Research Article, J Sleep Disor Vol: 8 Issue: 1
Predicting Technical Success in Home Sleep Apnea Test
Anniina Alakuijala1,2*, Julia Tervamäki1, Paula Maasilta3 and Adel Bachour3
Department of Forestry and Biodiversity, Tripura University, Suryamaninagar, Agartala, India
*Corresponding Author: Selvan T
Tripura University, Department of Forestry and Biodiversity, Suryamaninagar, Agartala- 799 022, India
Tel: +91- 8974236218
E-mail: tselvan@tripurauniv.in
Received: December 29, 2016 Accepted: March 09, 2017 Published: March 13, 2017
Citation: MeCarty SC, Chauhan DS, MeCarty AD, Tripathi KM, Selvan T (2017) Effect of Azotobacter and Phosphobacteria on Yield of Wheat (Triticum aestivum). Vegetos 30:2. doi: 10.4172/2229-4473.1000225
Abstract
Background: Home sleep apnea tests are economical but their technical failure rate is higher than with in-lab studies. We aimed to predict factors related to failures. Methods: Altogether, 1,055 consecutive respiratory polygraphy recordings for subjects aged 16-90 years (38% female) were included. The sleep nurses were asked to predict the success of the upcoming recording according to their experienced perception. The recording was considered successful if the main recorded parameters (nasal flow, thoracic and abdominal movements, blood oxygen saturation, snoring, and posture) were intelligible during ≥80% of the night. Results: Defects due to a recording device caused a failure rate of 4.4%, and those recordings were excluded from further analyses. Subject-related reasons caused a failure rate of 10.4% (i.e. 70% of all failures). There were no statistically significant differences in the failure rate regarding gender, age, education level, ESS, smoking habits, BMI, comorbidities, sharing a bed with someone, having small children or pets, being outside of working life, or working irregular hours. Nurse’s prediction of reliability sorted out successful and unsuccessful recordings statistically significantly (P=0.035). The technical success was not statistically significantly different between first-time and repeated recordings. Conclusions: Background characteristics of the subject or conditions during the recording did not predict the failure of home sleep apnea test. An experienced nurse could still predict the technical success of the recording based on her perception. Even if the first test failed, it is still worthwhile to retest at home, as the failure rate in repeated recordings stayed low.
Keywords: Obstructive sleep apnea; Home sleep apnea test; Reliability; Failure; Recording; Retest
Abbreviations
AASM: American Academy of Sleep Medicine; AHI: Apnea-hypopnea Index; BMI: Body Mass Index; CCI: Charlson Comorbidity Index; CPAP: Continuous Positive Airway Pressure; ESS: Epworth Sleepiness Scale; HSAT: Home Sleep Apnea Test; ODI3: Oxygen Desaturation Index Of Three Percentage Units; OSA: Obstructive Sleep Apnea; PSG: Polysomnography; REI: Respiratory Event Index (corresponding to AHI in PSG)
Introduction
Obstructive sleep apnea (OSA) is characterized by recurrent upper airway collapse during sleep associated with frequent oxygen desaturations and arousals. OSA is the most common sleep disorder leading to an increased risk of cardiovascular and neurologic comorbidities. The reference standard for diagnosing OSA is an attended overnight polysomnography (PSG) [1]. However, this Level 1 sleep testing is expensive and laborious both for patients and staff. Level 3 testing uses portable monitors which record at least three channels of data (e.g., oximetry, airflow, respiratory effort). This home sleep apnea testing (HSAT) allows diagnostic sleep studies to be done at the patient’s home or elsewhere outside a sleep laboratory, like in a hospital ward. For subjects without suspicion of other sleep disorders than OSA, a multi-channel HSAT, respiratory polygraphy, is equally reliable compared to PSG [2,3]. As for the results of HSAT, American Academy of Sleep Medicine (AASM) recommends the use of respiratory event index (REI) instead of apnea-hypopnea index (AHI) because the actual sleep time cannot be determined [1].
Unattended sleep studies have inevitably higher risk of technical failures than attended ones. Previously, the proportion of technically unsuccessful recordings with Level 3 portable monitors has ranged from 3 to 27% [4-11]. Subject-related factors associated with failure rate have not often been addressed. Domingo and Vigil reported that correct performance of HSAT was not affected by gender, smoking habits, education, or type of health insurance [7]. In another study among patients with chronic kidney disease, HSAT was more often failed, if the patient also had comorbid diabetes [10].
Most subjects sleep better at home than in the sleep laboratory [12]. Sometimes children creeping to the same bed during the night, snoring sounds of a bed partner, noise from restless pets or other environmental sources may disturb sleep during the test night, however. Both sleep laboratory personnel and subjects themselves may have doubts about whether a non-professional can manage to hook up the necessary sensors at home before going to bed.
We aimed to look more closely at factors eventually leading to unreliable HSAT, including background characteristics of the subjects but also conditions during the preparations and the actual process of overnight recording in the home environment. Our hypotheses were that subjects with old age, low education level, high body mass index (BMI), or who smoke, have small children or pets at home, suffer from comorbidities in addition to OSA, work irregular hours or are outside of working life, sleep poorly, share a bed with someone, or have findings of a severe OSA in the recording, have higher failure rate in HSAT than subjects without these attributes.
Methods
The Helsinki and Uusimaa Ethics Committee approved the study (38/2013), and because the study is based only on documents completed during normally scheduled outpatient visits and diagnostic procedures, no written informed consent was required.
All consecutive home sleep apnea tests made during the year 2014, altogether 1,055 recordings, were included in this retrospective study. Subjects were referred to our laboratories for suspicion of OSA. A referral was accepted if the subject had two or more of the following symptoms: excessive daytime sleepiness, loud snoring, pauses in breathing during sleep observed by someone else, headache in the morning, shortness of breath during sleep, cognitive impairment, or depression with a suspicion of association with sleep apnea. Most of the subjects were snorers and suffered from a variable degree of daytime somnolence.
This study was conducted in two separate laboratories: Center A: Department of Clinical Neurophysiology and Center B: Sleep Unit at the Heart and Lung center.
Center A
Subjects were referred by general practitioners (65%) and specialists (35%, mostly otorhinolaryngologists and neurologists), and 947 HSATs were conducted during the single year. Nineteen qualified female nurses with a mean age of 43 years and with an experience of eight years on average, and two female nursing students participated. Of note, there are very few sleep technicians in our country, and therefore qualified nurses prepare the recordings and instruct the subjects.
Center B
Subjects were referred mainly from pulmonary or other departments in the university hospital. Sleep Unit is focused on performing in-lab PSG and starting continuous positive airway pressure (CPAP) treatment. During the single year, 108 HSATs were conducted by eight qualified female nurses with a mean age of 35 years and with an experience of four years on average.
On both locations, qualified nurses instructed the subjects in the preceding afternoon before HSAT. The guiding session usually lasted about 30 minutes. Afterwards, the nurse predicted the technical success of the upcoming recording by marking a vertical line on a 10 cm long line segment, the ends being total success (100%) and total failure (0%). She was asked to explain which factors she based her prediction on, the options being the subject’s fine motor, memory, or language skills, other diseases, aberrations in sleep cycle, motivation, being in a hurry, and understanding the instructions. It was possible to pick more than one predictive factor.
In addition, between the guiding session in the afternoon and going to bed in the evening, the subject was asked to predict the technical success of the upcoming recording, similarly to a nurse. The subject was also asked to estimate his or her motivation to the study and whether he or she felt that the amount of information about how to proceed at home in the evening, during the night, and in the morning was sufficient. These two estimates were asked with the help of the 10-cm long line segment, as well. The subjects also filled in a questionnaire based on Basic Nordic Sleep Questionnaire [13] with some new questions about the household arrangements, e.g., ages of children living with the subject. Age-adjusted Charlson comorbidity index (CCI) was measured, as well [14,15].
All cardiorespiratory polygraphs included in this study were performed at home. Subjects used either a NOX T3 Sleep Monitor (Nox Medical, Reykjavik, Iceland) or an Embletta Gold device (Embla, Denver, CO, USA) to perform HSAT. Respiratory parameters were scored manually according to AASM criteria [16].
Every morning, when an HSAT device was returned to the center, the recording was downloaded to a computer and all the signals were inspected. Had there been faults lasting for more than a couple of minutes, the function of the particular sensor was checked thoroughly, usually so that the nurse wore the sensor herself for a while. Thus, defective sensors and devices were detected before they were given to the next subject. This procedure allowed us to classify failures to device-related and subject-related, as well. If no defect was found during the check, we assumed that the failure in the recorded signal was caused by the subject, who perhaps totally forgot to put on an oximeter or did not fasten it tightly to a finger etc.
Two authors (AA, AB) went through all the signals in all the recordings and assessed if they were good enough to be interpreted. First, a proportion of recording time with a technically reliable signal was assessed for each signal. Then, the recording was considered technically successful, if the recording time was ≥ 4 hours and all the important recorded signals (nasal cannula or thermistor, either thoracic or abdominal respiratory belt, pulse oximetry, snoring sensor, and position sensor) were intelligible during at least 80% of the night [7].
However, not all those recordings which failed to fulfill the criteria presented in the literature were actually repeated. If the initial results showed a diagnosis of severe OSA (i.e., REI was>30/h), a retest was not carried out despite moderate technical problems in order to avoid further delays in starting the treatment. A total failure in the oximeter signal was always an indication for retest, however. In addition, it was considered possible to give a reasonably reliable answer from the recording in a case when a subject slept only 3 h 50 min or there were problems with snoring sensor or respiratory belts, but the remaining available data showed a moderate or severe OSA. These recordings were considered clinically reliable and this assessment was agreed by all the authors. In other words, clinically reliable recording refers to the processes in everyday clinical practice.
Statistics
Results were generated with a computerized statistical package (IBM SPSS® Statistics 22.0, Armonk, NY, USA). We used the Student’s t test for continuous variables and Chi Square test for categorical variables. Some of the measured parameters had slight abnormalities with their distributions, but our material is so large that parametric tests can be used in any case. All P values are two-sided, and the significance level is set at 0.05 throughout. For descriptive purposes, we report values as means and standard deviation.
Results
Altogether, 1,055 successive HSATs were included in this material. They were done to 997 different subjects, aged 16-90 years. Additionally, 58 recordings were repetitions. Sixty-two percent of tests were performed to male subjects, who were, on average, younger than female subjects (Table 1).
| All | Female | Male | P | |
|---|---|---|---|---|
| n | 1055 | 402 | 653 | |
| Age (y) | 53.8 (15.0) | 56.2 (15.0) | 52.4 (14.8) | <0.001 |
| Quality of air flow, nasal cannula | 95.2 (16.5) | 97.4 (11.2) | 93.9 (19.0) | <0.001 |
| Quality of air flow, thermistor (n=111) | 87.2 (29.9) | 91.7 (25.1) | 84.7 (32.1) | 0.205 |
| Quality of oximeter | 94.2 (20.2) | 95.7 (16.8) | 93.3 (21.9) | 0.045 |
| Quality of respiratory movements, thorax | 95.5 (19.1) | 96.0 (17.4) | 95.2 (20.1) | 0.466 |
| Quality of respiratory movements, abdomen | 95.6 (18.8) | 97.1 (15.0) | 94.8 (20.8) | 0.038 |
| Quality of snoring with microphone (n=629) | 95.4 (13.1) | 96.1 (9.4) | 95.0 (14.9) | 0.222 |
| Quality of position data | 97.8 (12.7) | 98.9 (6.4) | 97.2 (15.2) | 0.014 |
| Technically successful (%) | 85.2 | 87.6 | 83.8 | 0.092† |
| Technically unsuccessful (%) | 14.8 | 12.4 | 16.2 | 0.092† |
| Failure due to device (%) | 4.4 | 3 | 5.2 | 0.086† |
| Failure due to subject (%) | 10.4 | 9.4 | 11 | 0.086† |
| Clinically unreliable (%) | 7.6 | 6.5 | 8.3 | 0.283† |
Table 1: All home sleep apnea tests.
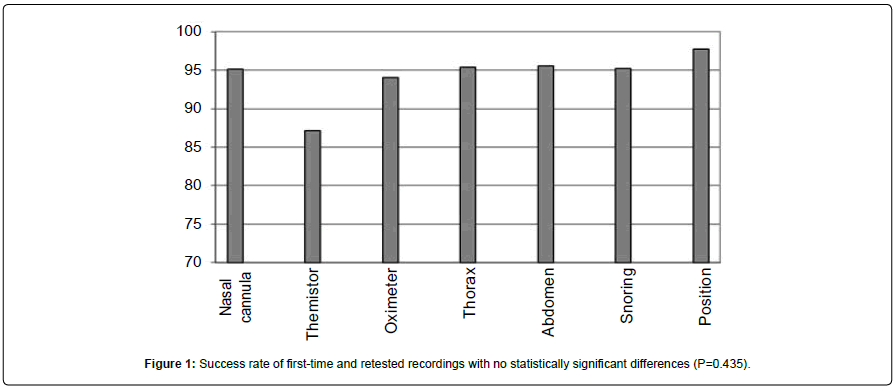
Of these 1,055 recordings, 900 were technically successful (see methods for the definition). That is to say, technical success rate in the whole material was 85.2%. When separate signals are considered, thermistor was by far the most vulnerable signal, while the position detector had the highest quality (Figure 1). Recording time was less than four hours in only four recordings, if they were otherwise technically successful. Female subjects’ recordings had better quality in all different signals, particularly the air flow measured by nasal cannula (Table 1).
Failure of the recording was due to a technical defect in the function of a measuring device in 30% of the technically unsuccessful cases. In other words, defects due to a recording device caused a failure rate of 4.4%, and those recordings were excluded from further analyses. The most common reasons comprised defects in an oximeter contact or a missing data from the whole night. There were differences between the separate laboratories. The smaller Sleep Unit conducted 8.3% of all recordings but 21.2% of technically unsuccessful recordings.
Of all recordings, 10.4% were technically unsuccessful due to the subject and not device. Subject-related reasons caused 70% of all failures. The classification to device-related and subject-related failures was made after the check in the following morning by the sleep nurse (see methods for further details). In order to find out what kind of subjects are more prone to failures, we analyzed further only those 1,009 recordings, where the device itself had functioned properly. The technical success rate without device-related failures was 89.1%.
All the background characteristics of the subjects with technically successful and unsuccessful recordings without device-related failures are compared in Table 2. Surprisingly, there were no statistically significant differences in regard to gender, age, education level, Epworth sleepiness scale (ESS), smoking habits, BMI, having comorbidities, sharing a bed with someone, having small children or pets at home, being outside of working life, or working irregular hours. REI, oxygen desaturation index of three percentage units (ODI3), recording time, and subjective sleep quality during the recording were also similar. The used device or the laboratory did not make a difference here.
| Technically successful | Technically unsuccessful | P | |
|---|---|---|---|
| n | 899 | 110 | |
| Females (%) | 39.2 | 34.5 | 0.349† |
| Age (y) | 53.8 (14.7) | 54.3 (17.2) | 0.768 |
| BMI | 29.5 (6.4) | 29.4 (7.0) | 0.926 |
| ESS | 8.2 (4.4) | 8.4 (4.6) | 0.751 |
| Age-adjusted CCI | 0.61 (1.3) | 0.76 (1.5) | 0.298 |
| Smoker (%) | 19.5 | 20.2 | 0.860† |
| Ex-smoker (%) | 35.2 | 40.4 | 0.297† |
| Sleeps usually alone (%) | 51.9 | 44.3 | 0.142† |
| Underage children (%) | 22.4 | 21.9 | 0.918† |
| Pets (%) | 25.2 | 19.6 | 0.213† |
| Working (not unemployed, sick, or retired) (%) | 49.8 | 41.2 | 0.102† |
| Shift work (%) | 7.3 | 8.8 | 0.589† |
| High education level (%) | 33 | 29.1 | 0.429† |
| Nurse's prediction of success (0-100%) | 86.9 (15.0) | 83.2 (17.1) | 0.035 |
| Subject's prediction of success (0-100%) | 81.5 (17.6) | 78.6 (18.5) | 0.141 |
| Subject's motivation (0-100%) | 93.3 (10.6) | 93.5 (7.8) | 0.8 |
| Subject's view of adequate information (0-100%) | 94.3 (9.4) | 94.0 (8.8) | 0.761 |
| Embletta Gold device (vs. NOX T3) (%) | 39.5 | 39.8 | 0.948† |
| Sleep Unit (vs. Dep. of Clin. Neurophysiol.) (%) | 8.3 | 12.7 | 0.126† |
| REI (/h) | 20.7 (21.5) | 17.7 (18.5) | 0.151 |
| ODI3 (/h) | 21.2 (21.4) | 19.7 (21.3) | 0.533 |
| Recording time (min) | 435 (71) | 419 (99) | 0.128 |
| Subjective sleep quality (0-100%) | 44.3 (25.1) | 44.5 (28.0) | 0.929 |
Table 2: HSAT without device-related failures.
Nevertheless, the nurse could still predict the technical success of the upcoming recording statistically significantly, as the prediction for success in recordings that turned out to be technically successful was 86.9%, while the prediction was 83.2% in recordings that failed in the following night (Table 2). Furthermore, in a gender-specific analysis, it was noticed that the nurse could very well predict the technical success of the recordings of male subjects: the nurse’s prediction for success was 88.0% (SD 14.3%) in technically successful recordings vs 82.0% (SD 18.9%), P = 0.014, in technically unsuccessful recordings. On the contrary, the nurse could not at all predict the technical success of the upcoming recording of female subjects: the nurse’s prediction for success was 85.1% (SD 16.0%) in technically successful recordings vs 85.3% (SD 12.9%), P = 0.943, in technically unsuccessful recordings.
Understanding the instructions during the guiding session was the most significant predictive factor (P = 0.047). By contrast, the subject himself/herself was not able to predict the technical success of the upcoming recording. His or her motivation or the impression of having adequate amount of information about the recording did not differ at all between technically successful and unsuccessful recordings (Table 2).
However, not all those recordings which failed to fulfill the criteria for technically successful recording presented in the literature were repeated. Of the total amount of 1,055 home sleep apnea studies, 80 (7.6%) recordings were clinically unreliable (see methods for the definition), i.e. it was necessary to repeat them. In Table 3, background characteristics of the subjects are compared between those clinically reliable and unreliable HSAT where the device had functioned properly. If the subject usually sleeps alone, the recording was more prone to be clinically reliable. Other background characteristics of the subjects were similar in clinically reliable and unreliable recordings. REI was statistically significantly higher in clinically reliable recordings.
| Clinically reliable | Clinically unreliable | P | |
|---|---|---|---|
| n | 959 | 50 | |
| Females (%) | 38.7 | 38 | 0.923† |
| Age (y) | 53.9 (14.9) | 53.4 (17.3) | 0.84 |
| BMI | 29.5 (6.4) | 29.7 (7.2) | 0.792 |
| ESS | 8.2 (4.4) | 8.6 (4.3) | 0.579 |
| Age-adjusted CCI | 0.61 (1.3) | 0.90 (1.6) | 0.218 |
| Smoker (%) | 19.7 | 15.6 | 0.490† |
| Ex-smoker (%) | 35.3 | 44.4 | 0.213† |
| Sleeps usually alone (%) | 51.9 | 35.4 | 0.026† |
| Underage children (%) | 22.3 | 21.7 | 0.925† |
| Pets (%) | 24.9 | 20 | 0.460† |
| Working (not unemployed, sick, or retired) (%) | 49.2 | 40.9 | 0.282† |
| Shift work (%) | 7.5 | 6.8 | 0.861† |
| High education level (%) | 32.7 | 31.1 | 0.830† |
| Nurse's prediction of success (0-100%) | 86.8 (15.0) | 79.5 (19.3) | 0.018 |
| Subject's prediction of success (0-100%) | 81.3 (17.7) | 80.6 (16.8) | 0.81 |
| Subject's motivation (0-100%) | 93.3 (10.5) | 93.2 (8.2) | 0.907 |
| Subject's view of adequate information (0-100%) | 94.2 (9.4) | 94.6 (6.6) | 0.692 |
| Embletta Gold device (vs. NOX T3) (%) | 39.2 | 45.8 | 0.360† |
| Sleep Unit (vs. Dep. of Clin. Neurophysiol.) (%) | 8.9 | 8 | 0.834† |
| REI (/h) | 20.6 (21.3) | 12.9 (17.8) | 0.029 |
| ODI3 (/h) | 21.2 (21.2) | 17.6 (27.8) | 0.532 |
| Recording time (min) | 435 (72) | 402 (115) | 0.096 |
| Subjective sleep quality (0-100%) | 44.5 (25.2) | 40.7 (28.4) | 0.339 |
Table 3: HSAT without device-related failures.
The nurse could predict the clinical reliability of the upcoming recording even better than the technical success described above, particularly of male subjects: the nurse’s prediction for success was 87.9% (SD 14.4%) in clinically reliable recordings vs 76.9% (SD 21.1%), P<0.001, in clinically unreliable recordings, but not of female subjects. Understanding the instructions during the guiding session was statistically very significant predictive factor (P = 0.001). In addition, a memory deficit was a significant predictive factor for a clinically unreliable recording, although it appeared quite rarely.
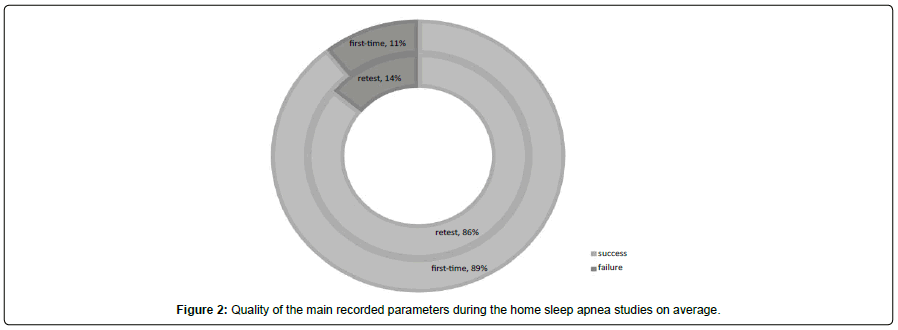
In repeated HSAT, the technical success rate without device-related failures was 86.0% (Figure 2). It was not statistically significantly different from first-time recordings (P = 0.435). Repeated recordings did not differ from the first-time recordings in any of background characteristics or recording details, either (not shown).
Discussion
To the best of our knowledge, this is the largest study aiming to predict factors causing technically unsuccessful HSAT. We studied all recordings during one year conducted to subjects with moderate or high susceptibility for obstructive sleep apnea. We found that age, education level, ESS, smoking habits, BMI, comorbidities, sharing a bed with someone, having small children or pets at home, being outside of working life, or working irregular hours did not predict the failure. Had there been significant predictive factors for technically unsuccessful recordings, they would certainly have emerged in this very large material.
Many colleagues working in the sleep medicine field presume that elderly subjects or subjects with numerous pets or many small children cannot be reliably studied in the home environment. Our present data did not support this presumption. There were no statistically significant differences in the technical success rate with respect to age or any other background characteristics or conditions during the recording. Surprisingly, if a subject had a teenager or a dog at home, a recording was actually slightly more prone to be technically successful in our study. Probably these factors are not protective as such but they associate with a subject having “a life in order” with an interest in health.
Even if strong predictive factors could not be detected, experienced nurses could still predict technical success rate and clinical reliability very well in this large material. Our nurses managed to predict the failure of the recording remarkably well in men, but not in women. One reason behind this gender difference might be women’s older age which, in the conditions of using technical equipment, sometimes rises concerns among younger personnel. Another explanation could be that, during the guiding session, women expressed their worries about the recording while men often hid their expressions.
The fact that home sleep apnea tests collected in this study were conducted in two separate sleep laboratories revealed some differences between centers. Center A, Department of Clinical Neurophysiology, was larger than Center B, Sleep Unit. It is specialized in various recordings and tests, also outside the sleep medicine field. Center A performed eight times more HSAT than center B, yielding in better team and personal experience. Center A had a detailed and systematic check of the recorded signals which probably prevented some device-related technical failures that emerged in Center B where a shorter device check was done. As a consequence, the device-related technical success rate was slightly lower in center B. The practice of routinely testing the quality of the main recorded signals can be warmly recommended to every sleep laboratory conducting HSAT. The number of the recording devices should be large enough in order to enable a proper check and also maintenance, if needed, between the recordings. When only subject-related technical success rate is considered, there was no statistically significant difference between the centers. This leads to a conclusion that both centers had sufficiently qualified nurses. The nurses evaluated the ability of the subject in assimilating instructions and adjusted their instructions to obtain the best results. Sometimes a 30-minute instruction time proved insufficient but the nurses had to cope with their daily schedule.
The overall proportion of technically unsuccessful and clinically unreliable recordings was comparable to earlier research. Previously, results have ranged from 3 to 27%, depending on the definition of failure and on the characteristics of the patient group, like devastating comorbidities [4-11]. Our failure rate was relatively low, as only 7.6% needed another test. What is more, repeated HSAT also had an equally low failure rate. Hence, there is no need to send the subject to much more expensive in-lab sleep study.
Limitations
Our study has certain limitations to address. All subjects in the study had the same national insurance system covering about 90% of the total HSAT costs; therefore, we cannot generalize our conclusions to other health insurance systems. Moreover, 99% of subjects were of Caucasian origin, and the failure rate may be different in other groups. Both participating centers were part of the university hospital, and results cannot be generalized to other types of sleep centers. We cannot draw conclusions about other types of HSAT devices than the two used in this study. The precise time spent in the individual guiding session prior to the recording and its correlation to the success rate is unknown.
Conclusions
Gender, age, education, comorbidities, or other background characteristics did not predict the failure of HSAT. Even if there was a failure, it is cost-effective to retest at home, as the failure rate in repeated recordings stayed low.
Acknowledgements
We thank all the personnel in the participating sleep centers for their valuable help in collecting data. The Helsinki University Special Fund is acknowledged for providing financial support in the form of research grant funding (grant number Y2017SK002 to Adel Bachour).
References
- Kapur VK, Auckley DH, Chowduri S, Kuhlmann DC, Mehra R, et al. (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 13:479-504.
- Atwood CW (2012) The times they are a changin: Home diagnosis of sleep apnea has arrived. Sleep 35: 735-736.
- El Shayeb M, Topfer LA, Stafinski T, Pawluk L, Menon D (2014) Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. CMAJ 186:E25-51.
- Dingli K, Coleman EL, Vennelle M (2003) Evaluation of a portable device for diagnosing the sleep apnoea/hypopnoea syndrome. Eur Respir J 21:253-259.
- Yin M, Miyazaki S, Ishikawa K (2006) Evaluation of type 3 portable monitoring in unattended home setting for suspected sleep apnea: factors that may affect its accuracy. Otolaryngol Head Neck Surg 134:204-209.
- Santos-Silva R, Sartori DE, Truksinas V (2009) Validation of a portable monitoring system for the diagnosis of obstructive sleep apnea syndrome. Sleep 32: 629-636.
- Domingo C, Vigil L (2011) Effectiveness of unattended ambulatory sleep studies for the diagnosis and treatment of OSAS. J Eval Clin Pract 17: 26-31.
- Polese JF, Santos-Silva R, de Oliveira, Ferrari PM, Sartori DE, et al. (2013) Is portable monitoring for diagnosing obstructive sleep apnea syndrome suitable in elderly population? Sleep Breath 17: 679-686.
- Tedeschi E, Carratù P, Damiani MF, Ventura VA, Drigo R, et al. (2013) Home unattended portable monitoring and automatic CPAP titration in patients with high risk for moderate to severe obstructive sleep apnea. Respir Care 58: 1178-1183.
- Lee J, Turin TC, Nicholl DD, Ahmed SB, Loewen AH, et al. (2015) Predictors of successful completion of diagnostic home sleep testing in patients with chronic kidney disease. Sleep Breath 19: 669-675.
- Bachour A, Aalto T, Maasilta P (2016) Home sleep apnea study of patients with limited to no mobility. J Sleep Disor Treat Care S1.
- Masa JF, Corral J, Pereira R, Duran-Cantolla J, Cabello M, et al. (2011) Effectiveness of home respiratory polygraphy for the diagnosis of sleep apnoea and hypopnoea syndrome. Thorax 66: 567-573.
- Partinen M, Gislason T (1995) Basic Nordic Sleep Questionnaire (BNSQ): a quantitated measure of subjective sleep complaints. J Sleep Res 4: 150-155.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373-383.
- Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47: 1245-1251.
- Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, et al. (2012) Rules for scoring respiratory events in sleep: Update of the 2007 AASM manual for the scoring of sleep and associated events. J Clin Sleep Med 8: 597-619.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi