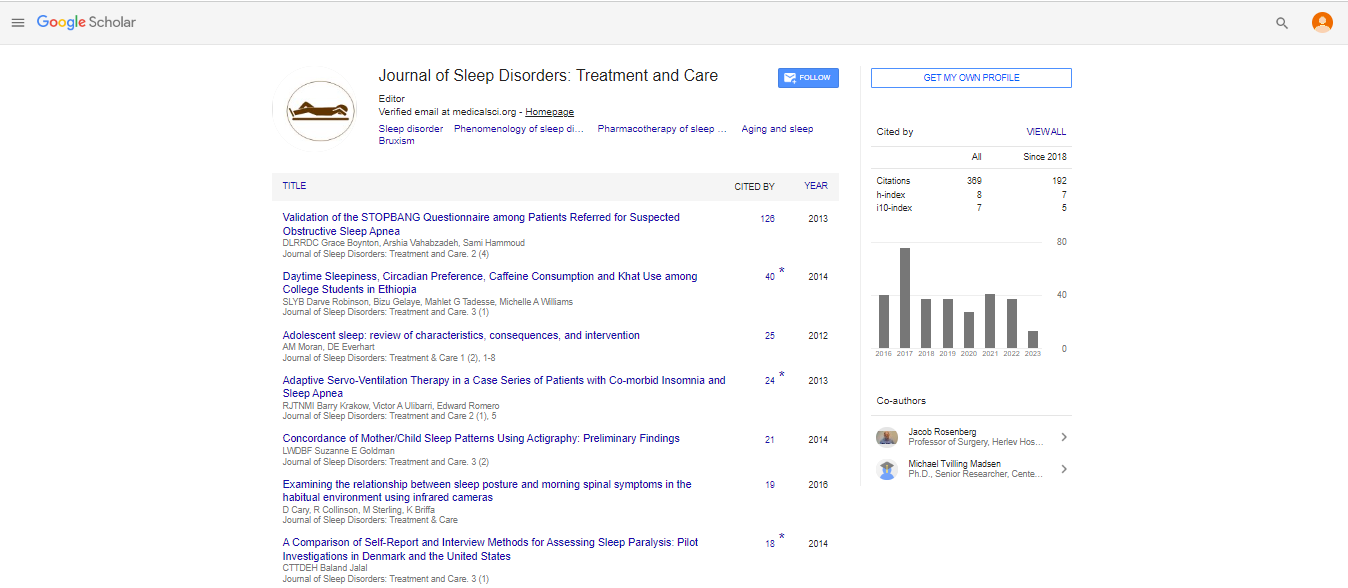
Perspective, J Sleep Disor Treat Care Vol: 11 Issue: 1
Using Pictograms to Make Structured Behavioral Observations of Youth with Restless Legs Syndrome Reproducible
Oliviero Bruni*
Department of Developmental Neurology and Psychiatry, Sapienza University, Rome, Italy
*Corresponding Author:
Oliviero Bruni
Department of Developmental Neurology and Psychiatry, Sapienza University, Rome, Italy
E-mail:oliviero.bruni@uniroma.it
Received date:Â 09 December, 2021, Manuscript No. JSDTC-22-56814;
Editor assigned date: 11 December, 2021, PreQC No. JSDTC-22-56814 (PQ);
Reviewed date: 25 December, 2021, QC No JSDTC-22-56814;
Revised date: 30 December, 2021, Manuscript No. JSDTC-22-56814 (R);
Published date: 09 January 2022, DOI: 10.4172/ 2325-9639.1000064
Citation: Bruni O (2022) Using Pictograms to Make Structured Behavioral Observations of Youth with Restless Legs Syndrome Reproducible. J Sleep Disor: Treat Care 11:1.
Keywords: Physiology of Sleep, Restless Leg Syndrome, Sleep Apnea
Description
Restless Leg Syndrome (RLS) is an uncomfortable or unpleasant tickling or twitching in the legs. Symptoms also occasionally occur in the arms or other parts of the body. To be classified as restless leg syndrome, symptoms must worsen when you're inactive or when you rest, worsen in the evening or nighttime, and improve when you walk or move. Approximately 10% of people in the United States have RLS, and the condition is more common in women. Most people with the disease are middle-aged or older, but children also have the condition. The disorder often goes unrecognized or misdiagnosed for years. There is no cure for restless leg syndrome, but we can reduce your discomfort and sleep disturbances and greatly improve your quality of life. Our goal is to reduce your symptoms. Symptoms can be intermittent or chronic. They can range from mild to incapacitating [1]. Some patients experience significant restlessness and difficulty falling asleep, causing sleep deprivation. The cause is unknown, but there is probably a genetic component because about half of people with RLS also have a close relative with the condition. Certain diseases and medical conditions such as the following may be a cause: Iron deficiency (anemia), Kidney failure, Diabetes mellitus, Rheumatoid arthritis, Peripheral neuropathy, Parkinson’s disease, Pregnancy, The following may make the symptoms worse: Medications used to treat nausea, Alcohol, Caffeine [2].
Restless Legs Syndrome
There is no medical test to diagnose restless leg syndrome. We make the diagnosis based on your medical history. Sometimes we use blood work or other testing to rule out other medical conditions, low levels of red blood cells or ferritin (a protein that stores iron in the tissues) [3]. In patients with more chronic or severe symptoms, prescription medications may be required. The same drug may not be helpful for all patients, and a particular medication may initially be helpful but become less effective over time. All medications have potential side effects and should be used only under the supervision of a physician trained in the treatment of this disorder [4]. Some medications used to treat restless leg syndrome act on a neurotransmitter in the brain called dopamine. These drugs include levodopa, pramipexole and ropinirole. In other cases, we may prescribe anti-convulsing or anti-seizure medications such as carbamazepine or gabapentin are. We occasionally use sedative medications or narcotic pain medications to help with sleep or to control pain [5]. It is suggested the main cause of restless leg syndrome is a problem using iron or the lack of iron in the brain. Many conditions have been associated with restless leg syndrome because of the iron problem, for example, diabetes, rheumatoid arthritis, pregnancy, kidney failure, Parkinson's disease, and iron deficiency [6]. Perpendicular axis of femoral stem and the center of femoral head. Last, the interpretation indicates the gyration angle between proximal and distal corridor of femurs. Depending on the length of implant neck, the medium neutralize and perpendicular height can be acclimated; also the perpendicular height can be acclimated according to depths of femoral stem into femurs [7].
RLS during Pregnancy
Restless leg syndrome is relatively common during pregnancy, especially in the second half of pregnancy. While most medications used to treat restless leg syndrome have not been adequately studied in pregnant women, the non-medication treatments and techniques described above can be very helpful [8]. Furthermore, avoiding caffeine, warm compresses, massage, and regular exercising according to the doctors' suggestions can be helpful. Restless legs syndrom causes a powerful urge to move your legs. Your legs become uncomfortable when you are lying down or sitting. Some people describe it as a creeping, crawling, tingling, or burning sensation. Moving makes your legs feel better, but not for long. RLS can make it hard to fall asleep and stay asleep. In most cases, there is no known cause for RLS. In other cases, RLS is caused by a disease or condition, such as anemia or pregnancy. Some medicines can also cause temporary RLS. Caffeine, tobacco, and alcohol may make symptoms worse. Lifestyle changes, such as regular sleep habits, relaxation techniques, and moderate exercise during the day can help. If those don't work, medicines may reduce the symptoms of RLS. Most people with RLS also have a condition called periodic limb movement disorder. PLMD is a condition in which a person's legs twitch or jerk uncontrollably, usually during sleep [9]. PLMD and RLS can also affect the arms. Restless legs syndrome may resolve if the underlying problem is addressed. Otherwise treatment includes lifestyle changes and medication. Lifestyle changes that may help include stopping alcohol and tobacco use, and sleep hygiene. Medications used include levodopa or a dopamine agonist such as pramipexole. RLS affects an estimated 2.5â??15% of the American population. Females are more commonly affected than males, and it becomes increasingly common with age [10].
References
- Jahdali HH, Qadhi WA, Khogeer HA (2009) Restless legs syndrome in patients on dialysis. Saudi J Kidney Dis Transpl 20: 378-385. [CrossRef], [Google Scholar], [Indexed]
- Applebee GA, Guillot AP, Schuman CC (2009) Restless legs syndrome in pediatric patients with chronic kidney disease. Pediatr Nephrol 24: 545-548. [CrossRef], [Google Scholar], [Indexed]
- Barriere G, Cazalets JR, Bioulac B (2005) The restless legs syndrome. Prog Neurobiol 77: 139-165. [CrossRef], [Google Scholar], [Indexed]
- Becker J, Becker F, Schindelbeck K, Koch P (2015). Restless-legs-syndrome and iron deficiency in patients with inflammatory bowel disease. J Crohns Colitis 9: 250-251. [CrossRef], [Google Scholar], [Indexed]
- Berger K, Luedemann J, Trenkwalder C (2004). Sex and the risk of restless legs syndrome in the general population. Arch Intern Med 164: 196-202. [CrossRef], [Google Scholar], [Indexed]
- Castaneda TR, Prado BM, Prieto D (2004) Circadian rhythms of dopamine, glutamate and GABA in the striatum and nucleus accumbens of the awake rat: Modulation by light. J Pineal Res 36: 177-185. [CrossRef], [Google Scholar], [Indexed]
- Catoire H, Dion PA, Xiong L (2011) Restless legs syndrome-associated MEIS1 risk variant influences iron homeostasis. Ann Neurol 70: 170-175. [CrossRef], [Google Scholar], [Indexed]
- Chen NH, Chuang LP, Yang CT, Kushida CA (2010). The prevalence of restless legs syndrome in Taiwanese adults. Psychiatry Clin Neurosci 64: 170-178. [CrossRef], [Google Scholar], [Indexed]
- Connor JR, Boyer PJ, Menzies SL (2003). Neuropath logical examination suggests impaired brain iron acquisition in restless legs syndrome. Neurology 61: 304-309. [CrossRef], [Google Scholar], [Indexed]
- Davis ID, Baron J, Oâ??riordan MA, Rosen CL (2005) Sleep disturbances in pediatric dialysis patients. Pediatr Nephrol 20: 69-75. [CrossRef], [Google Scholar], [Indexed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi