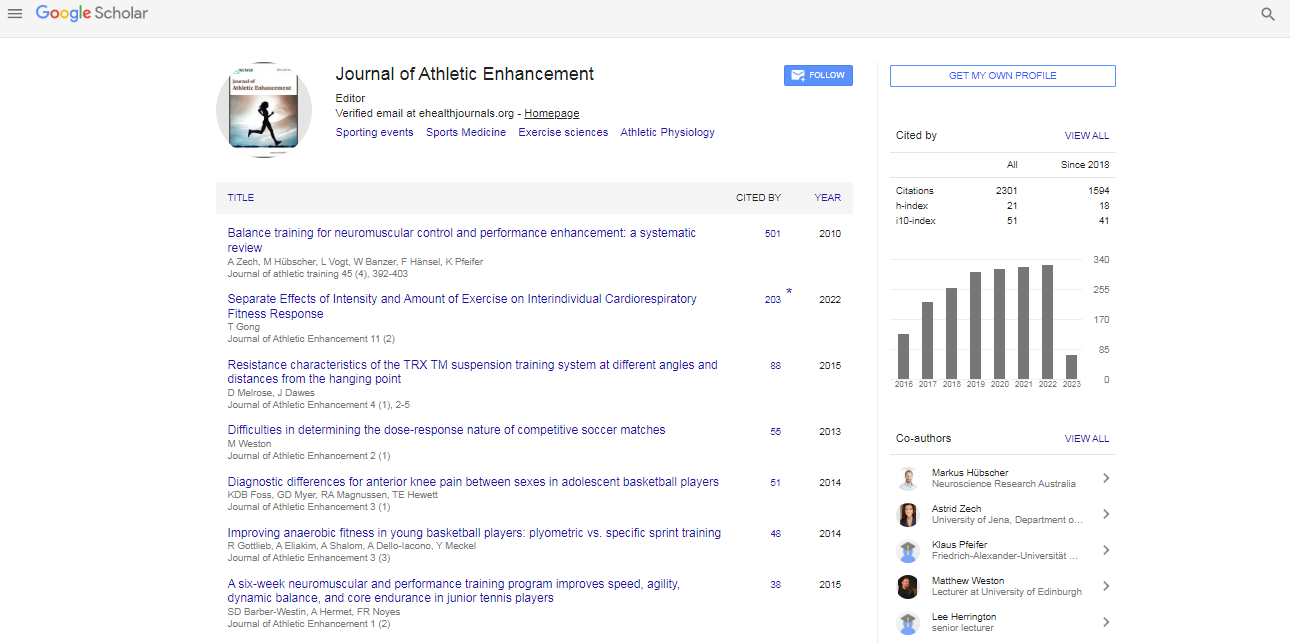
Review Article, J Athl Enhanc Vol: 11 Issue: 6
Virtual Reality in Sport Rehabilitation: A Narrative Review
Wai Kiu Thomas Liu1, Peter KT Siu1 and Tak Man Wong2*
1Department of Orthopaedics and Traumatology, Queen Mary Hospital, Hong Kong
2Department of Orthopaedics and Traumatology, School of Clinical Medicine, The University of Hong Kong, Hong Kong
*Corresponding Author: Tak Man Wong, Department of Orthopaedics and Traumatology, Queen Mary Hospital, 102 Pok Fu Lam Road, Hong Kong Tel: +852-22556899 E-mail: wongtm@hku.hk
Received date: 24 May, 2022, Manuscript No. JAE-22-64802;
Editor assigned date: 26 May, 2022, PreQC No. JAE-22-64802 (PQ);
Reviewed date: 06 June, 2022, QC No. JAE-22-64802;
Revised date: 16 June 2022, Manuscript No. JAE-22-64802 (R);
Published date: 22 June, 2022, DOI: 10.4172/2324-9080.1000026
Citation: Liu TW, Siu PKT, Wong TM (2022) Virtual Reality in Sport Rehabilitation: A Narrative Review. J Athl Enhanc 11:6.
Abstract
Objective: In the past two years, the social distancing practice of COVID-19 pandemic has caused a surge in the demand of remote health service, including teleconsultation and telerehabilitation. With technology advances, research in the use of virtual reality for rehabilitation has emerged in recent years. This narrative review will provide the latest overview of rehabilitation using virtual reality in musculoskeletal condition, with a particular focus on sports injuries. This review aims to investigate the effectiveness of virtual reality and summarise the potential benefits, concerns, and the future of virtual reality in the field of rehabilitation.
Results: Virtual reality has been employed in rehabilitation of gait and postural control in various medical conditions, in which it has been shown to be effective. Apart from postural rehabilitation, the use of virtual reality has also been studied in the rehabilitation of various musculoskeletal conditions. Several studies have investigated the use of virtual reality for patient after ACL reconstruction, and the results are promising. Besides physical rehabilitation, virtual reality offers psychological preparation for patients to return to sports. Virtual reality offers various advantages to conventional rehabilitation. This includes reducing therapist’s workload, enhancing patient’s autonomy, psychological preparation through near-real-life scenario, offering complex assessment, readily available at home and increasing enjoy ability and compliance. However, there are still challenges for using virtual reality for rehabilitation, for example, need for technical expertise, motion sickness, lack of supervision by therapist and questionable accuracy of motion tracking.
Conclusion: In summary, using virtual reality in rehabilitation has shown early success, however, there are still challenges and questions to be explored. Up to now, there is no high-level evidence supporting the use of virtual reality in rehabilitation. Further research is encouraged in this field in order to provide a better understanding of its effectiveness.
Keywords: Sports rehabilitation, Musculoskeletal rehabilitation, Virtual reality
Introduction
Musculoskeletal disorder is one of the most common medical problems that we may encounter. According to studies, the prevalence was up to 70% [1]. Most of musculoskeletal disorders are sport related injuries. Sport rehabilitation is essential part of musculoskeletal rehabilitation. In the past two years, the social distancing practice of COVID-19 pandemic has caused a surge in the demand of remote health service, including teleconsultation and telerehabilitation. With technology advances, virtual reality has been developed in the field of digital media to integrate imaginary worlds and stories with the reality [2]. Virtual reality is a new technology enabling people to involve themselves in a virtual and interactive environment that they feel it was real. This technology induces a subjective sense of presence by creating a vivid and interactive simulation with the ultimate aim to enable user to transcend into the virtual world. The extent of interaction can be various, from two-dimensional virtual environment to real-time perception and interaction [3]. Virtual reality can be classified into non-immersive or immersive [4]. Non-immersive system involves individual using devices such as a mouse or controller to interact with the simulated world projected on a display. Immersive system utilizes devices such as Head Mounted Displays (HMD) to project a three-dimensional simulated world. Newer virtual reality systems allow larger Fields of View (FOV) and block external visual information by using portable Head Mounted Displays (HMD). User can interact with the virtual environment using pre-existing or custommade devices [5,6]. Research in the use of virtual reality for rehabilitation has emerged in recent years. This narrative review will provide the latest overview of rehabilitation using virtual reality in musculoskeletal condition, with a particular focus on sports injuries. This review aims to investigate the effectiveness of virtual reality and summarise the potential benefits, concerns, and the future of virtual reality in the field of rehabilitation.
Evidence of Virtual Reality in Rehabilitation
Virtual reality has been employed in rehabilitation of gait and postural control in various medical conditions. Evidence has demonstrated that the concurrent use of virtual reality games and traditional physiotherapy exercises have positive implications on the gait and postural control of children with cerebral palsy, and it is more effective than physiotherapy exercise alone [7]. Virtual reality rehabilitation significantly improved their strength compared to traditional physiotherapy, and slightly more effective in improving postural balance and motor control development. The author attributed these improvements to the increased enjoyability and physical and cognitive fidelity. It has been proposed that virtual reality technology and commercial video games can reduce fall and improve postural control in patients with acquired brain injury by increasing their motivation to rehabilitation and changing their movement control strategies [8]. A systematic review had demonstrated that using virtual reality to assess postural balance of elderly could identify individuals with impaired balance [9]. It also showed that virtual reality using HMD reduced incidence of fall and improved gaits. Apart from training, virtual reality has been employed for the assessment of patients during the rehabilitation. Functional neuropsychological assessment and postural control assessment using virtual reality have been developed for patients with concussion, and it has an increased sensitivity than traditional paper or computerized assessments [4]. A “moving room” simulation using virtual reality can help to identify patients with persistent perceptual-motion disintegration, which may predispose the patients to musculoskeletal injuries in the future. Virtual reality technology also allowed creation of virtual real-life scenarios for neuropsychological functional assessment, which may not be covered in traditional assessments. The virtual scenarios could be controlled and individualized to meet the needs of individual patient. A meta-analysis study suggested that playing Wii Fit (Nintendo, Japan), a home-based active video game, encouraged faster weight loss in post-partum women and increase physical activity and function in elderly. Compared to traditional therapy, balance training using Wii Fit for patients demonstrated a similar Berg Balance Score (BBS) and an improved Time-Up-and-Go test (TUG) [10].
Evidence of Virtual Reality in Musculoskeletal Rehabilitation
Apart from postural rehabilitation, the use of virtual reality has also been studied in the rehabilitation of various musculoskeletal conditions. Ankle injuries accounted for up to 30% of all sports injury [11]. Up to 70% of patients after ankle sprain reported residual symptoms and re-injury [12]. These might have been predisposed by the reduced muscle strength, reduced proprioception and poor postural control after the injury [13]. A systematic review with five randomised controlled trials had demonstrated that rehabilitation by virtual reality for functional ankle instability could significantly improve 30 seconds single leg standing test result compared to traditional training. They concluded that the overall improvements in muscle strength, proprioception and maintaining body balance were superior to conventional therapy. In a systematic review of nineteen studies, the author investigated the effect of virtual reality in the rehabilitation of general musculoskeletal disorders and regional dysfunctions [14]. Regarding general musculoskeletal disorders, rehabilitation by virtual reality was more effective than no treatment in the management of fibromyalgia and no significant difference in the effectiveness was shown between virtual reality and exercise therapy in the management of rheumatoid arthritis. Regarding regional dysfunction, the study investigated the effect of virtual reality in shoulder impingement syndrome, osteoarthritis of knee, post-total knee arthroplasty, post- ACL reconstruction, ankle sprain and low back pain, in which virtual reality was not significantly more effective than physical exercises. Effective postoperative rehabilitation dictates the outcomes of any orthopedic surgery. However, there is no consensus on the rehabilitation regime after total knee arthroplasty [15]. A recent randomised controlled study, published in 2020, compared the efficacy of in-patient rehabilitation with virtual reality and that of conventional rehabilitation after total knee arthroplasty [16]. Although no significant differences were found in pain relief, muscle strength and patient’s satisfaction, the improvement of global proprioception was significantly higher in the group underwent virtual reality rehabilitation. An experimental study demonstrated that accurate tracking of location and speed of movement of upper limb was feasible when using HTC VIVE virtual reality rehabilitation training system [17]. However, lower score was observed in the system usability in the post-test questionnaire, as it was reported that the handle was difficult to operate. The author suggested that patients should be well-trained before they start rehabilitation using virtual reality.
Evidence of Virtual Reality in Post-Acl Reconstruction Rehabilitation
Anterior cruciate ligament (ACL) injury is one of the most common encountered sport injuries. Not only it requires operative treatment, but extensive rehabilitation programme is also warranted in order to achieve a favorable post-operative outcome. However, about 1 in 4 patients are at risk of suffering another injury after returning to highdemand sports [18,19]. A recent retrospective study investigated the use of mobile application that taught patients home-based exercises for patients after ACL reconstruction [20]. At post-operative 3 weeks, mobile app users were more likely to demonstrate quadriceps locking during walking with crutches and be pain-free; however, the difference was not significant at 6 weeks. The author suggested that it might encourage quadriceps awakening, hence preventing atrophy, functional deficit, gait instability, knee pain and early osteoarthritis. A small prospective randomized controlled double-blind trial, with 30 subjects, compared the functional outcomes between Nintendo Wii Fit and conventional rehabilitation for patients after arthroscopic ACL reconstruction [21]. No significant difference was found between the two groups in terms of the dynamic balance, coordination, proprioception, response time and the strength of knee flexors and extensors at first, 8th and 12th weeks. Both groups showed significant improvement in dynamic stability, coordination and proprioception after the programme. The author suggested that rehabilitation using the Wii Fit Balance programme is a practical, cost-effective and safe alternative to conventional rehabilitation. ACL injury is not purely a ligamentous problem; research has shown that it is associated with functional neuroplasticity [22]. One-third of professional athletes could not return to their level of sport 3 years after ACL reconstruction [23]. Therefore rehabilitation after ACL injury should not only focus on the strength, but also the sensorimotor rehabilitation. This can potentially be achieved by using virtual reality, as evidenced by research on using virtual reality to improve gait and postural control [7-9]. About two-third of players who could not return to play after ACL reconstruction reported a psychological reason, most commonly the fear of reinjure [24]. It is recognized that psychological readiness is a vital factor for return-to-play after injury in sport players [25]. Rehabilitation after ACL reconstruction should also incorporate the psychological readiness to address these issues. Evidence has also shown that relaxation intervention with virtual reality was effective in reducing anxiety and boost confidence of healthy sport players during stressed condition [26]. This may in turn enhance their performance, as anxiety negatively impacts sports performance [27,28]. Virtual reality has also been studied for analyzing and enhancing the performance of sports players, in which the outcomes were favorable [29,30].
Advantages of VR
As virtual reality can be controlled remotely, clinicians or therapists do not have to physically be with the patients. This allows patients to undergo rehabilitation at home or in different locations. It helped to reduce the therapist’s workload, while enhancing patient’s autonomy in rehabilitation.
Virtual reality offered a near real-life scenarios, which traditional rehabilitation or assessment could not. This could be utilized to prepare psychological rehabilitation training for patients or athletes after injury. This may help to overcome the fear of reinjure and improve the readiness to return-to-play. In addition, virtual reality offered a safe environment for patients to experience various real-life scenarios. Patients do not have to bear the same risk of injury during training as undergoing training in real life scenario. Traditional assessments usually focused on separated components in rehabilitation, whereas virtual reality offered a complex assessment of neuropsychological, physical and behavioral functions of patients. From entertainment to clinical use, virtual reality has become more readily available and less costly. Virtual reality setup ranges from expensive complex simulation device to simple portable devices such as head-mounted displays with hand-held controllers. Therefore virtual reality is not only exclusive to hospital setting, but it can also be used at home. This is especially useful in the COVID-19 era, when social distancing is in practice. Physical rehabilitation and psychological therapy using virtual reality have been employed for patients recovering from COVID-19 [31]. Traditional physical rehabilitation training involves home exercises to be performed by patients, which often has low adherence and may seem boring due to the repetitive nature. Studies have suggested that the vivid image and game-like scenarios of virtual reality could increase the enjoyability during training [7,10]. This is especially useful in younger population and can help to increase the compliance of rehabilitation training. It may create distraction from fatigue and anxiety that may otherwise hinder movement.
Disadvantages of VR
Although virtual reality devices are readily accessible, development of rehabilitation tools and assessments required technical expertise. Individual patient may not be able to tolerate virtual reality well, for example, patients may develop cyber sickness. Motion sickness occurs when actual received signal is different from the sensory perception [32]. Study had reported that virtual reality could cause motional sickness, disorientation and dizziness in patients within 3 days after concussion injury [33]. Long-term adverse effect of virtual reality is currently unclear. With the technological advancement, the use of virtual reality in rehabilitation seems to be the latest trend. However, its effectiveness and efficacy are still yet to be established with highlevel research evidence. When using home-based virtual reality gaming console for rehabilitation without supervision by therapist, patients may focus on the result of the game instead of the quality of movements [34]. This may predispose the patients to injury and reduced effectiveness of training due to poor posture. Problems have been reported in the accuracy of motion tracking when using commercial gaming technology for home-based rehabilitation [35]. The accuracy depended on the movements and the position of the patients, and fine hand motion might not be accurately detected [36-38]. This limits the use of virtual reality system in rehabilitation of fine movements, for example, functional rehabilitation of hand after injury. However, with the foreseeable technological advancement, this issue is likely to be resolved. Although virtual reality training can be employed at home, it does not compose of manual therapy by therapist. Touch therapy has been proven effective to relieve pain [39,40]. Hence, it can be potentially used with manual therapy in order to provide optimal rehabilitation outcome for patients.
Conclusion
Many studies have suggested that rehabilitation using virtual reality is as effective as conventional rehabilitation. Early evidence showed that postural control and proprioception training with virtual reality were effective, and could prevent future fall and re-injury. Virtual reality has already been employed for the rehabilitation of various musculoskeletal conditions, including sports injury such as post-ACL reconstruction, and has been shown to be as effective as conventional training. Other than providing physical sensorimotor training, virtual reality can offer psychological preparation for patients as it can display vivid virtual real-life scenarios, which has been shown to be especially important for sports player after injury. Rehabilitation using virtual reality confers many benefits compared to traditional rehabilitation programme. Most importantly, virtual reality systems are often fun to participate in and can encourage compliance of patients, which is an essential factor to determine the success of the rehabilitation, in turn; it determines the outcome of the injury or the surgery. On the other hand, there are still obstacles in its utilization in rehabilitation. Patients should be well-instructed before being prescribed with programme using virtual reality. Up to now, there is no high-level evidence supporting the use of virtual reality in rehabilitation. Further research is encouraged in this field in order to provide a better understanding of its effectiveness. In summary, using virtual reality in rehabilitation has shown early success, however, there are still challenges and questions to be explored.
References
- Pribicevic M (2012) The epidemiology of shoulder pain: A narrative review of the literature. Pain in Perspective.
- Gackenbach J, Bown J (2017) Boundaries of self and reality online: Implications of digitally constructed realities. Academic Press-an imprint of Elsevier, London.
- Lim SG, Jung SH, Huh JH (2021) Visual algorithm of VR E-sports for online health care. Healthcare 9: 824.
[Crossref] [Google Scholar] [Indexed]
- Santos FV, Yamaguchi F, Buckley TA, Caccese JB (2020) Virtual reality in concussion management: from lab to clinic. J Clin Transl Res 5: 148-154.
[Crossref] [Google Scholar] [Indexed]
- Weiss PL, Rand D, Katz N, Kizony R (2004) Video capture virtual reality as a flexible and effective rehabilitation tool. J Neuroeng Rehabil 1: 12.
[Crossref] [Google Scholar] [Indexed]
- Lin DH, Lin YF, Chai HM, Han YC, Jan MH (2007) Comparison of proprioceptive functions between computerized proprioception facilitation exercise and closed kinetic chain exercise in patients with knee osteoarthritis. Clin Rheumatol 26: 520-528.
[Crossref] [Google Scholar] [Indexed]
- Simsek TT (2019) The effectiveness of virtual reality in the rehabilitation of balance and gait in children with cerebral palsy: Mini-review. Am J Biomed Sci & Res
[Crossref] [Google Scholar] [Indexed]
- Liliana BM, Javier ES (2020) Rehabilitation system using virtual reality techniques and video games to improve postural control in people with acquired brain injury. J. Xi'an Univ Archit amp Technol 12: 874-879.
- Soltani P, Andrade R (2020) The influence of virtual reality head-mounted displays on balance outcomes and training paradigms: A systematic review. Front Sports Act Living 2: 531-535.
[Crossref] [Google Scholar] [Indexed]
- Tripette J, Murakami H, Ryan KR, Ohta Y, Miyachi M (2017) The contribution of Nintendo Wii Fit series in the field of health: A systematic review and meta-analysis. Peer J 5: 3600.
[Crossref] [Google Scholar] [Indexed]
- Kosik KB, McCann RS, Terada M, Gribble PA (2017) Therapeutic interventions for improving self-reported function in patients with chronic ankle instability: A systematic review. Br J Sports Med; 51: 105-112.
[Crossref] [Google Scholar] [Indexed]
- Doherty C, Bleakley C, Delahunt E, Holden S (2017) Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br J Sports Med; 51: 113-125.
[Crossref] [Google Scholar] [Indexed]
- Lin H, Han K, Ruan B (2021) Effect of virtual reality on functional ankle instability rehabilitation: A systematic review. J Healthc Eng.
[Crossref] [Google Scholar] [Indexed]
- Gumaa M, Rehan YA (2019) Is virtual reality effective in orthopedic rehabilitation? A systematic review and meta-analysis. Phys Ther 99: 1304-1325.
[Crossref] [Google Scholar] [Indexed]
- Westby MD, Brittain A, Backman CL (2014) Expert consensus on best practices for post-acute rehabilitation after total hip and knee arthroplasty: A Canada and United States delphi study. Arthritis Care Res 66: 411-423.
[Crossref] [Google Scholar] [Indexed]
- Gianola S, Stucovitz E, Castellini G (2020) Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: A randomized controlled trial. Medicine 99: 19136.
[Crossref] [Google Scholar] [Indexed]
- Chen J (2021) Clinical effect of virtual reality technology on rehabilitation training of sports injury. J Healthc Eng 2021.
[Crossref] [Google Scholar] [Indexed]
- Grooms D, Appelbaum G, Onate J (2015) Neuroplasticity following anterior cruciate ligament injury: A framework for visual-motor training approaches in rehabilitation. J Orthop Sports Phys Ther 45: 381-393.
[Crossref] [Google Scholar] [Indexed]
- Hewett TE, Di Stasi SL, Myer GD (2013) Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med 41: 216-224.
[Crossref] [Google Scholar] [Indexed]
- Foissey C, Thaunat M, Bondoux L, Sonnery CB, Fayard JM (2021) Self-rehabilitation guided by a mobile application after anterior cruciate ligament reconstruction leads to improved early motion and less pain. Arthrosc Sports Med Rehabil 3: 1457-1464.
[Crossref] [Google Scholar] [Indexed]
- Baltaci G, Harput G, Haksever B, Ulusoy B, Ozer H (2013) Comparison between nintendo wii fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surg Sports Traumatol Arthrosc 21: 880-887.
[Crossref] [Google Scholar] [Indexed]
- Adam LH, Cody RC, HoWon K, Tim W, Dustin RG (2020) Neuroplastic multimodal ACL rehabilitation: Integrating motor learning, virtual reality, and neurocognition into clinical practice. Aspetar Sports Medicine Journal.
- Walden M, Hagglund M, Magnusson H, Ekstrand J (2016) ACL injuries in men's professional football: A 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med 50: 744-750.
[Crossref] [Google Scholar] [Indexed]
- Nwachukwu BU, Adjei J, Rauck RC (2019) How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? A systematic review. Orthop J Sports Med; 7.
[Crossref] [Google Scholar] [Indexed]
- Margot Putukian(2017)Psychological issues related to illness and injury in athletes and the team physician: A consensus statement-2016 Update. Curr Sports Med Rep 16: 189-201.
[Crossref] [Google Scholar] [Indexed]
- Harrison K, Potts E, King AC, Braun TR (2021) The effectiveness of virtual reality on anxiety and performance in female soccer players. Sports 9: 167.
- Wilson MR, Wood G, Vine SJ (2009) Anxiety, attentional control, and performance impairment in penalty kicks. J Sport Exerc Psychol 31: 761-775.
[Crossref] [Google Scholar] [Indexed]
- Sekiya H, Tanaka Y (2019) Movement modifications related to psychological pressure in a table tennis forehand task. Percept mot skills 126: 143-156.
[Crossref] [Google Scholar] [Indexed]
- Bedir D, Erhan SE (2020) The effect of virtual reality technology on the imagery skills and performance of target-based sports athletes. Front Psychol 11: 2073.
[Crossref] [Google Scholar] [Indexed]
- Akbas A, Marszalek W, Kamieniarz A, Polechonski J, Slomka KJ et al. (2019) Application of virtual reality in competitive athletes - A review. J Hum Kinet 69: 5-16.
- Smits M, Staal JB, Goor VH (2020) Could virtual reality play a role in the rehabilitation after covid-19 infection? BMJ Open Sport Exerc Med 6: 943.
[Crossref] [Google Scholar] [Indexed]
- Reason JT (1978) Motion sickness adaptation: A neural mismatch model. J R Soc Med 71: 819-829.
[Crossref] [Google Scholar] [Indexed]
- Slobounov S, Slobounov E, Newell K (2006) Application of virtual reality graphics in assessment of concussion. Cyberpsychol Behav 9: 188-191.
[Crossref] [Google Scholar] [Indexed]
- Deutsch JE, Brettler A, Smith C (2011) Nintendo wii sports and wii fit game analysis, validation, and application to stroke rehabilitation. Top Stroke Rehabil 18: 701-719.
[Crossref] [Google Scholar] [Indexed]
- Kuroda Y, Young M, Shoman H, Punnoose A, Norrish AR et al. (2021) Advanced rehabilitation technology in orthopaedics- A narrative review. Int Orthop 45:1933-1940.
[Crossref] [Google Scholar] [Indexed]
- Obdrzalek S, Kurillo G, Ofli F (2012) Accuracy and robustness of kinect pose estimation in the context of coaching of elderly population. Annu Int Conf IEEE Eng Med Biol Soc 1188-1193.
[Crossref] [Google Scholar] [Indexed]
- Da Gama A, Fallavollita P, Teichrieb V, Navab N (2015) Motor rehabilitation using kinect: A systematic review. Games Health J 4: 123-135.
[Crossref] [Google Scholar] [Indexed]
- Wochatz M, Tilgner N, Mueller S (2019) Reliability and validity of the Kinect V2 for the assessment of lower extremity rehabilitation exercises. Gait Posture 70: 330-335.
[Crossref] [Google Scholar] [Indexed]
- Monroe CM (2009) The effects of therapeutic touch on pain. J Holist Nurs 27: 85-92.
[Crossref] [Google Scholar] [Indexed]
- So PS, Jiang Y, Qin Y (2008) Touch therapies for pain relief in adults. Cochrane Database Syst Rev 4.
[Crossref], [Google Scholar] [Indexed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi