Research Article, J Sleep Disor Treat Care Vol: 9 Issue: 5
Various Anthropometric Measures and Sleep-Disordered Breathing in Obstructive Sleep Apnea Patients in Qazvin Province, Iran.
Veisi Hampa F1, Javadi M1, Jalilolghadr S2, yazdi Z3, Javadi A4 and Afaghi A1*
1Department of Nutrition, School of Health, Qazvin University of Medical Science, Iran
2Children Growth Research Center, Qazvin University of Medical Sciences, Iran.
3Metabolic Disease Research Centre, Faculty of Medicine, Qazvin University of Medical Science, Iran.
4Department of Social Sciences, Qazvin University of Medical Sciences, Iran
*Corresponding Author: Afaghi A
Department of Nutrition, School of Health, Qazvin University of Medical Science, Qazvin, Iran
E-mail: aafa2000@gmail.com
Received: March 16, 2020 Accepted: November 17, 2020 Published: November 24, 2020
Citation: Veisi Hampa F, Javadi M, Jalilolghadr S, Yazdi Z, Javadi A (2020) Various Anthropometric Measures and Sleep-Disordered Breathing in Obstructive Sleep Apnea Patients in Qazvin Province, Iran. J Sleep Disor: Treat Care 9:3.. doi: 10.37532/jsdtc.2020.9(5).241
Abstract
Objective: To investigate the correlation between different anthropometric measures and sleep disorder breathing (SDB) as measured by apnea / hypopnea index (AHI) in obstructive sleep apnea (OSA) patients. Also to find out the most correlated anthropometric measure with SDB. Methods: We evaluated 80 patients with suspected OSA underwent polysomnography and anthropometric measurements including body mass index (BMI), waist–hip ratio (WHR), waist to height ration (WHtR), waist, and hip circumference. Results: A statistically significant correlation was found between the anthropometrics variables (BMI, WHtR, W, and WHR) relative to the AHI (r = 0.516, p< 0.001; r = 0.477, p = 0.002; r = 0.333, p=0.024; and r = 0.302, p=0.042 respectively) in men. These correlations were confirmed by observed significant negative correlation of the mentioned anthropometrics variables and oxygen saturations (SMED, SMIN). No significant correlation was found between anthropometrics and SDB in women. The step-wise linear regression showed that increasing BMI has the most effect on severity of AHI followed by WHR in men (Beta = 0.469, and 0.22 respectively). Conclusion: BMI is the most reliable obesity indicator that significantly correlated with SDB. BMI is more appropriate indicator than WHtR or W to predict SDB.
Keywords: Anthropometric measures, obstructive sleep Apnea, sleep disorder breathing, apnea / hypopnea index, race, craniofacial.
Abbreviations
Apnea / Hypopnea Index (AHI); Sleep Disorder Breathing (SDB); Obstructive Sleep Apnea (OSA); Body Mass Index (BMI); Waist–Hip Ratio (WHR); Waist to Height Ration (WHtR); Neck Circumference (NC); Abdominal Circumference (AC); Waist Circumference (WC); Obstructive Sleep Apnea-hypopnea Syndrome (OSAHS); Mean Oxygen Saturation (SMED); Minimum Oxygen Saturation (SMIN).
Introduction
The Obstructive Sleep Apnea-hypopnea Syndrome (OSAHS) is a common disorder experienced by 4% of men and 2% of women. It is caused by structural and functional abnormalities that promote obstruction of the upper airways during sleep [1]. Clinical symptoms associated with this disorder include obesity, high daily sleepiness, night snoring, and neuropsychiatric disorders. The prevalence of obstructive sleep apnea increases with age with its maximum in middle-aged adults [2]. This Sleep Disordered Breathing (SDB) can reduce sleep quality and therefore affect the quality of daily function [3]. Obesity is a major risk factor of OSAHS [1,4]. Epidemiological studies have shown that there is a strong relationship between OSAHS and obesity. OSAHS prevalence was 30% in obese and 50 – 98% in morbidly obese subjects [5]. There are several anthropometric methods for measuring obesity such as Body Mass Index (BMI), Neck Circumference (NC), Abdominal Circumference (AC), Waist Circumference (WC), Waist to Hip Ratio (WHR) and Mallampati grades. Thus, it is important to determine which anthropometric and obesity measures best correlate with OSAHS [6].
There have been various studies. In two different studies of Turkish and Brazilian populations, the researchers found the most significant correlation to be between NC and SDB [7,8]. In a Korean population the WHR had the most significant correlation with OSA in both sexes [9]. In a San Diego - California study, the WC, NC, WHR and BMI were significantly correlated with SDB in both sexes with the strongest correlation related to WC followed by NC in both sexes [6]. Moreover, in the study of Korean men, BMI and WHR showed the strongest correlation with Apnea-Hypopnea Index (AHI) respectively in both the whole group and the BMI < 25 group [10]. Several other studies have reported the BMI to be the appropriate indicator of obesity to correlate with SDB [11-13]. However, other influences including ethnicity, craniofacial and cephalometric deviation on SDB are reported too [1,14].
For example, a Japanese study discusses the prevalence of anomaly in craniofacial morphology in normal weight subjects with mild SDB [15]and in another study, Chinese OSA patients had more craniofacial deviations than Caucasians with similar OSA severity [1].
The findings in different populations are not consistent and different studies have introduced different obesity measures that best correlate with SDB. There were no studies in Iran to demonstrate the effect of anthropometric measurement on SDB. Therefore, the aim of this study was to find out the obesity measures that best correlate with SDB in Iranian obstructive sleep apnea patients.
Subjects and Methods
Subject
Eighty adult subjects (47 male and 33 female) suspected of having OSAS were recruited from among 150 subjects screened. In the first medical visit, subjects answered the Epworth sleep disorder screening questionnaire [16]. Those with a score ≥ 10 indicating excessive day time sleepiness were included in the study [17]. Subjects were excluded if they had a self- reported current history of chronic diseases such as heart and lung disease, diabetes, thyroid disorder, pregnancy and if they were under 18 years old. The study was approved by the Human Research Committee of Qazvin University of Medical Science. Written informed consent for publishing patient information was obtained from participants.
Polysomnography
Full night polysomnography (using a DeVilbiss-USA sleep system) with an International 10–20 electrode placement (F4/M1, C4/M1, O2/ M1), leg electromyogram (to exclude limb movement disorders), left and right electrooculogram and submental electromyogram recording, was performed.The Respiratory Inductance Plethysmography method (respiratory effort band) was used to evaluate pulmonary ventilation by measuring the movement of the chest and abdominal wall. The respiratory flow (through an oronasal thermal sensor) and nasal pressure were both monitored for detection of apnea and hypopnea respectively. All polysomnography and respiratory event recording was performed on the familiarization night and subsequently on the study night and evaluated for sleep stages and respiratory events. A respiratory event was considered to be apnea if the peak signal excursion dropped by ≥ 90% of the pre-event baseline for a duration ≥ 10 seconds. Hypopnea was defined as abnormal breathing if the nasal pressure sensor peak signal excursion dropped by ≥ 30% of the pre-event baseline for a duration ≥ 10 seconds and there was a > 3% peripheral capillary oxygen desaturation from the pre-event baseline or the event was associated with an arousal. The AHI was defined as the number of apneal and hypopnea events that occurred per hour of sleep and scored using AASM guideline [18].
Anthropometric Measurements
All anthropometric parameters were measured before familiarization overnight polysomnography. To evaluate BMI (kg/ m2), we measured height (m) and weight (kg). The NC was measured horizontally at just inferior the Adam’s apple. The WC was measured at the narrowest part of the trunk of the body. Hip circumference was determined as the maximum value over the buttocks. The position of the tongue relative to the palate, was evaluated using the modified Mallampati index (Patients were classified as follows: class I = complete visualization of uvula, tonsils, and palatal arches; class II = complete visualization of the uvula while the tonsils and arches are partly hidden; class III = visualization of some of the soft palate but not tonsils, pillars, distal soft palate, or base of the uvula; and class IV = only the hard palate is visible [19].
Waist to Hip Ratio (WHR), Waist to height ratio (WHtR), BMI were calculated using the following formulae: WHtR = WC (cm)/ height (cm); WHR = WC (cm)/HC (cm); BMI = weight (kg)/height (m2).
Statistical Analysis
A sample size calculation was based on a correlation coefficient obtained between AHI and body mass index (r = o.3) powered at 80% and with a confidence of 95% in Pinto’s (2011) study of anthropometric data as predictors of obstructive sleep apnea severity [7]. We estimated that a sample size of 80 would be appropriate for our study. Normality of distribution of data was inspected before using parametric statistics with SPSS version 16. Data were reported as Mean ± SDs. Pearson's correlation coefficient was used to determine the effect of the anthropometric measurement on the SDB parameter. Repeated measurement analysis of variance (ANOVA) was conducted to explore the effect of the Mallampati on SDB.
Results
Sleep recording on the study night was performed from 11 PM to 5 AM. The participants included 47 males (58.8%) and 33 females (41.2%) with age range of 21 - 83 years. One male patient was excluded from the study due to an observed artefact in sleep recording. The mean values for age, anthropometric measures and SDB parameters as measured by AHI are shown in (Table 1). A statistically significant correlation was found between the anthropometric variables (BMI, WHtR, WC, and WHR) with AHI (r = 0.516, p< 0.001; r = 0.477, p = 0.002; r = 0.333, p=0.024; and r = 0.302, p=0.042 respectively) in men. This correlation was confirmed by observed significant negative correlation of the mentioned anthropometric variables and oxygen saturations (SMED, SMIN). No significant correlation was found between anthropometrics and AHI in women (Table 2). The step-wise linear regression showed that increasing BMI has the most effect on severity of AHI in men (β = 0.469) (Table 3).
| Variable | Female | Male |
|---|---|---|
| M±SD | M±SD | |
| (n=33) | (n=47) | |
| Age | 54.6±11.3 | 45.4±12.8 |
| BMI (body mass index) | 34.2±8.2 | 30.2±5.8 |
| WHtR (Waist to height ratio) % | 67.7±12.3 | 60.3±6.9 |
| WHR (Waist to hip ratio) | 0.89±0.04 | 0.91±0.07 |
| Waist circumference | 107.3±15.9 | 104.3±11.1 |
| Neck circumference | 43.0±4.4 | 44.2±4.1 |
| AHI (Apnea hypopnea index) | 30.4±18.4 | 34.0±18 |
| SMED (Mean oxygen saturation) | 89.0±6.4 | 90.2±5.2 |
| SMIN (Minimum oxygen saturation) | 74.3±12.9 | 74.2±12.6 |
| Mallampati | ||
| I | - | - |
| II | 4 (12.1%) | 7 (14.9%) |
| II | 9 (27.3%) | 18 (38.3%) |
| IV | 20 (60.6%) | 22 (46.8%) |
Table 1: Description of scalar variables.
| SMIN | SMED | AHI | Gender | Variable |
|---|---|---|---|---|
| r (p) | r (p) | r (p) | ||
| -0.089 (0.550) | -0.168 (0.258) | 0.113 (0.455) | Male | Age |
| -0.449 (0.009) | -0.223 (0.212) | 0.358 (0.041) | Female | |
| -0.410 (0.004) | -0.251 (0.089) | 0.516 (0.000) | Male | BMI |
| -0.266 (0.134) | -0.175 (0.329) | 0.265 (0.136) | Female | |
| -0.416 (0.004) | -0.332 (0.023) | 0.333 (0.024) | Male | waist circumference |
| -0.215 (0.230) | -0.299 (0.091) | 0.185 (0.303) | Female | |
| -0.367 (0.011) | -0.457 (0.001) | 0.302 (0.042) | Male | Waist hip ratio |
| -0.111 (0.538) | -0.255 (0.152) | -0.203 (0.256) | Female | |
| -0.484 (0.001) | -0.457 (0.001) | 0.447 (0.002) | Male | WHtR |
| -0.240 (0.179) | -0.282 (0.112) | 0.166 (0.355) | Female |
Table 2: Correlation of anthropometric measurements with SDB severity separated by gender.
| Parameters | B | SE | β | T | P |
|---|---|---|---|---|---|
| BMI | 2.952 | 1.229 | 0.469 | 2.403 | 0.02 |
| WC | 0.082 | 1.052 | 0.025 | 0.078 | 0.94 |
| WHR | 104.23 | 71.526 | 0.22 | 1.457 | 0.15 |
| WHtR | -0.701 | 166.37 | -0 | -0 | 1 |
| Constant | -137.68 | 59.506 | -2.31 | 0.03 | |
| R= 0.564a | R SQUARED = 0.318 | Adjusted R Squared = 30.59062 | |||
Table 3: Evaluation of effect of anthropometric measures on SDB using step-wise linear regression analysis.
The Mallampati measurements classified as grade 1 (n=0), grade 2 (n=11, 13.8%), grade 3 (n=27, 33.8%) and grade 4 (n=41, 52.5%). Mean AHI and respiratory disturbance index (RDI) increased more than twofold among total patients in grade 3 and 4 compared to grade 2 of the Mallampati (Table 4). The AHI and RDI severity significantly increased in grade 3 and 4 compared to grade 2 of the Mallampati in total patients (P= 0.044, and 0.039 respectively) (Table 4).
| MLPT | N | Mean | SD | P | |
|---|---|---|---|---|---|
| AHI | 2 | 11 | 17 | 5 | 0.04 |
| 3 | 27 | 36.22 | 15 | ||
| 4 | 41 | 38 | 14 | ||
| Total | 79 | 32 | 20 | ||
| SMIN | 2 | 11 | 80 | 6.44 | 0.28 |
| 3 | 27 | 73.62 | 12.4 | ||
| 4 | 42 | 73.21 | 13.8 | ||
| Total | 80 | 74.28 | 12.7 | ||
| SMED | 2 | 11 | 91.48 | 2.99 | 0.38 |
| 3 | 27 | 90.24 | 4.57 | ||
| 4 | 42 | 88.95 | 6.86 | ||
| Total | 80 | 89.73 | 5.77 | ||
| RDI | 2 | 11 | 24.01 | 23.4 | 0.04 |
| 3 | 27 | 53.92 | 33.6 | ||
| 4 | 41 | 49.78 | 34.6 | ||
| Total | 79 | 47.61 | 34 |
Table 4: Association between the modified Mallampati grades and SDB parameters in total patients
Discussion
In this study, there were significant correlations of BMI, WHtR, WC, and WHR to the AHI. The step-wise linear regression showed that increasing BMI has the most effect on severity of AHI in men (β = 0.469) (Table 3).
Different studies have introduced different anthropometric measures as the most significant risk factor for SDB. In three population studies, Turkish [8], Brazilian - Sao Paulo [7] and Korean - Seoul [9] a strong correlation was found between the variables AHI and NC [7-9]. In another study of Korean males, BMI showed the strongest correlation with AHI across all male subjects [10]. However, association between AHI and NC did not differ by ethnicity [20].
Several racial/ethnic international studies including Southerlan (2019) and Chen (2016) in the MESA study of the association between anthropometric measures and SDB severity, have focused on the BMI variable and found a strong significant association between BMI and AHI [20-24].
Although anthropometric measures strongly correlate with SDB, other parameters such as gender, age and race of the population may also affect SDB [11]. Davidson and Patel [6]in their California population study revealed that only 50% of patients having AHI > 5 were clinically obese. And the craniofacial factor strongly correlated to SDB in leaner Caucasian men [25] and Chinese men and women [26].
A Japanese study reported that anomalies in craniofacial morphology and occlusion are more prevalent in normal weight subjects than obese subjects with mild SDB [15] as well as severe OSAS patients [27]. Ethnicity influences OSA craniofacial phenotype, and comparison of Chinese and Caucasian subjects with similar degrees of OSA severity showed that Caucasian patients were more obese, while Chinese patients had more craniofacial deviations [1]. And magnetic resonance imaging (MRI) cephalometry showed that having a small and shallow mandible is an independent risk factor for OSA in males [28].
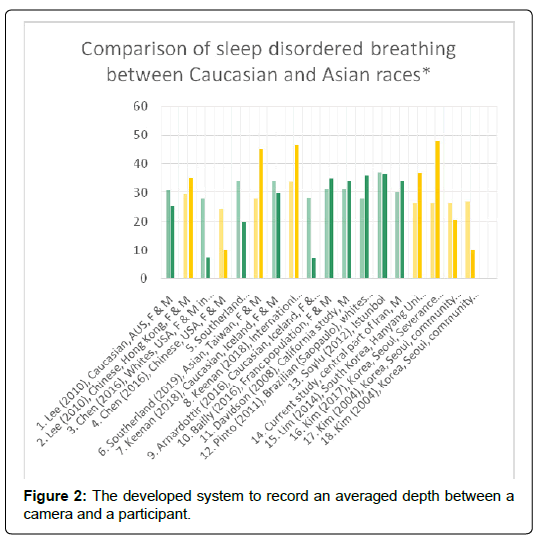
In this regard, it has been demonstrated that the mean BMI among SDB patients (AHI ≥ 5) of similar age-group in Korean and Chinese men and women was 27 Kg/m2. For Indian men it was 31 and for African American men and women 32 Kg/m2. Caucasian men and women with mean BMI = 33 Kg/m2 had the highest BMI among the different ethnic groups of the SDB patients [11]. According to different studies, Asian OSA patients mainly have craniofacial skeletal deviation, African American patients display more obesity and enlarged upper airway soft tissue abnormalities, while Caucasians show evidence of both skeletal and soft tissue deviation[1]. American studies, which have compared Asian and Caucasian OSA patients having a similar severe range of AHI, have found that Asian patients are younger, with a lower mean BMI than Caucasians (26.6 ± 3.7, and 30.7 ± 5.9 Kg/m2 respectively) [23]. Also, it has been reported that the severity of illness in Asian OSA patients is greater than that in Caucasian patients when matched for age, gender and BMI [29]. Craniofacial skeletal deviation between humans has been found to be largely due to differing patterns of biological inheritance; crossanalysis of osteological variables and genome association has identified specific genes which control this craniofacial deviation [30]. A recent genetic study published in Nature (2019) showed that West Asians (Iran, Turkey, Iraq, Afghanistan,) Europeans, Northern Africans and South Asians (Caucasoid group), are closely related to each other and can be distinguished from Mongoloid and Negroid populations [31]. (Figure 1) shows a geographical diversity of racial / ethnic groups. There is evidence showing that despite the existence of internal heterogeneity in a population, a group can form a geographical cluster [31-33]. Several studies, International included, have confirmed the influence of ethnicity / craniofacial deviation on SDB. (Figure 2) shows the influence of ethnicity / craniofacial deviation in several studies conducted among various ethnic groups. Asians / Chinese of similar or younger age than Caucasians and with lower BMI/Kg/m2 demonstrated higher AHI than Caucasians in comparison studies [20, 21, 23, 34]. And incremental changes in BMI were associated with larger increases in AHI among Chinese than Caucasian [21,34]. Also, in Arnardottir (2016) and Kim (2004), two separate communitybased studies performed in Iceland (Caucasian) and Korea, (with nearly similar age and BMI groups), the Korean group showed higher AHI than the Caucasian group [35,36].
Other studies conducted in Istanbul, Sao Paolo, California and France having a mean range BMI = 28-37, showed a mean range of AHI = 34-37. Our findings in this current study are consistent with these studies and the four Caucasian comparison studies in (Figure 2).
While there is internal heterogeneity in the Iranian population, it forms a geographical cluster [31-33]. The Iranian population comprises numerous ethnic groups. The Persians in Central Iran and Azeri’s in Northern Iran are Caucasian and make up around 81% of Iran's population [33]. These two groups along with 3 other small groups (Kurds, Lures and Arabs) make up the existence of a Central Iranian Cluster (CIC) and amount to about 96% of the Iranian population [32]. The genetic diversity found in the CIC Group is comparable with the population groups found in the South Caucasus, Anatolia and Europe [32]. The CIC Group forms a distinct genetic entity, despite internal heterogeneity and on a global scale it is identified as being close to European [32]. The population we studied is in the city of Qazvin (Central Iran), 120 km north west of the Capital Tehran and within the CIC. The subject population’s genetic ethnic diversity and craniofacial structure is accordingly representative of the CIC.
Clinical study of association between anthropometrics measures and SDB in Iran is rare. To our knowledge, this is the first attempt (in the region of our study) to survey the racial/ethnic differences in the association between anthropometric measures and the severity of SDB using an ethnographic map. Importantly, our data reveals an ethnic / craniofacial similarity between the population in this current study with the European and Turkish population (Figure 1) [31,32] and consistency of SDB severity between our study subjects and the European population (Figure 2). We expect that our finding will be useful to future mapping studies which in turn will contribute to a better global understanding of the association of ethnicity and SDB, informing SDB protocols and definitions. We anticipate it may help those involved in comparing and interpreting data and determining the anthropometric predictors of SDB.
Conclusion
We are aware of ways in which our study could be expanded. The female sample sizes were small due to recruitment difficulties. Because of this we were unable to find any true correlation of anthropometric measures with SDB in this group of patients. We did not exclude patients with previous upper airway surgery or upper airway malformations. Finally, although not currently available in a suitable format for this paper, a future study might utilize more recent ethnographic data.
Declaration of conflicting interests
The authors declare that there is no conflict of interest with respect to the research, authorship and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- Sutherland K, Lee RW, Cistulli PA (2012) Obesity and craniofacial structure as risk factors for obstructive sleep apnoea: impact of ethnicity. Respirology 17: 213-222.
- Lim LL, Tham KW, Fook-Chong S (2008) Obstructive sleep apnoea in Singapore: polysomnography data from a tertiary sleep disorders unit. Ann Acad Med Singap 37: 629-636.
- Aguiar M, Valenca J, Felizardo M, Caeiro F, Moreira S et al. (2009) Obstructive sleep apnoea syndrome as a cause of road traffic accidents. Rev Port Pneumol 15: 419-431.
- Schwartz AR, Patil SP, Laffan AM, Polotsky V, Schneider H et al. (2008) Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc 5: 185-192.
- Simpson L, Mukherjee S, Cooper MN, Ward KL, Lee JD et al. (2010) Sex differences in the association of regional fat distribution with the severity of obstructive sleep apnea. Sleep 33: 467-474.
- Davidson TM, Patel MR (2008) Waist circumference and sleep disordered breathing. Laryngoscope 118: 339-347.
- Pinto JA, De Mello Godoy LB, Marquis VWPB, Sonego TB, Leal CdFA et al. (2011) Anthropometric data as predictors of obstructive sleep apnea severity. Brazilian journal of otorhinolaryngology. 77: 516-521.
- Soylu AC, Levent E, Sarıman N, Yurtlu S, Alparslan S et al. (2012) Obstructive sleep apnea syndrome and anthropometric obesity indexes. Sleep Breath 16:1151-1158.
- Lim Y-H, Choi J, Kim KR, Shin J, Hwang KG et al. (2014) Sex-specific characteristics of anthropometry in patients with obstructive sleep apnea: neck circumference and waist–hip ratio. Ann Otol Rhinol Laryngol 123: 517-523.
- Kim J-H, Koo YC, Cho HJ, Kang JW (2017) Relationship between various anthropometric measures and apnea-hypopnea index in Korean men. Auris Nasus Larynx 45: 295-300.
- Young T, Peppard PE, Taheri S (2005) Excess weight and sleep-disordered breathing. Journal of applied physiology 99:1592-1599.
- Newman AB, Foster G, Givelber R, Nieto FJ, Redline S et al. (2005) Progression and regression of sleep-disordered breathing with changes in weight: The Sleep Heart Health Study. Arch Intern Med 165: 2408-2413.
- Van Boxem TJ, De Groot GH (1999) Prevalence and severity of sleep disordered breathing in a group of morbidly obese patients. Neth J Med 54: 202-206.
- Paulo de Tarso MB, Ferreira Filho ES, de Araujo TME, Neto JMM, de Sa Borges NE et al. (2013) Correlation of cephalometric and anthropometric measures with obstructive sleep apnea severity. Int Arc otorhinolaryngology 17: 321-328.
- Pahkala R, Puustinen R, Tuomilehto H, Ahlberg J, Seppä J (2011) Risk factors for sleep-disordered breathing: the role of craniofacial structure. Acta Odontol Scand 69: 137-143.
- Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14: 540-545.
- Patil SP, Schneider H, Schwartz AR, Smith PL (2007) Adult obstructive sleep apnea: pathophysiology and diagnosis. Chest 132: 325-337.
- Berry RB, Brooks R, Gamaldo CE (2017) The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version 2.4. Darien, IL. American Academy of Sleep Medicine.
- Wang W-M, Hsu Y-B, Lan M-Y, Yang M-C, Huang T-T et al. (2018) The Relationship Between Modified Mallampati Score, Müller’s Maneuver and Drug-Induced Sleep Endoscopy Regarding Retrolingual Obstruction. Ann Otol Rhinol Laryngol 127:463-469.
- Sutherland K, Keenan BT, Bittencourt L, Chen N-H, Gislason T et al. (2019) A global comparison of anatomic risk factors and their relationship to obstructive sleep apnea severity in clinical samples. J Clin Sleep Med 15:629-639.
- Lee RW, Vasudavan S, Hui DS, Prvan T, Petocz P et al. (2010) Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep 33:1075-1080.
- Keenan BT, Kim J, Singh B, Bittencourt L, Chen N-H et al. (2018) Recognizable clinical subtypes of obstructive sleep apnea across international sleep centers: a cluster analysis. Sleep 41: zsx214.
- Li KK, Powell NB, Kushida C, Riley RW, Adornato B et al. (1999) A comparison of Asian and white patients with obstructive sleep apnea syndrome. Laryngoscope 109:1937-1940.
- Seidell J (2010) Waist circumference and waist/hip ratio in relation to all-cause mortality, cancer and sleep apnea. Eur J Clin Nutr 64: 35-41.
- Dempsey JA, Skatrud JB, Jacques AJ, Ewanowski SJ, Woodson BT et al. (2002) Anatomic determinants of sleep-disordered breathing across the spectrum of clinical and nonclinical male subjects. Chest 122: 840-851.
- Chang E-T, Shiao G-M (2008) Craniofacial abnormalities in Chinese patients with obstructive and positional sleep apnea. Sleep Med 9: 403-410.
- Ito D, Akashiba T, Yamamoto H, Kosaka N, Horie T (2001) Craniofacial abnormalities in Japanese patients with severe obstructive sleep apnoea syndrome. Respirology 6:157-161.
- Chi L, Comyn F-L, Mitra N, Reilly MP, Wan F et al. (2011) Identification of craniofacial risk factors for obstructive sleep apnoea using three-dimensional MRI. Eur Respir J 38: 348-358.
- Ong K, Clerk A (1998) Comparison of the severity of sleep-disordered breathing in Asian and Caucasian patients seen at a sleep disorders center. Respir Med 9: 843-848.
- Adhikari K, Fuentes-Guajardo M, Quinto-Sánchez M, Mendoza-Revilla J, Chacón-Duque JC et al. (2016) A genome-wide association scan implicates DCHS2, RUNX2, GLI3, PAX1 and EDAR in human facial variation. Nat commun 7: 11616.
- Pakstis AJ, Gurkan C, Dogan M, Balkaya HE, Dogan S et al. (2019) Genetic relationships of European, Mediterranean, and SW Asian populations using a panel of 55 AISNPs. Eur J Hum Genet 27: 1885-1893.
- Mehrjoo Z, Fattahi Z, Beheshtian M, Mohseni M, Poustchi H et al. (2019) Distinct genetic variation and heterogeneity of the Iranian population. PLoS Genet 15: e1008385.
- Chen X, Wang R, Lutsey PL, Zee PC, Javaheri S et al.(2016) Racial/ethnic differences in the associations between obesity measures and severity of sleep-disordered breathing: the Multi-Ethnic Study of Atherosclerosis. Sleep Med 26: 46-53.
- Arnardottir ES, Bjornsdottir E, Olafsdottir KA, Benediktsdottir B, Gislason T (2016) Obstructive sleep apnoea in the general population: highly prevalent but minimal symptoms. Eur Respir J 47:194-202.
- Kim J, In K, Kim J, You S, Kang K et al. (2014) Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am Journal Respir Crit Care Med 170: 1108-1113.
- Bailly S, Destors M, Grillet Y, Richard P, Stach B et al. (2016) Obstructive Sleep Apnea: A Cluster Analysis, PLOS ONE.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi