Short Communication, J Sleep Disor Vol: 8 Issue: 1
A New FDA Cleared Expiratory Resistance Device for Treatment of Snoring and Low Levels of Obstructive Sleep Apnea
Hakim TS* and Camporesi EM
Sleep Apnea Treatment Center, Phoenix, AZ and University of South Florida, TEAMHealth Anesthesia, Tampa, FL, USA
*Corresponding Author: Hakim TS
PhD Sleep Apnea Treatment Center, 10443 N Cave Creek Road, Suite 110, Phoenix, Arizona 85020, USA
Tel: (602) 944-0847
E-mail: salthakim@yahoo.com
Received: 31 October, 2018 Accepted: 18 November 2018 Published: 25 November 2018
Citation: Hakim TS, Camporesi EM (2018) A New FDA Cleared Expiratory Resistance Device for Treatment of Snoring and Low Levels of Obstructive Sleep Apnea. J Sleep Disor Treat Care 7:4. doi: 10.4172/2325-9639.1000222
Abstract
Expiratory Positive Airway Pressure (EPAP) devices have been successfully used to treat obstructive sleep apnea and snoring. A new EPAP device called “Optipillows EPAP Mask” has recently been cleared by the FDA for treatment of snoring. The goal of this study is to describe the new EPAP mask and characterize its resistance properties. The EPAP mask consists of a nasal pillow type mask with head straps and with a proprietary micro valve on the front of it. The EPAP mask allows inhalation with minimal resistance, but with more resistance during exhalation causing the pressure to be elevated. The expiratory resistance can be adjusted according to patient’s comfort. The pressure generated by the EPAP mask was evaluated using a breathing system that simulated normal breathing pattern at rest. With the expiratory resistance fully open (minimal resistance) peak expiratory pressure generated by the mask was 1.3 to 3.2 cm H2O depending on tidal volume. A larger tidal volume generated more pressure during expiration. Peak expiratory pressure increased as the expiratory resistance was increased. The expiratory resistance range of the EPAP mask is comparable to previous EPAP devices. EPAP devices have limitations. A patient must take as long as necessary to learn to sleep comfortably with low resistance on the EPAP mask, before rushing to increase the resistance. For treatment of snoring a low level of expiratory resistance may be sufficient. The EPAP mask may also be useful for treatment of low levels of obstructive sleep apnea.
Keywords: EPAP devices; EPAP mask; Expiratory resistance; Snoring and obstructive sleep apnea
Introduction
Snoring and Obstructive sleep apnea (OSA) are categorized as sleep disordered breathing (SDB) and together affect more than 25% of the adult population. SDB is caused by narrowing or collapse of the pharyngeal airway during sleep because of tissue crowding and reduced muscle tone. Partial obstruction of the upper airway leads to noise (snoring) created by air turbulence, while complete obstruction leads to the total cessation of airflow (obstructive sleep apnea). SDB is treated with the use of continuous positive airway pressure (CPAP) therapy which is generally well accepted by patients. CPAP provides positive pressure during the entire breathing cycle. In general it is thought that CPAP provides a stent like action which prevents the upper airways from collapsing [1,2]. In 1983, Mahadevia et al. [3], showed that the positive pressure during inspiration is not necessary to treat OSA, but a positive pressure during expiration in itself is adequate to prevent OSA. Such study lead to the introduction of the EPAP devices to treat snoring and OSA [4-9]. Current EPAP devices including Provent and Theravent, cleared by the FDA, have small valves that allow air to be inhaled with minimal resistance through each nostril, but during exhalation, air exits through a narrow opening with considerably more resistance. EPAP devices do not replace CPAP therapy but provide a new choice for patients who refuse to use CPAP or for more convenience during travel. EPAP devices have indeed been hailed as a great addition to the tools that are available to treat patients with SDB [10-12]. This is not surprising because at end expiration, upper airway is narrowest and most susceptible to collapse [13,14]. More recently a new EPAP mask designed as an expiratory resistance device was cleared by the FDA. The new EPAP mask is called “Optipillows EPAP Mask”, and consists of a nasal pillow type mask with a proprietary micro-valve that allows the user to inhale with minimal resistance and exhale against elevated resistance. The new EPAP mask is secured in place against the nostrils using light and comfortable head straps that can be adjusted to provide comfort while providing a seal against the nostrils. During normal breathing without EPAP device, inspiratory effort causes the pressure to become slightly negative potentially leading to upper airway collapse, causing the snoring noise or the sleep apnea. When an EPAP device is used, the pressure during expiration remains positive, stabilizing the upper airways and preventing or reducing any potential collapse that may occur when inspiration is initiated. The goal of this study is to describe the new EPAP mask and characterize the pressure that it generates.
Materials and Methods
Description of the EPAP mask and how it works
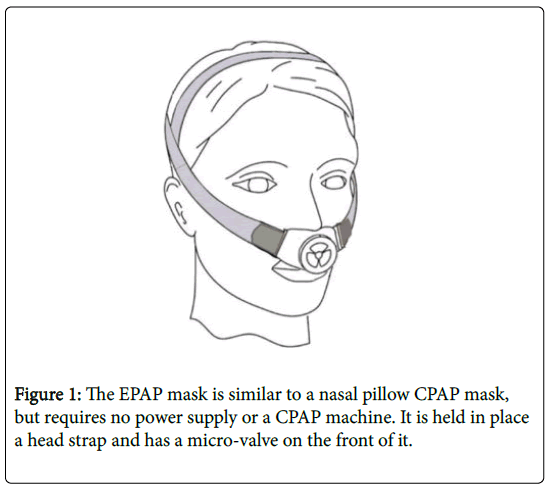
The new EPAP mask is an expiratory resistance device cleared by the FDA. The EPAP mask uses nasal pillows and is worn like a nasal pillow CPAP mask (Figure 1). The EPAP mask does not require a power supply and does not need to be connected to a CPAP machine. The EPAP mask has a proprietary valve on the front of the mask (Figure 2) that allows the patient to inhale with minimal resistance but creates some resistance during exhalation. The increased resistance generates positive pressure during exhalation, increasing the back pressure in the pharyngeal region and preventing upper airway obstruction. The increased pressure during exhalation alleviates snoring and obstructive sleep apnea.
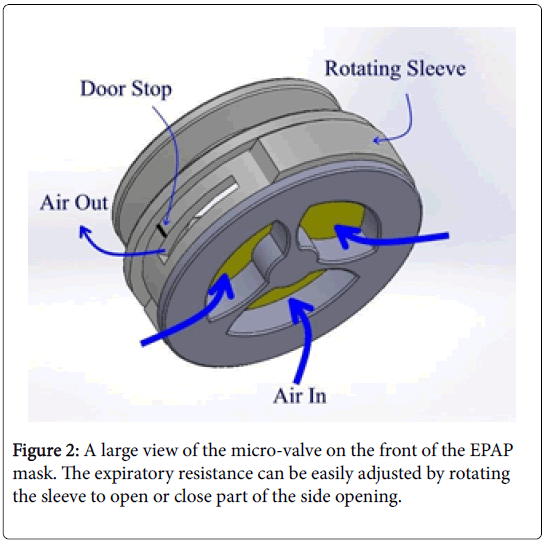
A larger view of the valve on the front of the EPAP mask is shown in Figure 2. During inhalation, air flows with minimal resistance through the large opening passing by a diaphragm on the front of the valve. During exhalation the diaphragm closes the large opening on the front of the valve and redirects air flow through a small opening on the side of the valve. The air flow through the small opening creates back pressure in the nose and throat alleviating upper airway obstruction. The resistance during exhalation can be adjusted by rotating the sleeve (Figure 2) to cover or uncover the side opening. The valve has a little “door stop” to prevent complete closure of the side opening by the rotating sleeve.
In summary, the EPAP mask is a modified nasal pillow CPAP mask with an expiratory resistance. Nasal pillow CPAP mask have been successfully used for many years without notable problems. Expiratory resistance devices such as Provent and Theravent have also been used for a few years to treat snoring and OSA with considerable measure of success [1-3]. The EPAP mask is likely to be as effective as previous EPAP devices but may be more comfortable for some patients. The low expiratory resistance on the EPAP mask provides a feeling of nearly normal breathing. The expiratory resistance can be well controlled and adjusted quickly and reliably over a wide range simply by rotating the sleeve on the valve in small steps. The expiratory resistance of the EPAP mask was designed to be comparable to the resistance in previous EPAP devices such as Provent or Theravent.
How much pressure does the EPAP mask generate during breathing?
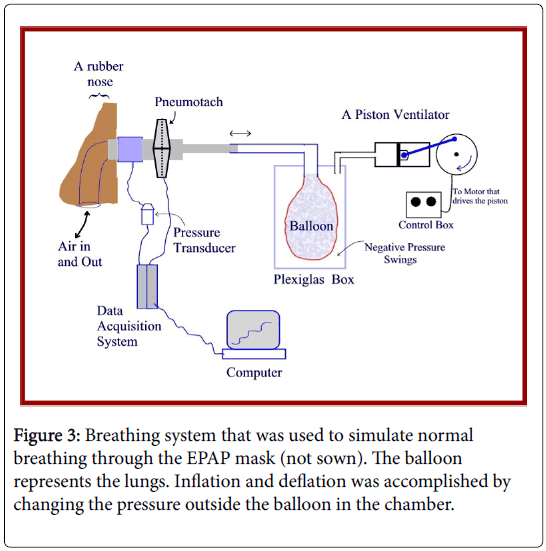
The operation of the EPAP mask was tested while connected to a breathing system shown in Figure 3. The EPAP mask (not shown in the figure) was applied on the plastic rubber nose with two nostrils and the mask was secured in place against the nostrils like it would be during normal use. The breathing system was designed to simulate normal breathing pattern at rest in terms of the volume of air flowing through the valve, in terms of frequency of breathing, in terms of the volume of air in and out of the lungs (tidal volume), and in terms of peak flow rate. This was accomplished by using a vacuum Plexiglas chamber in which a balloon (A respiratory breathing balloon) was suspended from the top of the chamber. A Harvard animal respirator (Harvard Apparatus Model 613 Dual Phase respirator) was connected to the chamber to generate negative pressure swings in the chamber causing inflation and deflation of the balloon. The swings in negative pressure in the chamber were adjusted to provide a volume of air in and out of the balloon of approximately 300 or 500 ml, which represents the normal range of tidal volume in adult humans. The frequency of the pressure swings in the chamber was set to provide a normal frequency of breathing of 15 breaths per minute. The pressure was measured from a side port near the nose using a pressure transducer (Grass Instruments, Warwick, RI). The signal from the pressure transducer was fed through a data acquisition system (Biopac Systems UM100A, Goleta, CA), and displayed on a computer monitor. The flow rate signal was recorded using a pneumotach (TSD117, Biopac Systems, Goleta, CA) and the flow rate was integrated as recommended by the manufacturer and recorded on a third channel to provide a tracing of the tidal volume in and out of the balloon and the EPAP mask. Calibration and verification of the pressure, flow rate, and volume measurement were done at the beginning of each experiment. The data were recorded and stored on the computer.
Results
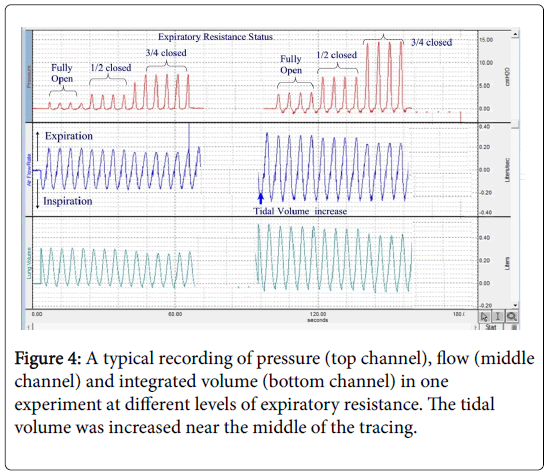
After completing the calibration of the flow and pressure sensors, the respirator was started to simulate normal breathing with the bidirectional cyclic flow through the EPAP mask. The negative pressure swings in the Plexiglas chamber were generated by the piston ventilator which was adjusted to provide a volume in and out of the chamber of approximately 300 ml. The expiratory resistance of the EPAP mask was adjusted by rotating the sleeve to increase or decrease the expiratory resistance. First, the valve was fully open, then it was 50% closed and 75% closed, and then back to fully open. The negative pressure swings in the Plexiglas chamber were then increased to provide a larger tidal volume of 500 ml. The resistance of EPAP mask was then increased as before with the valve closed at 50% and 75%, and pressure and flow signals were recorded at each resistance setting. The volumes that were used represent average tidal volume in most adults during normal breathing at rest; 300 ml would represent a person with a small tidal volume while a 500 ml would represent a person with a larger tidal volume. Furthermore, such volumes generated peak flow during breathing which is typical for most adults during normal breathing at rest.
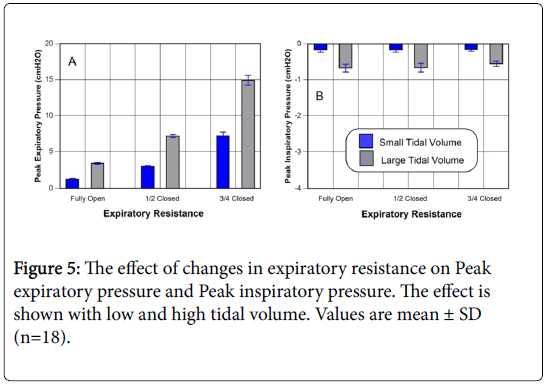
Figure 4 shows typical tracings during a simulated breathing at different tidal volumes and different expiratory resistances. The pressure that was measured just upstream from the nose represents the pressure in the pharyngeal region in the back of the mouth. Typical tracings are shown in the figure under different breathing conditions that represent normal breathing pattern. The tracings also show the protocol that was followed. The peak pressure during expiration and during inspiration was measured in each experiment at each resistance level. The mean values from 18 experiments on random samples of the EPAP mask are shown in Figure 5.
Peak expiratory pressure (Figure 5), Panel A generated by the EPAP mask when the expiratory resistance was fully open, was 1.3 ± 0.2 cm H2O while breathing at the low tidal volume, and 3.3 ± 0.5 cm H2O while breathing with the large tidal volume (the pair of bars on the left). These pressures would represent the peak expiratory pressure generated by a person with small size lungs, and a person with large lungs respectively. Peak expiratory pressure generated by the EPAP mask increased to 3.5 ± 0.3, and 7.2 ± 0.8 cm H2O when the resistance was 50% closed while breathing at low lung volume and large tidal volume respectively (the pair of bars in the middle). When the expiratory resistance was 75% closed, the peak expiratory pressures were 7.2 ± 1.2, and 15.2 ± 2.3 cm H2O while breathing with a small tidal and a large tidal volume respectively (the pair of bars on the right). The peak inspiratory negative pressure (Figure 5), Panel B was less than 0.2 cm H2O with low volume (0.16 ± 0.07), and less than 0.7 cm H2O (0.67 ± 0.11) while breathing at high lung volume. As expected, peak inspiratory pressure did not change as the expiratory resistance was increased.
Discussion
Clinical studies have shown that EPAP devices are safe and effective in treating snoring and OSA in many patients [4-9]. Some patients are unable to become adapted to the EPAP device [10,11]. EPAP devices have limitations and are likely to cause difficulty breathing [15]. A patient is more likely to be comfortable during sleep with an EPAP device that provides the appropriate resistance that allows nearly normal breathing. The EPAP mask allows adjustment of the expiratory resistance to facilitate adaptation. The peak expiratory pressure generated by the EPAP mask when the expiratory resistance is fully open was found to be approximately 1.3 to 3.2 cm H2O that rises at higher levels of expiratory resistance. The results in this study show that for a given resistance, a person with a small lung volume generates less pressure during expiration than a person with large lung volume. The new EPAP mask allows the patient to adjust the expiratory resistance as necessary to remain comfortable including using a low resistance during the adaptation period. Previous EPAP devices such as Provent or Theravent are fixed resistance EPAP devices and may pose problems for some patients. Realizing that a fixed resistance may be a problem for some patients, the scientists behind Theravent provided different adhesive patches that have low resistance (Theravent Lite), to facilitate adaptation. With the EPAP mask, the expiratory resistance can be adjusted simply by rotating the sleeve.
EPAP feels different from CPAP primarily because patients may feel that they need to work harder. This is particularly important during the first few days of adaptation to the EPAP device. Some patients give up on trying to use EPAP device because of such feeling. Adaptation to CPAP may be much easier because of the positive pressure support during inhalation; respiratory muscles do not need to work as hard as without CPAP. Indeed, work of breathing was reported to be less with CPAP than with EPAP [16]. EPAP devices do not provide such positive pressure support during inspiration and therefore work of breathing is not reduced like with CPAP. The EPAP mask was designed to facilitate adaptation because the expiratory pressure can be adjusted. The EPAP mask provides a range of expiratory resistance comparable to existing EPAP devices such as Theravent or Provent. For treatment of snoring a low expiratory pressure may be adequate. Guzman et al. [17] showed that snoring can be significantly alleviated with low level of CPAP therapy of 2 to 6 cm H2O. Such low pressure during expiration are generated by the EPAP mask with low level of expiratory resistance. Therefore, in some patients with snoring, it may be adequate to continue using the EPAP mask with minimal resistance (expiratory peak pressure of 1.3 to 3.2 cm H2O), but in some it may be necessary to increase the expiratory resistance slightly or perhaps up to ½ closed.
The EPAP mask provides setting of very low expiratory resistance to facilitate adaptation. Nevertheless even with such low resistance, it may take some time to become used to the EPAP mask. It is important to become fully adapted to using the EPAP mask before increasing the expiratory resistance. It is recommended that a patient use the EPAP with minimal resistance for as long as necessary until he/she becomes fully adapted and is able to fall asleep without any problem. Thereafter the resistance can be increased. If a patient cannot adapt to the EPAP mask with low resistance, it is not likely to be able to use the EPAP mask or any other EPAP device with expiratory resistance. Whether a patient prefers the EPAP mask over Provent and Theravent is a matter of choice. Provent and Theravent utilize adhesive material to affix the micro valve in the nostril and are one time use. The EPAP mask uses head straps to hold the pillows in place and can be used many times. With Provent or Theravent, if the patients feel uncomfortable, they have no choice but give up and not use the device. In contrast, the EPAP mask allows the patient to adjust the expiratory resistance to a low level, allowing time for adaptation before they have to adjust to higher levels of resistance.
Conclusion
In conclusion, the EPAP mask is an expiratory pressure device that can be useful for treating snoring and low levels of obstructive sleep apnea. The EPAP mask may require some time for adaptation. It is recommended that the expiratory resistance be kept to minimum during the training period for as long as necessary until the patient becomes totally adapted to the EPAP and is able to fall asleep without problems. Subsequently the resistance can be increased to get more effect. Closing off the expiratory resistance about half way, provides resistance comparable to Theravent regular which has been shown to be safe and effective for many patients. Thereafter the resistance can be increased or decreased as necessary to maintain comfort. Provent has a much higher expiratory resistance than Theravent, and yet some patients were able to use Provent successfully. One should not rush to thinking that a higher resistance would be much better. Too much resistance may be difficult to tolerate because it may compromise ventilation leading to CO2 retention (hypercapnia) and may disturb sleep. EPAP devices are not recommended for patients with central sleep apnea. Mouth breathers, and CPAP users using a full face mask, may have more difficulty using EPAP devices.
References
- Gordon P, Sanders MH (2005) Positive airway pressure therapy for obstructive sleep apnea/hypopnea syndrome. Thorax 60: 68-75.
- White DP (2009) Auto-PEEP to treat obstructive sleep apnea. J Clin Sleep Med 5: 538-539.
- Mahadevia AK, Onal E, Lopata M (1983) Effects of expiratory positive airway pressure on sleep-induced respiratory abnormalities in patients with hypersomnia-sleep apnea syndrome. Am Rev Respir Dis 128: 708-711.
- Berry RB, Kryger MH, Massie CA (2011) A novel nasal expiratory positive airway pressure device for the treatment of obstructive sleep apnea: a randomized controlled trial. Sleep 34: 479-485.
- Colrain IM, Brooks S, Black J (2008) A pilot evaluation of a nasal expiratory resistance device for the treatment of obstructive sleep apnea. J Clin Sleep Med 4: 426-433.
- Doshi R, Westbrook P (2012) A novel non-prescription nasal EPAP device (Theravent) to treat snoring. Sleep Diagnosis and Therapy 7: 1-5.
- Kryger MH, Berry RB, Massie CA (2011) Long term use of a nasal expiratory positive airway pressure (EPAP) device as a treatment for obstructive sleep apnea. J Clin Sleep Med 7: 449-453.
- Rosenthal L, Massie CA, Dolan DC, Loomas B, Kram J, et al. (2009) A multicenter, prospective study of a novel nasal EPAP device in the treatment of obstructive sleep apnea. Efficacy and 30-day adherence. J Clin Sleep Med 5: 532-537.
- Walsh JK, Griffin KS, Forst EH, Ahmed HH, Eisenstein RD, et al. (2011) A convenient expiratory positive airway pressure nasal device for the treatment of sleep apnea in patients non-adherent with continuous positive airway pressure. Sleep Med 12: 147-152.
- Riaz M, Certal V, Nigam G, Abdulatif J, Zaghi S, et al. (2015) Nasal Expiratory positive airway pressure devices (Provent) for OSA: A systematic review and meta-analysis. Sleep Disorders 2015: 734798.
- Wu, H, Yuan X, Zhan X, Li L (2015) A review of EPAP nasal device therapy for obstructive sleep apnea syndrome. Sleep Breath 19: 769-774.
- Schiza S, Mermigkis C, Bouloukaki I (2015) Expiratory positive airway pressure (EPAP) nasal device therapy: a welcome addition to obstructive sleep apnea syndrome therapy. Sleep Breath 19: 775-776.
- Braga CW, Chen Q, Burschtin OE, Rapoport DM, Ayappa I (2011) Changes in lung volume and upper airway using MRI during application of nasal expiratory positive airway pressure in patients with sleep disordered breathing. J Appl Physiol 111: 1400-1409.
- Morrell MJ, Arabi Y, Zahn B, Badr MS (1998) Progressive retropalatal narrowing preceding obstructive apnea. Am J Respir Crit Care Med 158: 1974-1981.
- Hakim TS, Camporesi EM (2016) Obstructive sleep apnea treatment with EPAP nasal devices: Physiological principles and limitations. J Sleep and Sleep Disorder Research 1: 33-41.
- Gherini S, Peters RM, Virgilio RW (1979) Mechanical work on the lungs and work of breathing with positive end expiratory pressure and continuous positive airway pressure. Chest 76: 251-256.
- Guzman MA, Sgambati FP, Pho H, Arias RS, Hawks EM, et al. (2017) The efficacy of low level continuous positive airway pressure for the treatment of snoring. J Clin Sleep Med 13: 703-711.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi