Case Report, Clin Oncol Case Rep Vol: 5 Issue: 12
Tumor to Tumor: Metastatic Lobular Breast Carcinoma into Primary Clear Cell Renal Cell Carcinoma
Gema Moreno Abenza1*, Oriol Daga Martinez2, Liliana Fabiola Castillo Paredes1, Jose Luis Ruiz Cerda2, Ana Santaballa Bertran3, Beatriz Montero Balaguer1, Rosa María Viguer Benavent4, Guillermina Montoliu Fornas4, David Ramos Soler1
1Department of Pathology, Pathological Anatomy Service of La Fe University and Polytechnic Hospital, Valencia, Spain
2Department of Urology, Urology Service of the La Fe University and Polytechnic Hospital, Valencia, Spain.
3Departemnt of Medical Oncology, La Fe University and Polytechnic Hospital, Valencia, Spain.
4Department of Radiodiagnosis Service of the La Fe University and Polytechnic Hospital, Valencia, Spain
*Corresponding Author: Gema Moreno Abenza
Department of Pathology, Pathological Anatomy Service of La Fe University and Polytechnic Hospital, Valencia, Spain
E-mail: gemamorenoabe@gmail.com
Received: November 26, 2022; Manuscript No: COCR-22-81312;
Editor Assigned: November 28, 2022; PreQC Id: COCR-22-81312 (PQ);
Reviewed: December 12, 2022; QC No: COCR-22-81312 (Q);
Revised: December 16, 2022; Manuscript No: COCR-22-81312 (R);
Published: December 21, 2022; DOI: 10.4172/cocr.5(12).265
Citation: Abenza GM, Martinez OD, Paredes LF, Cerda JL, Bertran AS, et al. Tumor to Tumor: Metastatic Lobular Breast Carcinoma into Primary Clear Cell Renal Cell Carcinoma. Clin Oncol Case Rep 5:12
Abstract
Tumor to tumor condition is a rare phenomenon described in up to 15% of tumor in patients that present more than one primary tumor simultaneously. The most common metastatic donor primary tumor is lung carcinoma, followed by invasive ductal carcinoma of the breast, prostatic acinar adenocarcinoma, and papillary thyroid carcinoma. Herein, we present a case regarding a 61 year-old tumor patient who developed a metastasis of lobular carcinoma of the breast over a primary clear cell renal cell carcinoma diagnosed incidentally.
Keywords: Tumor to tumor; Clear cell renal cell carcinoma; Lobular carcinoma of the breast
Introduction
Metastasis from a primary neoplasm into other primary neoplasm within the same individual is considered an extremely rare phenomenon. To date, fewer than 50 cases have been reported along the literature since the first description by Bernet in 1902, who described the existence of a metastasis of a squamous cell carcinoma of3 the jaw within a hypernephroma [1,2]. Afterwards, Hammann et al (1927) described a primary thyroid tumor metastasizing on a hypernephroma [2]. Subsequently, several other cases have been reported, such as Campbell et al (1968), who collected in his revision study up to 32 cases from different authors analyzing and describing primary donor tumors and primary recipient tumors within the same patient [2]. The vast majority of donor tumors of the metastatic process are bronchogenic carcinomas (52%), histologic type not specified [3], followed by ductal carcinomas of the breast [1,2, 4-7], prostate acinar adenocarcinomas and papillary carcinoma of thyroid [3].
The most frequent primary tumor receiving metastases are clear cell renal cell carcinoma (71% of cases) [1-8], followed by sarcomas, prostate and pancreatic adenocarcinomas, among other much more infrequent tumors [2]. More infrequently cases of metastasis from malignant carcinomas into primary benign renal tumors have also been described [9,10], such as metastasis from ductal carcinoma of the breast into renal angiomyolipoma and metastasis from lobular breast carcinoma on renal oncocytoma [9,10].
Case Report
We described a case of a 61 years old female patient diagnosed in 2014 of a lobular carcinoma of the breast, type luminal A, treated by bilateral mastectomy and selective sentinel node biopsy followed by hormone therapy. None of the sentinel nodes were affected by the tumor. The tumor stage was pT3a.
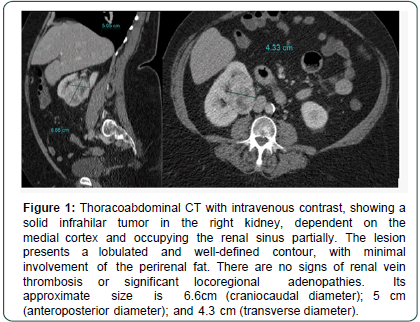
Previously, in 2019, the patient presented elevation of biochemical tumor markers, such as Ca 15.3. On the same year 2019, in our institution it was detected a metastasis at the left axillary lymph nodes and the presence of an incidental kidney tumor to 6 cm. So surgical resection of the tumor mass was decided. Radiologically, the renal tumor shows a solid consistency and a heterogeneous pattern. Its location is infrahilar and partially occupies the renal sinus. Its contours is well defined and lobulated, with minimal involvement of the perirrenal fat. There are no signs of renal vein thrombosis or significant locoregional lymphadenopathy. Its craniocaudal diameter size is 6.6 cm approximately (Figure 1).
Figure 1: Thoracoabdominal CT with intravenous contrast, showing a solid infrahilar tumor in the right kidney, dependent on the medial cortex and occupying the renal sinus partially. The lesion presents a lobulated and well-defined contour, with minimal involvement of the perirenal fat. There are no signs of renal vein thrombosis or significant locoregional adenopathies. Its approximate size is 6.6cm (craniocaudal diameter); 5 cm (anteroposterior diameter); and 4.3 cm (transverse diameter).
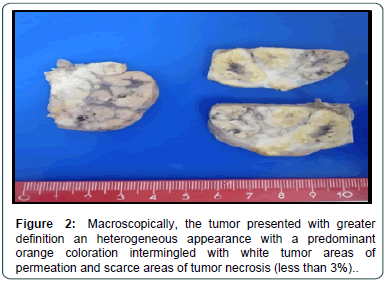
At the laboratory we received a radical nephrectomy specimen measuring 10 cm × 6 cm × 6 cm (craniocaudal diameter, anteroposterior diameter and transverse diameter, respectively). On gross examination, the presence of a well-defined 6 cm nodular lesion in upper pole renal was observed, showing an heterogeneous appearance with white, orange and yellowish areas (Figure 2).
The lesion, seemingly, infiltrates the perirenal fat and renal sinus vessels, at the macroscopical level.
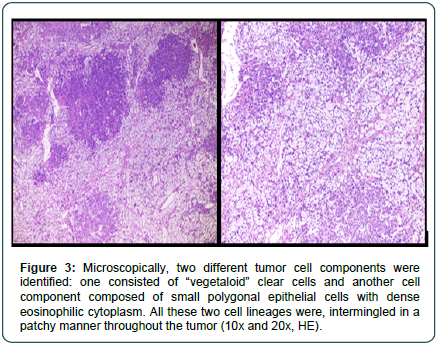
Microscopically, two different tumor areas were distinguished at routine conventional hematoxylin-eosin staining. Tumor cells were arranged in solid nests intermingled with each other andseparated by fine tracts of interposed collagen tissue fibers (Figures 3).
Figure 3: Microscopically, two different tumor cell components were identified: one consisted of “vegetaloid” clear cells and another cell component composed of small polygonal epithelial cells with dense eosinophilic cytoplasm. All these two cell lineages were, intermingled in a patchy manner throughout the tumor (10x and 20x, HE).
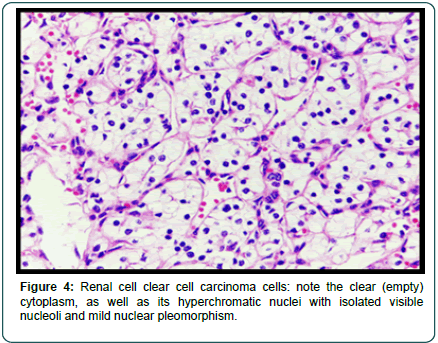
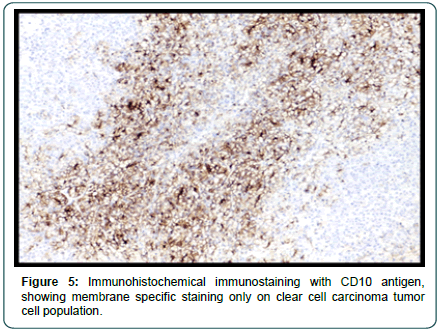
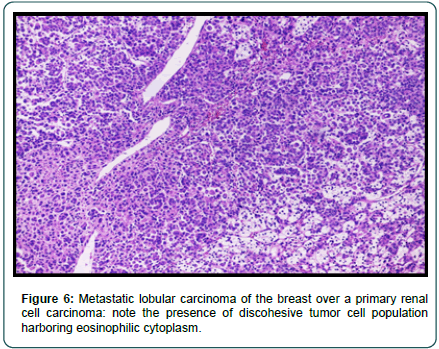
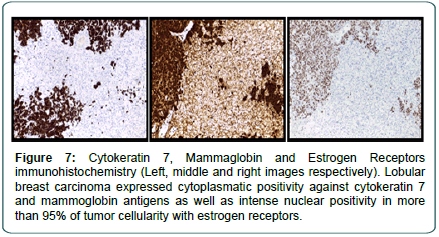
One tumor population presented a microscopically empty clear cytoplasm and with a vegetal-like histological appearance, with hyperchromatic nuclei with a visible nucleolus under 10x objective lens as well as mild nuclear pleomorphism (Figure 4). These tumor cells were positive with Vimentin and CD10 at the immunohistochemical level (Figure 5). The second tumor cell population consisted of atypical epithelial cells, with a rhabdoid appearance, and a moderate amount of dense eosinophilic cytoplasm, hyperchromatic nuclei with salt and pepper chromatin without visible nucleoli and with more intense nuclear pleomorphism (Figure 6). These cells were positive with Cytokeratin 7, GATA 3, Mammoglobin and Estrogen Receptors (intense positivity, 95% of cellularity) (Figure 7), being negative against vimentin and CD10, in comparison with the first tumor cells population. However, this last cell population was negative for Progesterone Receptors and the proliferation index measured by Ki-67 immunolabelling was 20% (corresponding to lobular carcinoma of the breast, type Luminal B subtype).
Figure 7: Cytokeratin 7, Mammaglobin and Estrogen Receptors immunohistochemistry (Left, middle and right images respectively). Lobular breast carcinoma expressed cytoplasmatic positivity against cytokeratin 7 and mammoglobin antigens as well as intense nuclear positivity in more than 95% of tumor cellularity with estrogen receptors.
Consequently, we identified two completely different tumor cell populations with different anatomical origins. Therefore according to the patient´s clinical evolution we can conclude that it was probably a metastatic lobular carcinoma of the breast, luminal B subtype, over a primary clear cell renal cell carcinoma of the kidney. The patient received radiotherapy at the left breast and axilla with a maximum dose of 50 Gray and three cycles of chemotherapy with palbociclib and fulvestrant which was terminated due to poor general conditions of the patient. After confirming tumor progression with the appearance of bone metastases as well as the progressive deterioration of the general conditions (liver failure and encephalopathy refractory to treatment), therapeutic adequacy was decided and the patient died two days after the last hospital admission.
Discussion
We present a case of a patient with a metastatic lobular breast carcinoma into a clear cell renal cell carcinoma. In comparison with the cases described to date in the literature, in which metastatic tumors to the kidney have been mainly bronchopulmonary and ductal carcinomas of the breast in origin [1,2, 4-7]. Specifically, our case deals with a metastasis of a lobular breast carcinoma on a clear cell renal cell carcinoma, which is the model of a tumor-to–tumor condition less frequently described in literature [11,12]; although the recipient tumor of the metastasis is the most frequently described [1-8,11,12].
In an attempt to explain why clear cell renal cell carcinoma (hypernephroma) is the preferred recipient tumor for metastases from other primary tumors two different theories have been elaborated [1,2,11-14]. First theory deals with a mechanistic theory which tries to explain this finding because the kidney is one of the most vascularized organs of the body and receives a high blood flow which favors tumor emboli on its parenchyma. Second theory deals with a “seed and soil theory” which supports that renal carcinoma due to its high content lipids and glycogen favors an environment in which tumor cells can develop and grow easily. These two theories try to explain this event but there is still much to elucidate about this topic.
In any case, pathologist may kept this entity in mind, especially on biopsies or surgical specimens with two completely different tumor cell populations, both morphologically and immunophenotypically. It is important for medical surgeons and pathologists to be aware of this rare phenomenon due to its influence on patient outcome and the therapeutic approaches to be carried out.
Conclusion
In conclusion, despite being an infrequent entity, tumor to tumor is a biological phenomenon that has to be kept in mind for surgeons, oncologists and obviously for pathologists when metastatic disease does not respond completely to neoadjuvant treatments, or when there are two concomitant tumor cell populations and there exist a history of others primary tumors in distant locations.
Acknowledgement
This article and the research that supports it would not have been possible without the exceptional support and help received from my colleague and friend, David Ramos. His enthusiasm and knowledge as pathologiest and researcher has been an inspiration in my work and in the writing of this article. Likewise, I must thankmy colleague Beatriz Montero and Liliana Fabiola Castillo, for their help in finding information related to the topic we are dealing within this article. I must thank the excellent work of the urologists, radiologists, pathologists and oncologists at my hospital, who have contributed to take an adequate diagnosis and the best therapeutic management of this patient. I would like to thank the doctors Rosa Viguer and Guillermina Montoliu for the radiological images lent for the article.
References
- Sella A, & Ro JY (1987) Renal cell cancer: Best recipient of tumor-to-tumor metastasis. Urology 30: 35-38. [Google Scholar] [Cross Ref]
- Campbell Jr LV, Gilbert E, Chamberlain Jr CR, Watne AL (1968) Metastases of cancer to cancer. Cancer 22: 635-643. [Google Scholar] [Cross Ref]
- Song JSA, Taylor SM, Trites J, Rigby MH, Bullock MJ, et al. (2017) Tumor-to-tumor metastases: Papillary thyroid carcinoma into a clear cell renal cell carcinoma. J Otolaryngol Head Neck Surg 46: 1-4. [Google Scholar] [Cross Ref]
- Viedma MU, Barona RL, de la Guardia FVD, Padilla SM (2016) Carcinoma renal de celulas claras metastatizado por carcinoma ductal de mama. Arch Espanoles Urolog 69: 197-201. [Google Scholar] [Cross Ref]
- Gazel E, Yalcin S, Kaya E, Uner A, Saglican Y, et al. (2018) Metastasis of breast cancer to renal cell carcinoma: A rare case of tumor-to-tumor metastasis. Clin Surg 3: 1935. [Google Scholar] [Cross Ref]
- Huo Z, Gao Y, Yu Z, Zuo W, Zhang Y (2015) Metastasis of breast cancer to renal cancer: Report of a rare case. Intern J Clin Experimen Pathol 8: 15417. [Google Scholar] [Cross Ref]
- Lakovschek IC, Petru E, Pollheimer MJ, Ratschek M, Augustin H, et al. (2019) A rare case of cancer-to-cancer metastasis: Breast cancer to renal cell cancer. Wiener Medizinische Wochenschrift 169: 350-353. [Google Scholar] [Cross Ref]
- Maloney JD, Immergut M (1968) The kidney as host in cancer-to-cancer metastasis. J Urol 98: 657-660. [Google Scholar] [Cross Ref]
- Amin M, Radkay L, Pantanowitz L, Fine J, Parwani A (2013) Tumor-to-tumor metastasis (TTM) of breast carcinoma within a solitary renal angiomyolipoma: A case report. Pathol Res Pract 209: 605-608. [Google Scholar] [Cross Ref]
- Bitner DP, Clements MB, Cathro HP, Mithqal A, Schenkman NS (2017) Remote development of tumor-to-tumor metastasis of breast adenocarcinoma in a renal Oncocytoma. Urol 107: E1-E2. [Google Scholar] [Cross Ref]
- Perrin C, Talarmin M, Fontaine A, Kerbrat P, Audrain O, et al. (2011) Métastase d’un carcinome mammaire dans un carcinome rénal. Annales Pathol 31: 399-401. [Google Scholar] [Cross Ref]
- Chanu T, Pavel CS, Saint-Frison MH, Hescot S, Oro H (2015) Metastasis of a primary tumor in renal cell carcinoma: A rare and surprising event. Advan Urol 25: 711-715. [Google Scholar] [Cross Ref]
- Fidler IJ, Poste G (2008) The “seed and soil” hypothesis revisited. Lancet Oncol, 9: 808. [Google Scholar] [Cross Ref]
- Pinthus JH, Whelan KF, Gallino D, Lu JP, Rothschild N (2011) Metabolic features of clear-cell renal cell carcinoma: Mechanisms and clinical implications. Canad Urolog Asso J, 5: 274-282. [Google Scholar] [Cross Ref]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi