Research Article, Clin Dermatol Res J Vol: 2 Issue: 1
The Use of 2-Octyl Cyanoacrylate Skin Adhesive for Laceration Repair in the Emergency Department
Wolfe A1, Aten A2 and Schrock JW3*
1Department of Emergency Medicine, Presbyterian St. Luke’s Hospital, Denver Colorado, USA
2Department of Emergency Medicine, Doctors Hospital/Springfield Regional Medical Center, Springfield Ohio, USA
3Department of Emergency Medicine, MetroHealth Medical Center, Case Western Reserve University School of Medicine, Cleveland Ohio, USA
*Corresponding Author : Jon W. Schrock
Department of Emergency Medicine, Metro Health Medical Center, Case Western Reserve University School of Medicine, Cleveland Ohio, USA
Tel: 216-778-5747
Fax: 216-778-5349
E-mail: jschrock@metrohealth.org
Received: April 13, 2017 Accepted: June 16, 2017 Published: June 21, 2017
Citation: Wolfe A, Aten A, Schrock JW (2017) The Use of 2-Octyl Cyanoacrylate Skin Adhesive for Laceration Repair in the Emergency Department. Clin Dermatol Res J 2:1.
Abstract
Objectives: Surgical adhesives are a common Emergency Department (ED) wound closure method. Advantages include
ease of closure, speed of closure, and decreased or elimination of injectable anesthetics. We sought to evaluate the how a new formulation of 2-octyl cyanoacrylate (2OCA) would perform used for closure of lacerations on ED patients presenting with lacerationslooking at post-procedure bleeding, dehiscence, and infection.
Methods: we performed a prospective open-label observational case study in an urban ED. Inclusion criteria included greater than 5 years of age, candidate for use of a topical surgical skin adhesive. Exclusion criteria included known sensitivity to topical tissue adhesive products or degrading products, a history of keloid formation, hypotension, insulin dependent diabetes mellitus, blood/clotting disorders, peripheral vascular diseases, hypertrophy history, or active infection. Subjects were followed at 48 hours postprocedure, 5-10 days, and at 14 days following the ED visit.
Results: A total of 35 patients were enrolled and 36 lacerations were repaired with 2OCA. Mean age was 33.1 (7-78 IQR) years of age. Laceration mean length was 3cm. Pain scale range before application of the skin adhesive was 0 to 5 with mean of 1.97. Pain was decreased in 23% of patients, increased in 9%. Prior to discharge, adequate hemostasis and wound closure occurred in 97.2% and 97.2% percentage of patients respectively. 5-10 day hemostasis and wound closure in 93.5% and 83.8% of patients respectively. 14 day hemostasis and wound closure occurred in
100% of patients not lost to follow up.
Conclusion: This study demonstrates that 2OCA is a safe product in terms of wound closure/bleeding for simple laceration repair in the ED setting. Patient and proper wound selection, protection, and aftercare are important. 2OCA is a practical alternative to other common skin closure techniques available.
Keywords: 2-Octyl cyanoacrylate; Emergency department; Laceration; Injectable anesthetics
Introduction
Surgical adhesives have become more prevalent in the Emergency Department (ED) to close skin lacerations due to their ease of use, more complete surface contact and microbial barrier properties [1-4]. They also have unique advantages over traditional suturing in the ED. This includes the ease of closure, speed of closure, decreased or elimination of the need for topical or injectable anesthetics, and reducing the need for specific aftercare including suture removal. Prior research has found that liquid skin adhesives for laceration closure are less painful and produce similar cosmetic affects when compared to sutures [4].
While skin adhesives offer advantages opportunities for improvement exist. Ease of application is important characteristic. The viscosity of the adhesive may cause problems if too low, flowing into sensitive areas including eyes and mucous membranes. If too high it may not adequately cover the wound or create a raised area that patients may find irritating, particularly children who may scratch at these raised areas which can increase the risk of infection.
Although the use of adhesives for wound closure has been well studied in the literature, little exists on this new formulation of 2-octyl cyanoacrylate (2OCA) (Medline Industries, Inc., Mundelein, IL). While the mechanism of polymerization of 2OCA is similar to other liquid skin adhesives, this formulation has a higher viscosity to avoid run off and is colored violet to ease in its application. Higher viscosity adhesives have been found to be more quickly applied compared to low viscosity adhesives however this difference was small [2]. This formulation is also reported to be less exothermic and may be less painful for patients. The use of 2OCA is not limited to skin and has been used in corneal, nerve, and skin graft repairs [3,5-7]. We sought to evaluate the how this novel skin adhesive would perform for laceration closure in a busy clinical emergency department environment.
Objectives
The aim of this prospective case series is to report clinical data with the application of 2OCA when used for closure on ED patients presenting with lacerations. The research specifically examined the primary outcomes of post-procedure bleeding, dehiscence, and infection. Additionally, patients’ perception of pain following application was investigated.
Methods
This study is a prospective open-label observational case study that took place following institutional review board approval. Patients were recruited from an urban ED with an annual census of 107,000 visits located in the Midwestern United States.
Patients were approached for recruitment in the ED when discussing closure options by the physician. Only patients deemed appropriate for skin adhesive closures by their treating physician were approached. Inclusion criteria included greater than 5 years of age and must be a candidate for use of a topical surgical skin adhesive (determined by attending physician and informed consent by a parental guardian if under age 18). Exclusion criteria included known sensitivity to topical skin adhesive products or degrading products (cyanoacrylates or formaldehyde), a history of keloid formation, hypotension, and insulin dependent diabetes mellitus, blood/clotting disorders, peripheral vascular diseases, or hypertrophy history. Subjects with evidence of active infection or gangrene, wounds of decubitus etiology, mucosal surfaces or across mucocutaneous junctions, and wounds that might be exposed to body fluids or dense natural hair were also excluded.
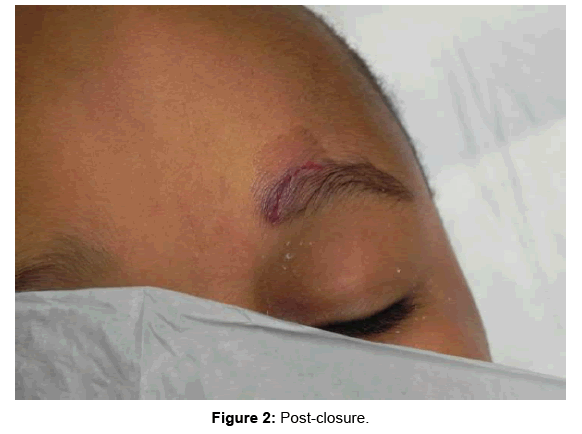
2OCA was applied to skin lacerations in the standardized method as described in the Instructions for Use for the product. A one hour training session was held for investigators by the manufacturer prior to the study initiation. This was performed to ensure the application was performed in a consistent manner by all investigators. Only 5 trained emergency medicine physicians were used to apply 2OCA. The technique included approximation of wound edges with gloved fingers and application of the first layer. After 30 seconds of drying, additional layers were optionally applied at the discretion of the study physician. Photography was taken of the wound before and after application of 2OCA (Figures 1 and 2). The use of a dressing after application was left discretion of the treating physician.
Subjects were followed at 48 hours post-procedure, 5-10 days, and at 14 days following the ED visit. Follow-up phone calls (FUPC) were done at 48 hours, 5-10 days and 14 days by a trained study coordinator.
During FUPC the patient was asked to answer questions about dehiscence (defined as skin separation), infection and active bleeding. These were completed by a trained study coordinator. Questions included observations of pain, dehiscence, and infection. A Likert pain scale was used to estimate pain from 0-5 with 5 being the most amount of pain.
Results
A total of 35 patients were enrolled in the study and 36 lacerations were repaired with Skin Affix. Mean age was 33.1 years of age with age ranging from 7-78 years old. There were 8 black, 24 Caucasian, and 3 Hispanic patients. Layers applied ranged from 1-5. Length of lacerations ranged from 9 to 90 mm with mean length of 22.8 mm. The lacerations were located at the following sites: fingers/toes (22), hand/foot (3), arm (4), leg (1), and face (6). Pain scale range before application was 0 to 5 with mean of 1.97. Patients were asked 15 min after application to rate pain in terms of decreased, increased or no change. Pain was decreased in 23% of patients, increased in 9%, 57% of patients noted no change in pain and 11% were not recorded. Prior to discharge, adequate hemostasis and wound closure occurred in 97.2% and 97.2% percentage of patients respectively. 5-10 day hemostasis and wound closure (the % of patients who did not dehisce) in 93.5% and 83.8% of patients respectively. 14 day hemostasis and wound closure occurred in 100% of patients not lost to follow up. A total of three patients, 8.6%, reported post procedural bleeding at some point during their follow up. Five patients, 13%, reported dehiscence at some time during follow up. Additionally, two patients, 6%, reported infection at the site of the laceration. One infection was reported over phone to a 1.5 cm laceration of left upper arm, which the participant treated at home. A second infection was to a 1.4 cm laceration to left second digit and was treated with an antibiotic course following ED visit 72 hours following initial test product application. Of note, complication rates were tabulated assuming that the three patients lost to follow-up did not suffer from any adverse events.
Conclusion
Ideal skin closure should utilize a technique that is safe, effective, fast and affordable. Skin adhesives have become increasingly utilized for closure of lacerations in the ED. As technology progresses new formulations such as 2OCA have been produced to improve ease of application without altering efficacy.
This study is a first step towards demonstrating the effectiveness and safety of 2OCA in the ED, but has also highlighted the need for further investigation. Overall, the data shows exceptional wound closure and bleeding control rates in the study population at time of discharge at 97.2%. The first two days following closure saw the highest rate of wound dehiscence with 4 of 36 wounds reopened at the 48 hour FUPC. Of the five patients who suffered dehiscence, four patients had finger wounds of which none had been placed in finger splints to protect the wound. Wounds over joints are at risk for dehiscence but use of temporary splinting may mitigate this risk which has been recommended by other investigators [8]. Re-injury of the laceration contributed to some degree to wound dehiscence and delayed closure with at least two of the above five wounds re-opening after second injury. These two were injured by “accidentally bumping it against something”. This patient treated the injury by applying a Band-Aid at home and the bleeding stopped. A second patient reported hitting finger on gas pump causing laceration to be reported open at 48 hour call. The gas pump injury noted that it started to heal, but the patient bumped the finger again per the day 5 call FUPC. It was reported almost healed on day 14 day call. Some variables may increase the risk of dehiscence and infection and are independent of the type of closure procedure used. This includes site of injury, length of time the wound has been open prior to hospital presentation, and age of patient. One study participant reporting the most prolonged bleeding and delayed closure was also the oldest patient (78) enrolled with a wound to his great toe.
Our data differs from a 2014 Cochrane Review of tissue adhesives in closure of surgical lacerations in terms of rates of wound dehiscence. We suspect this to be due to our small sample size. Wound dehiscence was the most common complication in our study as well as the only statistically significant difference in the Cochrane meta-analysis with a rate of 4.5% (RR 3.35; 95% CI 1.53 to 7.33; 10 trials, 736 participants that contributed data to the meta-analysis) [9]. Additionally, the Cochrane Review demonstrated no statistically significant difference for sutures vs skin adhesives with respect to the outcome of infection. The mean percentage as shown in the Cochrane database for skin adhesives infection rate was 7.6%. We had a similar rate of infection at 6%.
One of the advantages of skin adhesives is avoiding the use of needles for anesthesia or suturing. The rated pain score patients reported our study were similar to scores reported in other studies evaluating cyanoacrylates for wound closure [4,8].
The importance of general wound care should be explained to the patient. Avoiding trauma to the wounds and avoid daily cleaning or scrubbing of the wound are important regardless of the methods used to close the wound.
Future studies are needed to add to our understanding of the test product’s role in the ED. 2OCA could replace primarily suturing of a wound in the appropriate clinical setting. Testing various bands under similar conditions with standardized assessments of dehiscence infection and complications would provide useful information. Although more time intensive and challenging, future studies may benefit from either direct visualization of wounds at follow-up to better ensure accurate data reporting.
This study demonstrates that 2OCA is safe alternative to typical sutures in terms of wound closure/bleeding, dehiscence, infection and pain for simple laceration repair in the ED setting. Appropriate wound selection, such as avoiding high tension wounds, and protection (such as splinting a finger) and aftercare may play a role in efficacy and complication rate. 2OCA is a practical alternative to other common skin closure techniques already in place in today’s ED.
Acknowledgements
The authors would like to thank Dr. Bryan Baskin, Dr. Matt Roehrs and Dana Hromyak for their assistance in gathering data. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Mertz PM, Davis SC, Cazzaniga AL, Drosou A, Eaglstein WH (2003) Barrier and antibacterial properties of 2-octyl cyanoacrylate-derived wound treatment films. J Cutan Med Surg 7: 1-6.
- Dumville JC, Coulthard P, Worthington HV, Riley P, Patel N, et al. (2014) Tissue Adhesives for Closure of Surgical Incisions. Cochrane Database Systemic R ev.
- Hallock GG (2001) Expanded applications for octyl-2-cyanoacrylate as a tissue adhesive. Ann Plast Surg 46: 185-189.
- Shapiro AJ, Dinsmore RC, North JH (2001) Tensile strength of wound closure with cyanoacrylate glue. Am Surg 67: 1113-1115.
- Quinn JV, Drzewiecki A, Li MM, Stiell IG, Sutcliffe T, et al. (1993) A randomized, controlled trial comparing a tissue adhesive with suturing in the repair of pediatric facial lacerations. Ann Emerg Med 22: 1130-1135.
- Piñeros-Fernández A, Rodeheaver PF, Rodeheaver GT (2005) Octyl 2-cyanoacrylate for repair of peripheral nerve. Ann Plast Surg 55: 188-195.
- Ritterband DC, Meskin SW, Shapiro DE, Kusmierczyk J, Seedor JA (2005) Laboratory model of tissue adhesive (2-octyl cyanoacrylate) in sealing clear corneal cataract wounds. Am J Ophthalmol 140: 1039-1043.
- Saxena AK, Willital GH (1999) Octylcyanoacrylate tissue adhesive in the repair of pediatric extremity lacerations. Am Surg 65: 470-472
- Coulthard P, Esposito M, Worthington HV, van der Elst M, van Waes OJ (2014) Tissue adhesives for closure of surgical incisions. Cochrane Database Syst Rev 11: CD004287.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi