hyderabad,Telangana, India
2Department of Trauma Surgery, All India Institute of Medical Sciences, New Delhi,India
3Department of Surgical Oncology, Apollo Cancer Institute, Hyderabad, Telangana, India
4Department of Internal Medicine, Lok Nayak Jai Prakash Narayan Hospital, Jawahar Lal Nehru Marg, Delhi, India.
*Corresponding Author: Arsheed Hussain Hakeem
Department of Head and Neck Oncology
Room No: 10, Apollo Cancer Institute, Jubilee Hills, Hyderabad, Telangana, India 500096.
E-mail: drahhakim@gmail.com
Received: January 10, 2023; Manuscript No: COCR-23-86680;
Editor Assigned: January 12, 2023; PreQC Id: COCR-23-86680 (PQ);
Reviewed: January 22,2023; QC No: COCR-23-86680 (Q);
Revised: January 24, 2023; Manuscript No: COCR-23-86680 (R);
Published: January 30, 2023; DOI: 10.4172/cocr.6(1).271
Citation: Hakeem AH, Javaid H, Vudayaraju H, Javaid U (2023) Successful Closure of the Post Tracheostomy Tracheoesophageal Fistula with Sternohyoid Muscle Interposition. Clin Oncol Case Rep 6:1
Abstract
We report the case in which post tracheostomy tracheoesophageal fistula was successfully managed by primary closure of the tracheal and oesophageal fistula with interposition of a sternohyoid muscle flap. Tracheoesophageal fistula at 20 cm form incisor teeth developed in a 56-year-old male who had tracheostomy as part of the supraglottic laryngectomy. Oesophageal and tracheal defects were dissected out and separately sutured and left inferiorly based sternohyoid muscle flap was interposed between the two suture lines. Satisfactory breathing and swallowing functions were gained after 3 weeks of surgery independent of nasal tube feeding and re-tracheostomy was avoided. Our method is simple and effective technique for successful closure of post tracheostomy tracheooesophageal fistula utilizing location tissues for achieving good results without significant morbidity and it can be practised even in nutritionally low patients.
Keywords: Tracheooesophageal fistula; Sternothyroid muscle; Tracheostomy; Trachea; Oesophagus
Introduction
Post tracheostomy tracheoesophageal fistula is relatively uncommon event and results from the hyperinflation of the tracheostomy tube cuff. It results from the ischemic necrosis of the party wall of membranous tracheal and oesophagus as a result of high pressure of the cuff, often against rigid nasogastric tube. It was only after the case reports of the fistulas due to the cuff of the tracheostomy tube as documented by Flege in 1967 and Hedden et al. in 1969, it became clear that cuffed tubes were the most frequent cause [1,2]. Since spontaneous closure is rare and communication between trachea and oesophagus is a life-threatening condition, consequent to tracheobronchial contamination and aspiration pneumonia, surgical closure of the fistula is mandatory. Surgical closure of the tracheoesophageal fistula is a challenge, despite availability of different options ranging from simple closure to tracheal resection and the major muscle transfers [3]. We report a patient who underwent successful surgical closure of an acquired tracheoesophageal fistula by primary closure and interposition of a sternohyoid muscle flap between trachea and oesophagus.
Case Report on Methods and Operative Technique
56-year-old male was referred to our head and neck surgery department with persistent symptoms of aspiration after 2 months of supraglottic laryngectomy for epiglottic carcinoma. As part of the surgery he was temporarily tracheostomised and nasogastric feeding tube was inserted. He was decannulated after 3 weeks of surgery, but nasogastric tube was continued for 2 months as he had symptoms of aspiration. As the symptoms of aspiration did not improve even after 2 months, after decannulation, an upper gastrointestinal endoscopy was advised which revealed a tracheoesophageal fistula at 20 cm from the incisor teeth (Figure 1A). Positron Emission Tomography/Computed Tomography (PET/CT) scan did not reveal any evidence of the cancer recurrence in the larynx. No symptoms or signs of pulmonary disease was seen despite tracheoesophageal fistula.
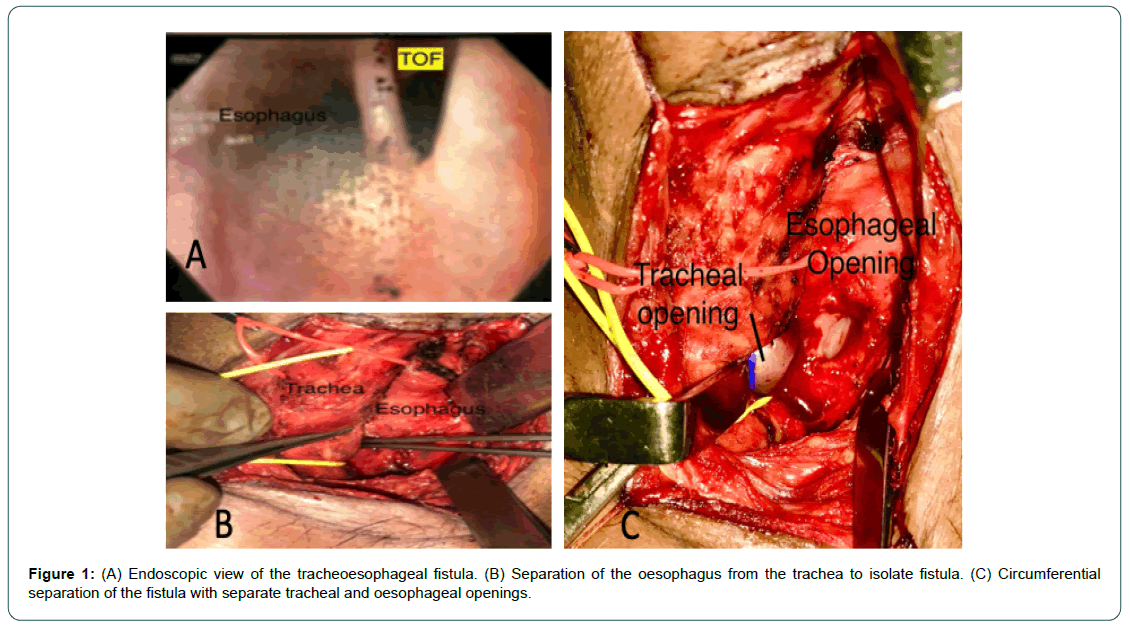
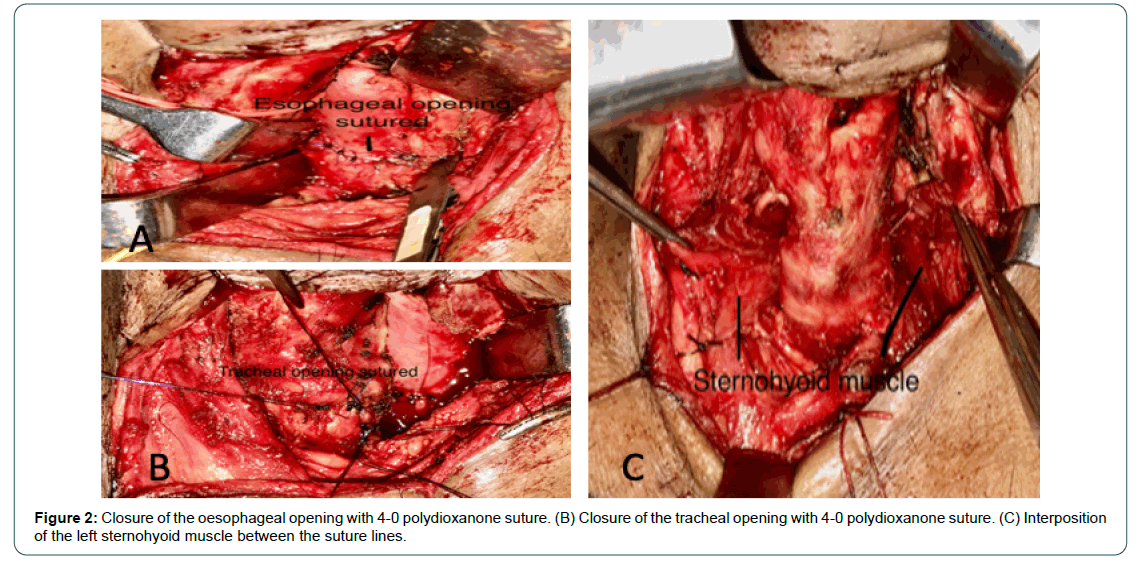
Open surgical closure was planned under general anaesthesia, orotracheal intubation was performed using 6.5 no. endotracheal tube. Smaller tube was used to allow the space for closure of the membranous tracheal wall. Extension position of the neck was given and a transverse skin incision was made about 2 finger breadths above the suprasternal notch. Subplatysmal flap was elevated superiorly up to the hyoid bone and inferiorly up to sternoclavicular joints. Strap muscles were separated in the midline and retracted laterally. Trachea was identified and sharp dissection was done to define the trachea and separate it from the oesophagus (Figure 1B). Tracheoesophageal communication was identified after completely separating the oesophagus from the trachea above and below the fistulous tract. Fistula site was incised and margins refreshed along the circumference (Figure 1C). Oesophageal opening was closed in two layers mucosal and muscular layer with 4-0 polydioxanone interrupted sutures horizontally (Figure 2A). Opening of the membranous wall of the trachea was also closed with 4-0 PDS suture in single layer horizontally (Figure 2B). Sternohyoid muscle on the left side was released from superior attachment and lateral soft tissue attachment and interposed between the trachea and the oesophagus to separate the sutured areas (Figure 2C).
Discussion
Post tracheostomy tracheoesophageal fistula although rare, is a well-known complication of the procedure. The wide spread use of high-volume low-pressure cuffed tracheostomy tubes has drastically reduced the incidence of cuff-related complications like tracheoesophageal fistula. In our case it was documented with an upper gastrointestinal endoscopy, as he continued to aspirate even after 2 months of supraglottic laryngectomy. Endoscopic evaluation was not only useful in the diagnosis, but also helped to determine level of fistula influencing the choice of a cervical rather than a thoracic approach [4]. We opted for dissection close to the tracheal wall till we identified the fistulous track on the both sides and separate trachea and oesophagus above and below the fistula without identifying recurrent laryngeal nerves or ligating inferior thyroid artery or removing thyroid gland or isthmus as advocated by some authors [5].
We prefer to divide the isthmus and retract the isthmus and thyroid lobe laterally from trachea in case it is hindering the isolation of the fistula. Our opinion is that thyroidectomy may be useful only in presence of cervical or cervicomediastinal goitres [6].
Different authors have described different techniques for the closure of the tracheoesophageal fistulas, varying from primary closure of tracheal and oesophageal defects with or without pedicled muscle flap interposition to segmental tracheal resection and anastomosis with oesophageal closure and/or diversion [3,7, 8]. Grillo described standard single stage procedure consisting of tracheal resection and anastomosis with primary oesophageal closure [3]. We chose not to resect trachea as advised by Grillo et al, as in our case there was no tracheal stenosis at all. The oesophageal and tracheal openings were separately closed and sternohyoid muscle was interposed between the two suture lines. Our technique is similar to that described by Pisanu A et al., which is suitable even for patients with poor clinical condition [6]. The interposition of an inferiorly based sternohyoid muscle flap is a simple, quick, and safe procedure with low donor-site morbidity, provided that flap’s n eural a nd a rteriovenous s upply i s properly preserved [9]. The arterial supply of the upper s ternohyoid muscle consistently arises from a branch of the superior thyroid artery [10]. Using an inferiorly based sternohyoid muscle flap has the potential to de-vascularize the muscle, resulting in ischemic atrophy and fibrosis of the flap in about 40% of cases [9]. However the neural and arteriovenous supply of the sternohyoid muscle can be preserved with careful lateral dissection. The knowledge of these anatomic variations together with presence of an un interrupted inferior neurovascular network coming from ansa-cervicalis may be useful for maintaining good postoperative bulk of the flap transported between the tracheal and oesophagus then avoiding close contact of the suture line and preventing dehiscence. On the other hand mainly after thyroid lobectomy and despite gain in trachea oesophageal fistula exposure, the inferior pedicle of the sternohyoid muscle may be damaged, thus compromising even more the muscle viability and increasing the risk of recurrence of ischemic atrophy. In this case, the muscle acts like a graft than flap making use of an inferiorly based sternohyoid muscle flap controversial.
Results and Conclusion
Surgery was successful and the drainage tube was removed after 3 days, the nasogastric tube was removed 2 weeks later. At this point, he was able to accept a liquid diet without coughing. In conclusion our technique of closure of the TOF is simple and effective. It utilises the local available tissue hence minimising morbidity. It can be used in nutritionally low patients as the operating time is less.
Acknowledgments
The research was performed at the Department of Head and Neck surgery, Apollo Cancer Institute, Hyderabad.
Authors Contribution
AHH operated the patient and conceptualized and designed the manuscript. Dr H V helped in surgery and design of the manuscript. HJ did the literature review. All authors reviewed and accepted the manuscript for publication
Conflicting Interest
The authors declare that they have no conflict of interest.
References
- Flege JB Jr (1967) Tracheoesophageal fistula caused by cuffed tracheostomy tube. Ann Surg 166: 153-156. [Google Scholar] [Cross Ref]
- Hedden M, Ersoz CJ, Safar P (1969) Tracheoesophageal fistulas following prolonged artificial ventilation via cuffed tracheostomy tubes. Anesthesiology 31: 281-289. [Google Scholar] [Cross Ref]
- Grillo HC, Monsure AC, McEnany MT (1976) Repair of inflammatory tracheoesophageal fistula. Ann Thorac Surg 22: 112-119. [Google Scholar] [Cross Ref]
- Cherveniakov A, Tzekov C, Grigorov GE, Cherveniakov P (1996) Acquired benign esophago-airway fistulas. Eur J Cardiothorac Surg 10: 713-716. [Google Scholar] [Cross Ref]
- Payne DK, Anderson WM, Romero MD, Wissing DR, Fowler M (1990) Tracheoesophageal fistula formation in intubated patients: Risk factors and treatment with high-frequency jet ventilation. Chest 98: 161-164. [Google Scholar] [Cross Ref]
- Pisanu A, Reccia I, Nieddu R, Uccheddu A (2009) Sternohyoid muscle flap interposition in the treatment of an acquired tracheoesophageal fistula. Head 31: 962-967. [Google Scholar] [Cross Ref]
- Golash V (2006) Single-stage repair of a large acquired tracheoesophageal fistula with interposition of 2 muscle pedicle flaps and laparoscopic gastrojejunostomy. J Thorac Car-diovasc Surg 131: 1413-1414. [Google Scholar] [Cross Ref]
- Wolf M, Yellin A, Talmi YP, Segal E, Faibel M, et al. (2000) Acquired tracheoesophageal fistula in critically ill patients. Ann Otol Rhinol Laryngol 109: 731-735. [Google Scholar] [Cross Ref]
- Wang RC, Puig CM, Brown DJ (1998) Strap muscle neurovascular supply. Laryngoscope 108: 973-976. [Google Scholar] [Cross Ref]
- Bailey BJ (1985) Surgery of the larynx. Philadelphia: WB Saunders 271. [Google Scholar]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 