Short Communication, Clin Dermatol Res J Vol: 2 Issue: 2
The Use of Advance Dermaplaning in Clinical Skin Care and Treatment
Robin Townsend*
Professional Beauty Association, Cooper Road, Suite 203 Cincinnati, USA
*Corresponding Author : Robin Townsend
Professional Beauty Association, Cooper Road, Suite 203 Cincinnati, USA
Tel: 513-807-3192
E-mail: townr10048@aol.com
Received: August 10, 2017 Accepted: October 30, 2017 Published: November 03, 2017
Citation: Townsend R (2017) The Use of Advance Dermaplaning in Clinical Skin Care and Treatment. Clin Dermatol Res J 2:2. doi: 10.4172/2576-1439.1000117
Abstract
Skin barrier function is important to the function and appearance of the skin. Without adequate hydration, the process that normally causes surface cells to shed is disrupted, resulting in flaky, itchy, dry and inelastic skin which can lead to barrier dysfunction. Adequate moisturizing is essential to treating skin with eczema. Treatments such as corticosteriod topicals and emollients cannot be effective in limiting flares of eczema if they cannot reach the skin surface due to barrier dysfunction. Exfoliation is beneficial for removing keratinized skin cells that disrupt normal barrier function. Advanced Dermaplaning is a new approach to exfoliation of the skin, in real time. The addition of Advanced Dermaplaning to the treatment protocol of persons with excessive cellular buildup or atopic dermatitis, can be useful in instantaneously removing the cellular blockage that prevent effectual topical treatment applications and their efficacy.
Keywords: Advanced dermaplane; Exfoliation; Dermaplane; Eczema; Atopic dermatitis; Hyperkeratosis; Non-invasive; Licensed esthetician
Introduction
Sixty-six-year-old woman presented for rejuvenation of her skin. Her primary concerns were dehydration and hyperpigmentation. She had regularly seen her dermatologist for the treatment of eczema on her left ear, a condition that she had been living with for several years. She had been treating the ear with prescription steroid topical treatments as prescribed by her dermatologist [1]. However, the condition persisted.
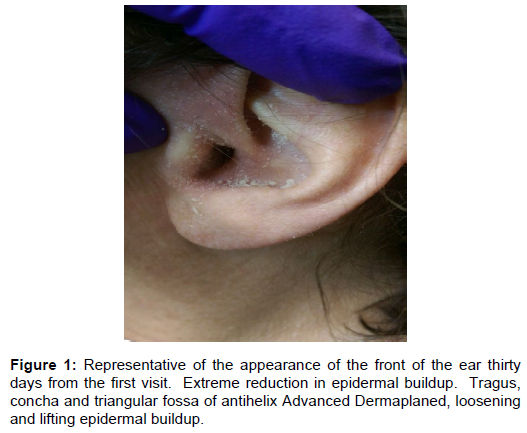
At her initial visit, it was observed that the entire front of the ear was almost completely covered with a proliferation of dry, flaky cellular debris. The actual skin tone was barely visible. The ear was primarily opaque white in color, resembling powder in appearance [2,3] (Figure 1,2).
During the consultation, she indicated that her ear became impacted several times per year, due to her own attempts to cleanse the ear or to remove cellular debris from the ear canal. As a result, she routinely made visits to her ear, nose and throat physician for irrigation or mechanical removal of debris in the canal to prevent further blockage.
Materials
Advance Dermaplaning is a non-invasive procedure that aids in achieving maximum exfoliation of the epidermis, virtually anywhere on the body. It helps to illuminate the skin more effectively for skin analysis, determining treatment protocol and may aid in promoting optimal post-treatment results [4]. The procedure is safe, noninvasive, pain free and can be provided for each skin type and Fitzpatrick. There is no downtime. It can be a stand-alone treatment or pre-treatment. Advanced Dermaplaning is also an excellent treatment option for persons that cannot receive mechanicalmicrodermabrasion or chemical exfoliation due to adverse reactions or contraindications [5,6]. Aggressive exfoliation is one of the leading factors of compromised barrier function [7].
Advanced Dermaplaning is performed using a 10 or 10R-gauge scalpel [8]. The advanced procedure allows the physician, nurse or extensively trained and skilled esthetician to physically exfoliate the skin with much greater detail, including areas such as noses, ears, hands, body and even eyelids [8]. Advanced Dermaplaning is especially beneficial for persons experiencing atopic dermatitis or hyperkeratosis. Major improvements are noticed after a single treatment, including moisture retention, which has a significant impact on the structure and function of the skin and its ability to retain moisture [5,9].
Methods
Performed a comprehensive oral consultation, reviewed intakegeneral skin health history, thorough facial skin analysis and cleansing. Start the Advanced Dermaplaning process once the skin was completely dry. Use a disposable 10 and 10R-gauge scalpel, held at various angles throughout the entire process [8].
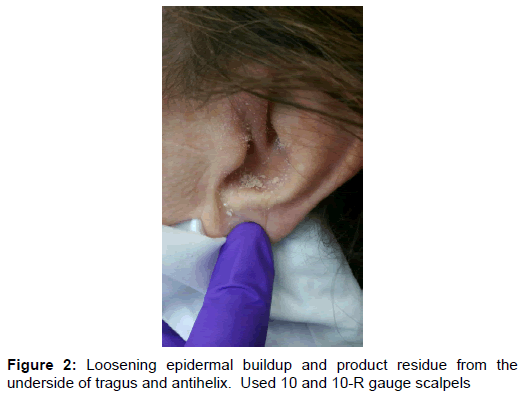
Start the process on the ear lobule and antitragus. Extending the ear lobule while holding the skin firm and taut, feathery strokes were made over the lobule and antitragus using the center of the 10-gauge blade at an angle. Safely and gently loosening and lifting cellular debris [8] exfoliating the skin in real time.
The center portion of the 10-gauge blade was used, at an angle, to exfoliate the helix area of the ear. Start at the upper base of the ear, extending the helix outward, while making small feathery strokes down the helix to the lobule area. At the lower helix region near the lobule area, extended the helix up and taut, using feathery strokes to lift cellular debris until the entire helix was exfoliated.
With the tragus held slightly downward near the center, feathery strokes were made over the tragus with the blade held at an angle. The curve of the 10-gauge blade was used in this area.
In preparing to Advance Dermaplane the triangular fossa, the antihelix and concha, her head was placed comfortably at an angle that would allow cellular debris to fall away from the ear canal. With each of these areas, the curve of the 10R gauge blade was used to carefully and skillfully loosen and remove the cellular debris.
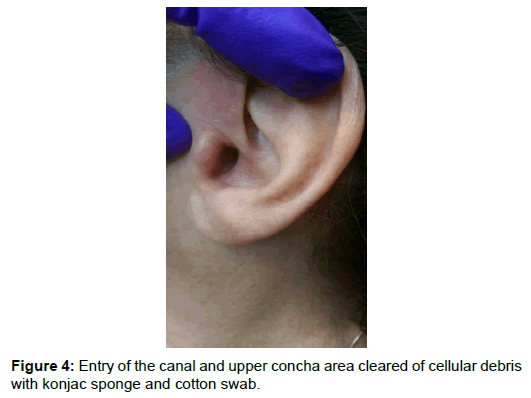
With her head still resting at an angle, a slightly damp konjac sponge was used to make circular motions around the entry of the ear canal. This loosened the debris. A moist konjac sponge was then used to cleanse this area, while capturing most of the dry cells onto the sponge in the process. Moist cotton swabs were also used to capture residual skin cells.
Once the entire ear was clear of cellular debris, the ear was cleansed with an anti-bacterial cleanser, hydrated with hyaluronic serum and fragrance-free sun protection was applied [9,10].
Results
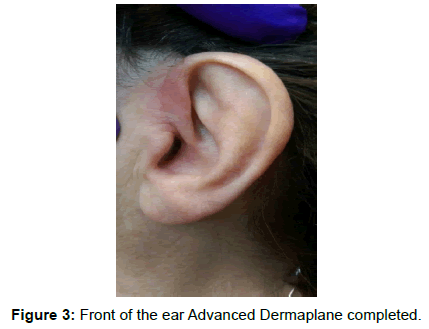
The results from Advanced Dermaplaning at this visit were very gratifying for this woman. Her entire ear was free and clear of all cellular debris and accessible. Skin tone was restored and no longer hidden. Skin texture was smooth and soft with enhanced appearance. She showed no signs of ill results or trauma and displayed minimal erythema. This treatment not only improved her appearance, but prepared her skin for skin surface hydration (Figure 3).
By removing cellular debris proliferation, there was also the ability to palpate the affected skin and perform a more thorough visual assessment [3]. Dehydration was visible. Due to strong water-binding potential, hyaluronic acid was applied [10]. She experienced no stinging sensations or burning. This helped to aid in dehydration itch, as well. Her overall skin response to corrective hydrating treatments was successful [1] (Figure 4).
It was recommended that she return monthly for Advanced Dermaplaning to ensure that this condition would not reoccur at the level to which it appeared prior to this procedure. Education regarding home skin health measures for the treatment of eczema were discussed in detail including water consumption, environmental factors, and skin barrier support [1,3,9,11].
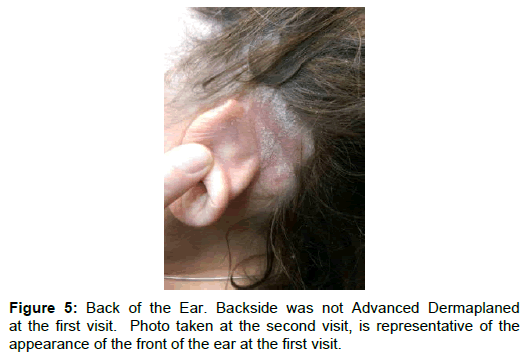
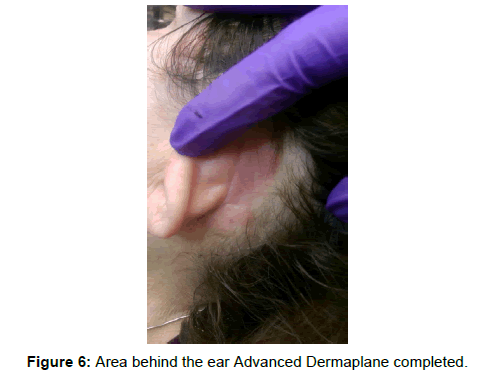
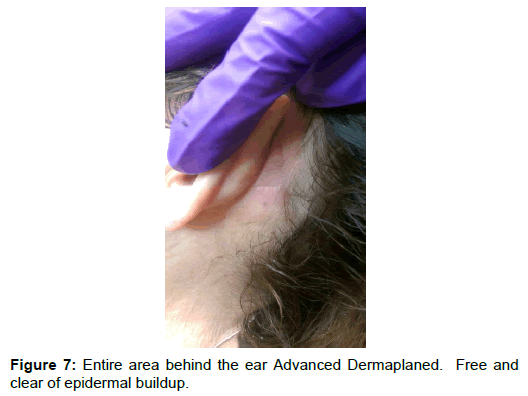
At her next visit one month later, she revealed an area behind her left ear that was not Advanced Dermaplaned during her initial visit. The photos provided show the before and after effects of Advanced Dermaplaning of the area behind the ear at the second visit. They also show the appearance of the front of the ear, which was Advanced Dermaplaned at the initial visit, one month later (Figure 5,6,7).
Summary
In this case, due to excessive epidermal proliferation, product application, surface hydration, and penetration was ineffective, including prescription topicals [1,3,11]. Advanced Dermaplaning eliminated the cellular buildup on the epidermis in an effective manner that did not injure or disrupt the skin barrier, in real time. Advanced Dermaplaning also restored the stratum corneum normal function allowing adequate skin hydration instantaneously [3]. The procedure resulted in smooth, hydrated skin and the alleviation of several of the symptoms associated with eczema including dry patches, flaking, itching and irritation [12].
Acknowledgements
Kathleen Calvaruso Damato, Esther Lynette Williams, Ph.D., Suzanne Kirk, Ph.D., Karen Jobalia, MD.
References
- Lee JH, Son SW, Cho SH (2016) A Comprehensive Review of the Treatment of Atopic Eczema. Allergy Asthma Immunol Res 8: 181-190.
- Dr. Claudia Aguirre. The Biology Behind Eczema and Psoriasis.
- Harding CR (2004) The Stratum Corneum: Structure and Function in Health and Disease. Dermol Ther 17: 6-15.
- Malherbe W (1977) Dermatone Dermaplaning and Sycosis Nuchae Excision. Clin Plast Surg 4: 289-296.
- American Board of Cosmetic Surgery.
- Nguyen T (2014) Dermatology Procedures: Microdermabrasion and Chemical Peels. FP Essent 426:16-23.
- Dr. Diana Howard. Methods of Exfoliation. International Dermal Institute.
- L Pryor, C Gordon, E Swanson, R Reish, K Horton-Beeman, et al. (2011) Dermaplaning Topical Oxygen and Photodynamic Therapy a Systematic Review of the Literature. Aesthetic Plast Surg 35: 1151-1159.
- VanZuuren EJ, Fedorowicz Z, Christensen R, Lavrijsen A, Arents BWM (2017) Emollients and Moisturizers for Eczema. Cochrane Database Syst Rev 2: CD012119.
- Weindl G, Schaller M, Schäfer-Korting M, Korting HC (2004) Hyaluronic Acid in the Treatment and Prevention of Skin Diseases: Molecular Biological, Pharmaceutical and Clinical Aspects. Skin Pharmacol Physiol 17: 207-213.
- Simion FA, Abrutyn ES, Draelos ZD (2005) Ability of Moisturizers to Reduce Dry Skin and Irritation and to Prevent Their Return. J Cosmet Sci 56: 427-444.
- American Academy of Dermatology.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi