Case Report, Clin Oncol Case Rep Vol: 2 Issue: 1
Extra skeletal Chondroma of the Knee: A Case Report
Trong Khoan Le* and Trong Binh Le
Department of Radiology, Hue University of Medicine and Pharmacy, Hue University 06 Ngo Quyen Street, Hue, Vietnam
*Corresponding Author : Trong Binh Le
Department of Radiology, Hue University of Medicine and Pharmacy, Hue University,06 Ngo Quyen, Hue, Vietnam
Tel: 84- 905 215 096
E-mail: binhr_vn@yahoo.com.vn
Received: December 11, 2018 Accepted: January 16, 2019 Published: February 23, 2019
Citation: Le TK, Le TB (2019) Extraskeletal Chondroma of the Knee: A Case Report. Clin Oncol Case Rep 2:1.
Abstract
Extraskeletal chondromas are rare, benign, cartilaginous tumor without the involvement of periosteum or bone cortex. Characteristics of internal calcification may suggest the diagnosis. Magnetic resonance imaging is helpful in delineating tumor location and margin. Definite diagnosis should be made after correlating clinical symptoms, radiological and histopathological findings.
Keywords: Extraskeletal chondroma; calcification; Magnetic resonance imaging
Introduction
An extraskeletal chondroma (ESC), or a soft tissue chondroma, is a benign, slow-growing cartilaginous tumor arising from tenosynovial sheaths or the soft tissue adjacent to tendons without connection to bone or periosteum [1-8]. The most frequent sites of an ESC are finger (over 80%), hands and feet, though the lesion can be rarely found at other sites such as oral cavity, pharynx, trunk, knee, buttock, fallopian tube, testis, prostate and liver [1,9,10]. Radiological findings are highly suggestive yet the definite diagnosis can only be made histologically. We herein presented an unusual case of ESC of the knee.
Case Report
An otherwise healthy 58 year-old man admitted to our institution with chief complaint of intermittent mild pain in his left knee. He first noticed the pain several years ago without worsening overtime. There was no history of clicking, locking and motion limitation of the left knee. He denied any previous remarkable trauma to the knee. Clinical examination was unremarkable compared to the right side. The local temperature was normal without any sign of a palpable mass, swelling, tenderness, skin color change, joint effusion and instability. The overlying skin was supple, with no dilated veins. The knee reserved full range of motion without distal neurovascular deficit. Laboratory tests were within normal range.
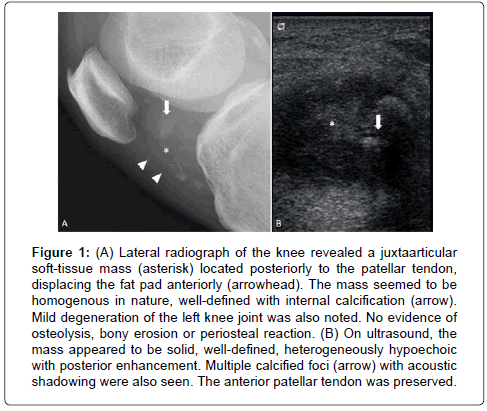
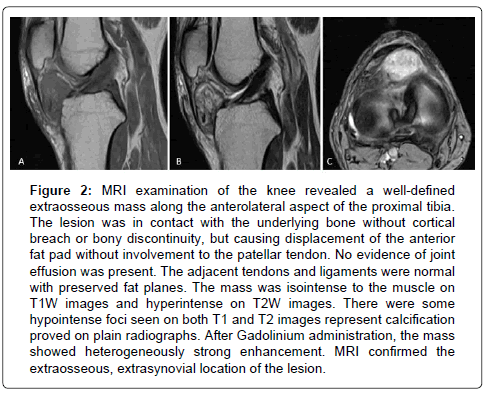
On admission, a knee radiograph (lateral view) demonstrated a suspicious soft tissue mass with various patterns of calcification within the left knee joint (Figure 1). On ultrasound, the mass appeared to be solid, well-defined and heterogeneously hypoechoic with multiple calcified foci distributed centrally. The anterior patellar tendon was preserved. These findings suggested a benign soft tissue tumor of the knee. Magnetic resonance imaging (MRI) was subsequently indicated to define the lesion location and to evaluate for any specific imaging characteristics that might propose a diagnosis. MRI revealed a 3 × 2 × 3 cm well-defined extraosseous mass located along the anterolateral aspect of the proximal tibia (Figure 2). The mass was isointense on T1W (TR/TE 571/16) and hyperintense (TR/TE 3600/79) on T2W images. There was marked diffuse strong homogeneous enhancement throughout the lesion following the administration of intravenous contrast. The remaining subcutaneous fat and adjacent muscle were normal, without surrounding inflammatory changes. Lymphadenopathy was not evident. The imaging characteristics of the mass were considered nonspecific, therefore, various differential diagnosis were accounted and malignancy could not be excluded.
Figure 1: (A) Lateral radiograph of the knee revealed a juxtaarticular soft-tissue mass (asterisk) located posteriorly to the patellar tendon, displacing the fat pad anteriorly (arrowhead). The mass seemed to be homogenous in nature, well-defined with internal calcification (arrow). Mild degeneration of the left knee joint was also noted. No evidence of osteolysis, bony erosion or periosteal reaction. (B) On ultrasound, the mass appeared to be solid, well-defined, heterogeneously hypoechoic with posterior enhancement. Multiple calcified foci (arrow) with acoustic shadowing were also seen. The anterior patellar tendon was preserved.
Figure 2: MRI examination of the knee revealed a well-defined extraosseous mass along the anterolateral aspect of the proximal tibia. The lesion was in contact with the underlying bone without cortical breach or bony discontinuity, but causing displacement of the anterior fat pad without involvement to the patellar tendon. No evidence of joint effusion was present. The adjacent tendons and ligaments were normal with preserved fat planes. The mass was isointense to the muscle on T1W images and hyperintense on T2W images. There were some hypointense foci seen on both T1 and T2 images represent calcification proved on plain radiographs. After Gadolinium administration, the mass showed heterogeneously strong enhancement. MRI confirmed the extraosseous, extrasynovial location of the lesion.
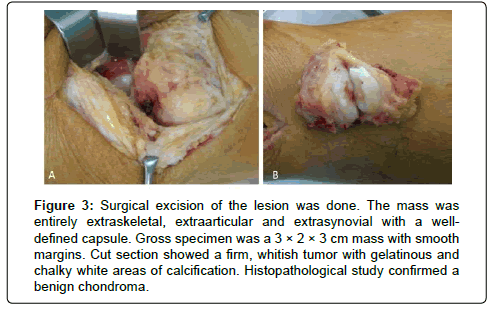
The lesion was fully excised and confirmed entirely extraskeletal, extraarticular and extrasynovial. Macroscopically, the specimen was welldemarcated, measuring 3 × 2 × 3 cm. The cut surface was firm, grayish white, with focal gelatinous areas and calcification (Figure 3). Histological examination confirmed an ESC. The patient had no evidence of local recurrence after 5 years follow-up.
Figure 3: Surgical excision of the lesion was done. The mass was entirely extraskeletal, extraarticular and extrasynovial with a welldefined capsule. Gross specimen was a 3 × 2 × 3 cm mass with smooth margins. Cut section showed a firm, whitish tumor with gelatinous and chalky white areas of calcification. Histopathological study confirmed a benign chondroma.
Discussion
Etiology and demographics
ESC was first described by Baumuller in 1883 and specifically defined later in 1978 by Chung and Enzinger [11]. This slow-growing tumor represents approximately 1.5% of all benign soft tissue tumors [2,9,11,12]. Soft tissue tumors can be categorized as enchondroma, periosteal chondroma and ESC according to their location, in which enchondroma is the most common and the rest are rare [1-4,12,13]. An ESC composes mainly of hyaline cartilage with no connection to bone or periosteum [1-3,7]. There is no gender predilection and the tumor mainly occurs in patients aged 30-60 years [2,5]. The etiology of ESC is uncertain though repeated micro trauma may be an initiating factor [5,11]. It is likely that the tumor cells arise from uncommitted mesenchymal stem cells either by metaplastic or neoplastic processes [9]. Other hypotheses are the migration of cartilaginous cells to the adjacent connective tissues, synovial cell metaplasia or conversion of pre-cartilaginous tissue located at the bone attachment of the ligaments [12].
Clinical and imaging findings
The typical clinical presentation of an ESC is a painless, slowly enlargement nodular soft tissue mass [1]. Grossly, these tumors are usually small, measuring less than 3 cm in diameter, well circumscribed, often encapsulated and have a glassy, myxoid or calcified cut surface [9]. The imaging features of an ESC depend on the amount of calcification and the response of the surrounding tissues [2]. In our case, relatively central calcification was seen with different patterns implying a long-lasting process. In addition, the characteristics of calcification such as ring like, punctate, or granular appearance may suggest the presence of hyaline cartilage [1,2]. Ultrasound can provide additional information of soft tissue nature, contour, infiltration and vascularity. MRI is the method of choice to delineate location and margin of this rare clinical entity, though the appearance is not specific[1,2,4,5,13]. An ESC has been described as low to intermediate signal intensity on T1W images and heterogeneous intermediate to hyperintense signal from the cartilages on T2W images [12]. Signal void can be seen in calcified areas [8]. Contrast enhanced MRI often shows diffuse enhancement within the mass, with normal adjacent soft tissues [1,2].
Treatment and prognosis
ESCs have a 15-25% risk of local recurrence, thus wide surgical excision with preservation of adjacent bone and soft tissue is usually the treatment of choice [3,9,10,12]. However, this tumor rarely evolves into a malignancy and there has been no report of distal or local metastasis [1,2,9].
Differential diagnosis
The differential diagnosis of soft tissue tumors with calcification may include hemangioma, tumoral calcinosis, synovial chondromatosis, myositis ossificans, extraskeletal chondroma/osteochondroma or soft tissue chondrosarcoma, extraskeletal myxoid chondrosarcoma and synovial sarcoma [1,3,6,12]. In tumoral calcinosis, dense calcification and histiocytic response to the calcified material may be present, but cartilage is absent while synovial chondromatosis occurs usually in large joints and consists of numerous cartilaginous nodules [10]. Extraskeletal mesenchymal chondrosarcoma is a malignant cartilaginous tumor occurring most commonly in the head and neck region [10]. Understanding typical chondroid calcification may help confine the differential diagnosis to cartilaginous tumors together with the absence of adjacent bone involvement makes ESC the most likely diagnosis. In addition, negative finding of intraosseous lesions on MRI can eliminate the possibility of chondromyxoid fibroma and chondroblastoma [3]. Synovial sarcoma and soft tissue chondrosarcoma should appear as an ill-defined or infiltrative mass with spotted or dense calcification and heterogeneous on T2W images [3]. The definite diagnosis should be confirmed after correlating clinical, radiological and histopathological examination in order to avoid unnecessary, aggressive management of this rare entity.
Conclusion
In conclusion, ESC is a rare pathologic entity which can be easily overlooked. Awareness of the patterns of internal calcification is essential to narrow the diagnosis to cartilaginous tumor whereas MRI is helpful in determining the location and margin. Definite diagnosis should be made by combining clinical, imaging and histological findings. Radical excision of the tumor is highly recommended.
References
- Adaletli I, Laor T, Yin H, Podberesky DJ (2011) Extraskeletal chondroma: another diagnostic possibility for a soft tissue axillary mass in an adolescent. Case Rep Orthop 2011: 309328.
- Khadija Benhayoune HEF, Hassan ElF, Siham T, Faouzi B, Mohammed ElM, et al. (2014) Soft tissue chondroma: Two cases report and literature review. Case Rep Clin Med 3: 644-649.
- Singh AP, Dhammi IK, Jain AK, Bhatt S (2011) Extraskeletal juxtaarticular chondroma of the knee. Acta orthopaedica et traumatologica turcica 45:130-134.
- Nurten Turhan-Haktanır YD, Alpay H, Fatma A, Nazlı S (2009) Concurrent soft tissue chondroma and periosteal chondroma of thumb. Eur J Gen Med 6: 257-261.
- Bahnassy M, Abdul-Khalik H (2009) Soft tissue chondroma: a case report and literature review. Oman Med J 24: 296-299.
- Rajalakshmi V, Jayaraman, Anand V, Ramprasad N (2014) Extraskeletal chondroma of the foot-a case report. J Clin Diagnostic Res 8: 134-135.
- Saito M, Nishimoto K, Nakayama R, Kikuta K, Nakamura M, et al. (2017) Extraskeletal chondroma of the index finger: A case report. Case Rep Oncol 10: 479-484.
- Kudawara I, Ueda T, Araki N (2001) Extraskeletal chondroma around the knee. Clinical Radiology 56: 779-782.
- Han JY, Han HS, Kim YB, Kim JM, Chu YC (2002) Extraskeletal chondroma of the fallopian tube. J Korean Medl Sci 17: 276-278.
- Parihar A, Khan NP, Agrawal V (2015) Extraskeletal chondroma of the gluteal region along with sporadic Neurofibroma - An unusual presentation. J Clin Diagnostic Res 9: 07-08.
- Schwaiger K, Ensat F, Neureiter D, Wechselberger G, Hladik M (2017) Trigger finger caused by extraskeletal chondroma. J Hand Surg 42: 51-55.
- Alaseirlis D, Tsifountoudis I, Konstantinidis G, Miliaras D, Malliaropoulos N, et al. (2017) Para-articular extraskeletal chondroma mimicking first metatarsophalangeal synovitis. Radiol Case Rep 12: 564-570.
- Miller SF (2014) Imaging features of juxtacortical chondroma in children. Pediatric Radiol 44: 56-63.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi