Case Report, J Neurosci Clin Res Vol: 8 Issue: 3
Neurotoxic Snake Bite: Management
Tarun Kumar Dutta*
Department of Clinical Hematology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
*Corresponding Author: Tarun Kumar Dutta
Department of Clinical Hematology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Tel: 9443602330
E-mail: tkduttajipmer@yahoo.co.uk
Received date: 19 May, 2023, Manuscript No. JNSCR-23-99314;
Editor assigned date: 22 May, 2023, PreQC No. JNSCR-23-99314 (PQ);
Reviewed date: 05 June, 2023, QC No. JNSCR-23-99314;
Revised date: 19 July, 2023, Manuscript No. JNSCR-23-99314 (R);
Published date: 26 July, 2023, DOI: 10.4172/JNSCR.1000161
Citation: Dutta TK (2023) Neurotoxic Snake Bite: Management. J Neurosci Clin Res 8:3.
Abstract
Principally there are two types of neurotoxic snakes seen in Indian subcontinent, namely Indian cobra and common krait. Venom acts at myoneural junction and paralyses muscle. Cobra bite has reversible action on muscle and patient responds to ASV and anti-cholinesterase; however common krait has irreversible action and patient may die due to bulbar and respiratory paralysis, thus may need to be kept on ventilatory support for longer time.
Case report: A 30 years old housewife got up in the morning and discovered, she was not able to open her eyes fully; she also noticed occasionally double vision.
Patient had slept last night on the floor on a mat. On closer observation, a painless bite mark was seen on the right arm. With passage of time patient complained of swallowing difficulty and nasal regurgitation of food. The treating doctor from his professional experience suspected a neurotoxic snake bite, and possibly a krait bite. Patient subsequently developed swallowing difficulty, muscular weakness and respiratory distress. Patient was immediately transferred to a hospital and connected to a ventilator. Patient was administered polyvalent Anti-Snake Venom (ASV) and injection neostigmine.
Over few hours, patient improved and herptosis and diplopia disappeared. Subsequently she was weaned off ventilator and within next two days patient was discharged.
Keywords: Cobra; Neostigmine; Neurotoxic snake; Anticholinesterase; Venom
Introduction
Among two major types of snake bites, one is vasculotoxic caused by Vipiridae group of snakes, and other one is neurotoxic caused by Elapidae group of snakes. Two important snakes in this Elapidae group are Indian cobra (Naja naja) and common krait (Bungarus caeruleus) [1]. They usually leave two or single fang mark at site of bite following bite.
Mechanism of action
Krait venom contains B-bungarotoxin which is presynaptic Acetyl choline (Ach) Ach receptor blocker with phospholipase A2 activity. Action is irreversible even with administration of Anti-Snake Venom (ASV). Action is much stronger compared to that due to cobra. Usually there is no local swelling unlike as in cobra bite case.
Cobra has a post-synaptic neurotoxin which is present in alpha neurotoxin of its venom. It inhibits nicotinic Ach receptor [2].
Clinical features
Cobra bite: Apart from severe pain, local swelling at site of bite and blisters, patients develop neuromuscular paralysis (at myoneural junction), which presents as ptosis, diplopia may follow. Paralysis then descends to bulbar muscles. Patient may have swallowing difficulty and develops respiratory paralysis and may succumb to this unless intervened with mechanical ventilator. Recovery occurs in the reverse order and ptosis and ophthalmoplegia recover the last.
Krait bite: Even though presentation is similar to as in cobra bite, there is no local swelling at site of bite and injury may go unnoticed.
Management
Snakes cause acute reversible muscle paralysis by inhibiting neuromuscular transmission. Naja naja neurotoxins (alfa-bungaro toxins have post-synaptic in action and their binding is reversible. Improvement occurs within 30-60 minutes of initial dose of Anti-Snake Venom (ASV). Anticholinesterase drugs like neostigmine sometimes are even more effective. Krait venoms have pre-synaptic action and bind irreversibly. Anticholinesterases are usually not effective to neutralize B-bungarotoxins.
Mechanical ventilation: In view of irreversible blockade, mechanical ventilation may be required for weeks till natural waning of venom occur in body.
Anti-Snake Venom (ASV): One available in India is polyvalent anti-snake venom which works against venoms all the four common species of snake russell’s viper (Daboia russelii), common cobra (Naja naja), common krait (Bungarus caeruleus) and saw scaled viper (Echis carinatus) [3].
National protocol of India recommends as follows
• 1st dose: 100 ml of ASV+2nd dose of ASV of 100 ml after two hours (maximum total 200 ml), if no subsidence of symptoms, and none thereafter.
It is believed administering further dose of ASV will be wastage, since 200 ml of ASV is likely to neutralize total dose of venom injected after a single bite [4].
• Neostigmine: Elapidae venom blocks Ach receptors. Neostigmine
can reverse it especially in cobra bite cases. Dose: 25 ug/kg/hr
proceeded by atropine.
• Mechanical ventilation: Indicated when tidal volume <200 ml. In
absence of ASV, long term use of artificial ventilation alone may
suffice in an emergency [5].
Case Presentation
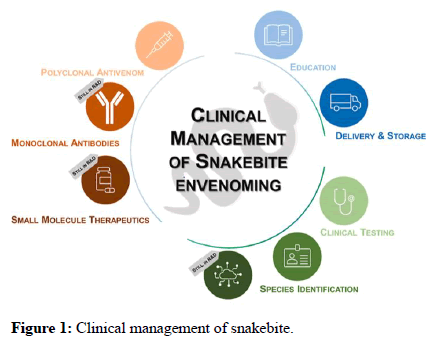
In this study, clinical profile of 51 patients of neurotoxic snake bites was studied. 28 patients were females and 23 males. Patients were bitten usually early morning. Patients had been randomized to conventional high dose regime group (25 patients) and national protocol low dose group (26 patients). Conventional regime group received 100 ml ASV every 6 hours till full recovery [6]. National protocol group received initial 100 ml and another dose of 100 ml ASV if symptoms persist, tell maximum of 200 ml ASV. The logic behind maximum 200 ml ASV is any snakebite can maximum inject venom which is neutralized by 200 ml of ASV thus administration beyond 200 ml is likely to be wastage. 39 patients required mechanical ventilation (Figure 1).
The aim of this study was to test the efficacy of low dose ASV regimen (national protocol) against the conventional high dose regime.
Results and Discussion
In terms of progression of neuroparalysis, time to complete resolution of ptosis and occurrence of VAP and ASV reactions, there was no difference between two groups. Duration of mechanical ventilation was less with the national protocol (24 h vs. 43.5 h). Significantly less amount of ASV was used with the national protocol (224 ml vs. 982 ml) per patient [7]. There were no mortality or permanent neurological sequelae with either regimen.
Interpretation
In this preliminary study, it was found that the national (low dose) ASV protocol was as effective as the conventional (high dose) regimen for neurotoxic snake bites.
Snake envenomation is a major health problem, particularly in rural India. Approximately 35,000-50,000 people die of snakebite every year in India. Snakes of family Elapidae are predominantly venomous causing neurotoxic features. This family includes cobra and krait, the most common neurotoxic envenomations encountered in clinical practice [8].
The dosage of Anti-Snake Venom (ASV) required to treat neurotoxic envenomation has been a subject of debate for many years. The conventional regimen for neurotoxic snake bite is to administer ASV at a dose of 100 ml every six hours till all features of envenomation resolve. The national snake bite protocol has set 200 ml ASV as the maximum dose needed to treat neurotoxic snake bite. This dose was arrived at on the basis of the average amount of venom injected per bite and the amount of antivenom needed to neutralize that amount.
ASV is a scarce, expensive drug and should be administered only when there are definite signs of envenomation. Unbound venom can be neutralized with ASV, but once bound, the reversibility is questionable. Adoption of the proposed national protocol will lead to significant reduction in the total dose of ASV used.
Inference: It appears that the national ASV protocol (low dose) may be as effective as the conventional regimen (high dose protocol) in treating neurotoxic snake bites. However, this being a preliminary study with a comparatively small sample size, this needs to be tested in a larger trial before definitive recommendations can be made. The result of this study discourages use of massive doses of ASV in neurotoxic snake bite.
Conclusion
Principally there are two types of neurotoxic snakes seen in Indian subcontinent, namely Indian cobra and common krait. Venom acts at myoneural junction and paralyses muscle. Cobra bite has reversible action on muscle and patient responds to ASV and anti-cholinesterase however common krait has irreversible action and patient may die due to bulbar and respiratory paralysis. Interestingly it is observed that maximum dose of ASV required may be 200 ml (100 ml initially and then 100 ml if inadequate response to initial dose).
References
- Monzavi SM, Dadpour B, Afshari R (2014) Snakebite management in Iran: Devising a protocol. J Res Med Sci 19:153.
[Crossref] [Google Scholar] [PubMed]
- Mehta SR, Sashindran VK (2002) Clinical features and management of snake bite. Med J Armed Forces India 58:247.
[Crossref] [Google Scholar] [PubMed]
- Alirol E, Sharma SK, Bawaskar HS, Kuch U, Chappuis F (2010) Snake bite in South Asia: A review. PLoS Negl Trop Dis 4:e603.
[Crossref] [Google Scholar] [PubMed]
- Boyd JJ, Agazzi G, Svajda D, Morgan AJ, Ferrandis S, et al. (2007) Venomous snakebite in mountainous terrain: Prevention and management. Wilderness Environ Med 18:190-202.
[Crossref] [Google Scholar] [PubMed]
- Chauhan V, Thakur S (2016) The North-South divide in snake bite envenomation in India. J Emerg Trauma Shock 9:151.
[Crossref] [Google Scholar] [PubMed]
- Sutherland SK, Leonard RL (1995) Snakebite deaths in Australia 1992-1994 and a management update. Med J Aust 163:616-618.
[Crossref] [Google Scholar] [PubMed]
- Ahmed SM, Ahmed M, Nadeem A, Mahajan J, Choudhary A, et al. (2008) Emergency treatment of a snake bite: Pearls from literature. J Emerg Trauma Shock 1:97-105.
[Crossref] [Google Scholar] [PubMed]
- Sharma SK, Khanal B, Pokhrel P, Khan A, Koirala S (2003) Snakebite reappraisal of the situation in Eastern Nepal. Toxicon 41:285-289.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi