Case Report, Clin Oncol Case Rep Vol: 3 Issue: 1
Volumetric Modulated Arc Radiotherapy for Resected HighGrade Costal Chondrosarcoma with Positive Margins: A Case Report and Review of Literature
Gadea J*, Ortiz I, Maturana JE, Garcia C and Pardo J
Radiation Oncology Department, Hospital Universitari Son Espases, Palma de Mallorca, Spain
*Corresponding Author : Jon Gadea Quinteiro
Radiation Oncology Department, Hospital Universitari Son Espases, Palma de Mallorca, Carretera de Valldemossa 79, 07120 Palma, Illes Balears, Spain
Tel: +34653448972
E-mail: Jongadea@gmail.com
Received: January 17, 2020 Accepted: January 23, 2020 Published: February 03, 2020
Citation: Gadea J, Ortiz I, Maturana JE, Garcia C, Pardo J (2020) Volumetric Modulated Arc Radiotherapy for Resected High-Grade Costal Chondrosarcoma with Positive Margins: A Case Report and Review of Literature. Clin Oncol Case Rep 3:1.
Abstract
Chondrosarcomas are cartilage-matrix-forming tumors that make up 30% of primary malignant bone tumors and are the third most common primary bone malignancy after multiple myelomas and osteosarcomas. Although wide en bloc surgical excision offers the best chance for a cure, achieving negative surgical margins can be challenging because of the high morbidity of surgery in different anatomic areas. Therefore, adjuvant radiation therapy plays an important role in improving the local control rate when negative margins are not achieved. However, delivery of a sufficient dose of radiation can be difficult because of the proximity to normal organs/tissues that are sensitive to radiation therapy and therefore dose-limiting. New techniques such as Volumetric Modulated Arc Therapy (VMAT) allow us to achieve an optimal conformation of the radiation beam, avoiding healthy organs and minimizing the undesirable acute and chronic side effects. We report a case of costal chondrosarcoma with positive post-surgery margins treated with adjuvant radiation therapy using VMAT technique that appears free of disease two years after finishing radiation therapy with a mild asymptomatic radiation-induced pneumonitis as the only late side effect.
Keywords: Chondrosarcoma; Chest wall; Radiotherapy; VMAT
Introduction
Chondrosarcomas (CS) are rare mesenchymal tumors with a cartilage-like appearance. They are almost one-third of all malignant bone tumors [1] and the third most common primary bone malignancy after multiple myeloma and osteosarcoma [2]. Unlike other bone sarcomas, conventional and dedifferentiated CS have their peak incidence at the ages of 40-70 years [3-5], so CS is the most frequently occurring bone sarcoma in adulthood. The 5-years Overall Survival (OS) for low grade CS is 83% while for intermediate/high grade CS is 53% [3]. Fortunately, most CS arises as conventional, primary, low grade, locally aggressive, non-metastasizing tumors rather than high-grade tumors.
Due to their hypo vascularity and slow mitotic activity, CS is distinguished for its resistance to chemotherapy and radiation therapy (RT) [4]. Therefore, wide en bloc surgical excision offers the best chance for a cure, especially for Grade II or III CS [5]. However, the location of these tumors makes it sometimes difficult to achieve a radical surgical excision because of the high morbidity of surgery in different anatomic areas such as the pelvis, skull base, and spine or chest wall. Thus, RT alone or combined with surgery, plays an important role in achieving local control (LC) in these “high risk” situations [6].
For This Reason, The Use Of New RT Techniques Such As Intensity-Modulated Radiation Therapy (IMRT) And Volumetric Modulated Arc Therapy (VMAT) is essential, allowing radiation oncologists to deliver higher radiation dose into the neoplasia with safer preservation of neighboring healthy organs [7].
Clinical case
A 54-year-old Caucasian female with no history of previous cancer presented with left-side chest pain for six months. The pain was more intense with deep inspiration and was partially calmed with ibuprofen. No weight loss, hemoptysis, cough or other symptoms were presented. The patient was admitted to the pneumolo Gy service for further management and diagnosis.
Chest radiography revealed a round well-defined mass in the upper lobule of the left lung (Figure 1). A blood test was made and the results were anodyne. A Computerized Tomography (CT) of the chest revealed an intrathoracic extra-pulmonary tumor of 5 × 6 centimeters (cm) in the sixth left costal arc (Figure 1). A CT-guided
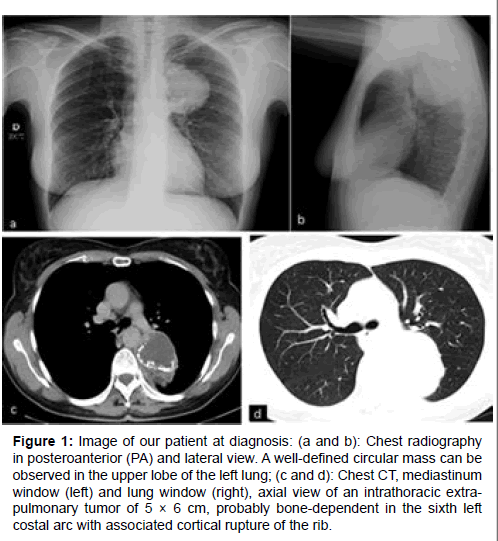
Figure 1: Image of our patient at diagnosis: (a and b): Chest radiography in posteroanterior (PA) and lateral view. A well-defined circular mass can be observed in the upper lobe of the left lung; (c and d): Chest CT, mediastinum window (left) and lung window (right), axial view of an intrathoracic extrapulmonary tumor of 5 × 6 cm, probably bone-dependent in the sixth left costal arc with associated cortical rupture of the rib.
Fine Needle Biopsy (FNB) revealed not enough material for diagnosis was obtained, so the patient was transferred to the thoracic surgery service.
Thoracic surgeons performed a left-back thoracotomy with subtotal resection of the mass. The extracted material was analyzed by de pathologist revealing a sixth left costal arc Grade III CS, with 30% of necrosis, positive surgical margins and invasion of rib bone marrow and residual parietal pleura.
After the surgery, the case was discussed in the multidisciplinary tumor board of bone and soft tissue tumors formed by orthopedic and thoracic surgeons, medical oncologists, radiation oncologists, pathologists and radiologists. The decision of the board was to complete local treatment with adjuvant RT because of the high-grade histolo Gy and the positive surgical margins.
The patient received daily External Beam Radiation Therapy (EBRT) in a Varian Clinac Rapid Arc accelerator (Varian medical system, Palo Alto, CA, USA). The technique used was Volumetric Modulated Arc Therapy (VMAT) with four dynamic coplanar arcs delivering a total dose of 66 Gy to the surgical bed in 33 fractions using 6 MV photon ener Gy. Image-Guided Radiation Therapy (IGRT) using Cone-beam CT (CBCT) was used for daily treatment. The prescribed dose was 66 Gray ( Gy) given at 2 Gy per fraction over 33 daily fractions to the surgical bed with margins and the normal tissue constraints used were QUANTEC.
The department of medical physics made two plans for the same treatment, using 3D EBRT and VMAT techniques. As we can see in Table 1, VMAT spares more doses to normal tissue compared with 3D EBRT, which is essential in order to avoid late toxicity in our patients.
Table 1: QUANTEC review on dose/volume tolerance for heart, lung, esophagus and spinal cord. Patient data (VMAT treatment and the comparison with 3D EBRT) are shown at the right side of the table.
The follow up was done every month for the first three months, and then every three months. One month after finishing RT a new thoracic CT showed no evidence of disease (Figure 2). At the sixth month check-up, the patient presented dry cough and occasional mild coastal pain with no need of taking medication and no other accompanying symptoms. A new thoracic CT revealed no evidence of disease (Figure 2) and confirmed mild radiation-induced pneumonitis as the only late RT side effect at that moment. Currently, the patient is asymptomatic and disease-free two years after finishing RT.
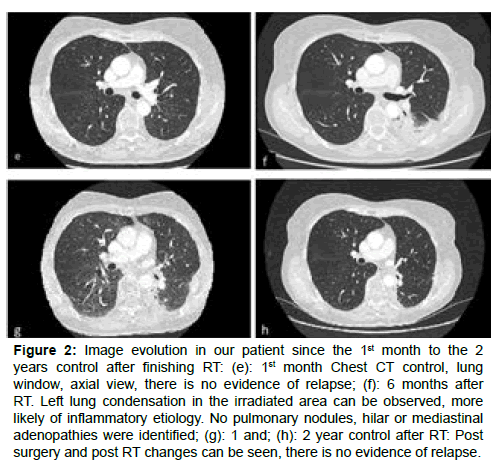
Figure 2: Image evolution in our patient since the 1st month to the 2 years control after finishing RT: (e): 1st month Chest CT control, lung window, axial view, there is no evidence of relapse; (f): 6 months after
RT. Left lung condensation in the irradiated area can be observed, more likely of inflammatory etiology. No pulmonary nodules, hilar or mediastinal adenopathies were identified; (g): 1 and; (h): 2 year control after RT: Post surgery and post RT changes can be seen, there is no evidence of relapse.
Discussion
Although they can be considered as a rare entity, CS should be among the leading differential diagnoses in any symptomatic patient who presents with chest wall pain and a palpable mass on clinical exam or a visible mass seen radiographically. CS is the most common malignant tumor of the chest wall [8]. In addition to plain radiography, CT and Magnetic Resonance (MR) scans should be obtained to better characterize the tumor. A polylobulated mass with surrounding bone destruction and an intralesional calcified chondroid matrix are distinguishing features of CS on CT imaging. MR reveals hyperintensity on T2- weighted images, reflecting the high water content of CS [9].
Respecting the treatment with curative intent, adequate LC through complete tumor removal is an important therapeutic goal. However, in managing CS, a multidisciplinary approach is extremely important to optimize treatment outcomes. While the primary aim of a multidisciplinary approach would favor a complete resection, when technically achievable with acceptable morbidity, this is often not possible. Usually, these tumors arise in axial locations, needing the use o f alternative strategies in order to achieve the highest possible LC optimizing function and quality of life [10].
Bergh et al. [11] published the following predictive factors of Local Recurrence (LR): inadequate surgical margins, incisional biopsy, primary surgery outside of a tumor center, increasing patient age and higher histolo Gy grade, correlated to significantly worse survival and local disease control. En bloc resection leads to a greater LC according to Boriani et al. [12]. of 13 patients treated with en bloc resection with a median follow-up of 2-236 months (average 81 months), only 1 patient experienced local failure. This differs from the 21 patients that underwent intralesional resection, in which only 1 patient experienced local disease controls. Widhe et al. [13] from the Scandinavian Sarcoma Group studied 106 consecutive patients with chest wall CS with a median of nine years follow-up. Patients who had wide surgical resection had a 10-year survival of 92% compared with 47% for those who had an intralesional resection. Talac et al. [14] studied the relationship between surgical margins and LR in 30 patients with sarcomas of the spine. According to their results, a clear relationship between LC and OS was found. In their study, more than 90% of the patients with LR died at an average of 16, 6 months after diagnosis of recurrence. Evans et al. [15] examined the relationship between histopatholo Gy and tumor behavior in 71 cases of CS. The tumors were grouped into Grades I, II, and III on the basis of mitotic rate, cellularity, and nuclear size. The five-year survival rates of Grades I, II, and III were 90%, 81%, and 43%, respectively, while the corresponding 10-year survival rates were 83%, 64%, and 29%. None of the Grade I CS metastasized, while metastasis was observed with 10% of the Grade II tumors and 71% of the Grade III tumors. No definite relationship between tumor grade and LR was found, so the rate of LR seems to be primarily dependent on the adequacy of surgical therapy rather than histologic grade.
RT plays an important role when negative margins (R0) resections are not achieved in order to improve local disease control. Goda et al. [10] reported 60 patients with a diagnosis of extracranial CS who were treated with surgery and RT (preoperative RT median dose of 50 Gy and postoperative RT median dose of 60 Gy were delivered in 40% and 60% of the patients, respectively). Surgical margin status played an important role in LC rates. R0, positive microscopical margins (R1), positive macroscopical margins (R2) resections had LC of 100%, 94% and 42%, respectively. Preoperative RT was delivered to patients with a high probability of having positive margins or subtotal resection. The timing of RT (preoperative vs. postoperative) did not result in a statistically significant difference in PFS. Tumor grade was a statistically significant prognostic factor for OS (p<0.009). The addition of RT as an adjuvant treatment to surgery appears promising. High rates of LC of the primary spine and sacral CS have been reported in the context of en bloc resections in conjunction with RT [1]. However, there is no consensus in the RT dose that has to be delivered in order to achieve an optimal LC and to preserve the function of neighboring healthy organs. De Laney et al. [16] investigated the efficacy of RT in soft-tissue sarcomas (STS) patients with positive margins. From the 131 patients who received only external beam radiation, 70 patients received <64 Gy and 61 received >64 Gy. Radiation doses higher than 64 Gy were associated with improved LC, disease-free survival (DFS), and OS. LC at 5 years for patients receiving doses <64 Gy was 66.1 ± 5.7%, whereas it was 85 ± 4.4% for those who received doses >64 Gy (p=0.01). By ten years, it was 67.8 ± 6.3% vs. 82.8 ± 5.3% (p=0.055), respectively.
Technological advances in RT such as the development of IMRT, VMAT, SRS (stereotactic radiosurgery), carbon ion therapy, and proton therapy enable better dose conformality and sparing radiation to normal organs/tissues. Thus, currently, it is possible for radiation oncologists to deliver the required high dose of radiation to provide LC in CS treatments, either in the adjuvant or in the radical setting [10].
In our patient, the treatment decision was based following the Scandinavian Sarcoma Group´s recommendations [17]. The patient received 66 Gy in the surgical bed over 33 fractions with IMRT technique using VMAT and daily IGRT. This technique allowed us to achieve an optimal conformation of the radiation beam, avoiding healthy organs and minimizing the undesirable acute and chronic side effects. We based our treatment planning on the Quantitative Analysis of Normal Tissue Effects in the clinic (QUANTEC) review, which summarizes the currently available three-dimensional dose/ volume-outcome data updating and refining the normal tissue dose/ volume tolerance guidelines provided by the classic Emami et al. paper published in 1991 [18].
The future probable chronic side effects of the RT treatment must be considered when deciding the ideal treatment planification for every patient. Acute radiation pneumonitis occurs in the majority of cases between six and twelve weeks after the end of thoracic radiotherapy. This phase is usually asymptomatic. In our patient, a dry cough and occasional mild costal pain were the only symptoms and no specific treatment was needed. Pulmonary fibrosis occurs approximately 6 months after the end of thoracic radiotherapy. It is a virtually constant radiological feature that stabilizes two years after the end of treatment. Its most common clinical manifestation is bronchiectasis. It can arise in the absence of acute pneumonia. There are several levels of late pulmonary toxicity (SOMA-LENT, CTCAE, RTOG-EORTC) with variations in therapeutic behavior from one level to another making it difficult to compare the different studies according to the rate and grade of pneumonia observed [19]. According to this, a close followup of our patient should be done with the aim of early recognition of pulmonary toxicity and early treatment instauration. Currently, 12 months after RT finished, no clinical signs of pulmonary fibrosis are observed in our patient [20].
Conclusion
In conclusion, high-grade CS continues to be a poor prognostic disease, especially when negative margins are not achieved. RT plays an important role in these cases, helping to improve LC. New radiation techniques such as IMRT and VMAT allow us to give a higher radiation dose with a better beam conformation and homogeneity, which traduces in better disease control with fewer side effects compared with conventional EBRT. In our patient, no evidence of LR or distant progression was observed after 24 months follow-up. However, OS at 5 years in high-grade CS continues to be around 50%, so improving cure rates remains a huge challenge for both surgeons and radiation oncologists. New treatment advances are required to improve these outcomes.
References
- Polychronidou G, Karavasilis V, Pollack SM, Huang PH, Lee A, et al. (2017) Novel therapeutic approaches in chondrosarcoma. Future Oncol 13: 637-648.
- Dorfman HD, Czerniak B (1995) Bone cancer. ACS Journals 75: 203-210.
- Grimer RJ, Gosheger G, Taminiau A, Biau D, Matejovsky Z, et al. (2007) Dedifferentiated chondrosarcoma: Prognostic factors and outcome from a european group. Eur J Cancer 43: 2060-2065.
- Gelderblom H, Hogendoorn PC, Dijkstra SD, Rijswijk CS, Krol AD, et al. (2008) The clinical approach towards chondrosarcoma. Oncologist 13: 320-329.
- Murphey MD, Walker EA, Wilson AJ, Kransdorf MJ, Temple HT, et al. (2003) From the archives of the AFIP: Imaging of primary chondrosarcoma: Radiologic-pathologic correlation. Radiographics 23: 1245-1278.
- Zagars GK, Ballo MT (2003) Significance of dose in postoperative radiotherapy for soft tissue sarcoma. Int J Radiat Oncol Biol Phys 56: 473-481.
- Kepka L, DeLaney TF, Suit HD, Goldberg SI (2005) Results of radiation therapy for unresected softtissue sarcomas. Int J Radiat Oncol Biol Phys 63: 852-859.
- Rascoe PA, Reznik SI, Smythe WR (2011) Chondrosarcoma of the thorax. Sarcoma 1-7.
- Littrell LA, Wenger DE, Wold LE, Bertoni F, Unni KK, et al. (2004) Radiographic, CT, and MR imaging features of dedifferentiated chondrosarcomas: A retrospective review of 174 de novo cases. Radiographics 24: 1397-1409.
- Goda JS, Ferguson PC, O'Sullivan B, Catton CN, Griffin AM, et al. (2011) High-risk extracranial chondrosarcoma: Long-term results of surgery and radiation therapy. Cancer 117: 2513-2519.
- Bergh P, Gunterberg B, Meis-Kindblom JM, Kindblom LG (2001) Prognostic factors and outcome of pelvic, sacral, and spinal chondrosarcomas: A center-based study of 69 cases. Cancer 91: 1201-1212.
- Boriani S, De Iure F, Bandiera S, Campanacci L, Biagini R, et al. (2000) Chondrosarcoma of the mobile spine: Report on 22 cases. Spine 25: 804-812.
- Widhe B, Bauer HC (2009) Scandinavian sarcoma group: Surgical treatment is decisive for outcome in chondrosarcoma of the chest wall: A population-based Scandinavian sarcoma group study of 106 patients. J Thorac Cardiovasc Surg 137: 610-614.
- Talac R, Yaszemski MJ, Currier BL, Fuchs B, Dekutoski MB, et al. (2002) Relationship between surgical margins and local recurrence in sarcomas of the spine. Clin Orthop Relat Res 397: 127-132.
- Evans HL, Ayala AG, Romsdahl MM (1977) Prognostic factors in chondrosarcoma of bone: A clinicopathologic analysis with emphasis on histologic grading. Cancer 40: 818-831.
- Delaney TF, Kepka L, Goldberg SI, Hornicek FJ, Gebhardt MC, et al. (2007) Radiation therapy for control of soft-tissue sarcomas resected with positive margins. Int J Radiat Oncol Biol Phys 67: 1460-1469.
- Scandinavian Sarcoma Group (2015) SSG XXIV Recommendations for radiotherapy in bone and soft tissue sarcoma. Version 1.
- Marks LB, Yorke ED, Jackson A, Ten Haken RK, Constine LS, et al. (2010) Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys 76: 10-19.
- Chargari C, Riet F, Mazevet M, Morel E, Lepechoux C, et al. (2013) Complications of thoracic radiotherapy. Presse Med 42: 342-351.
- Folkert MR, Singer S, Brennan MF, Kuk D, Qin LX, et al. (2014) Comparison of local recurrence with conventional and intensity-modulated radiation therapy for primary soft-tissue sarcomas of the extremity. J Clin Oncol 32: 3236-3241.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 