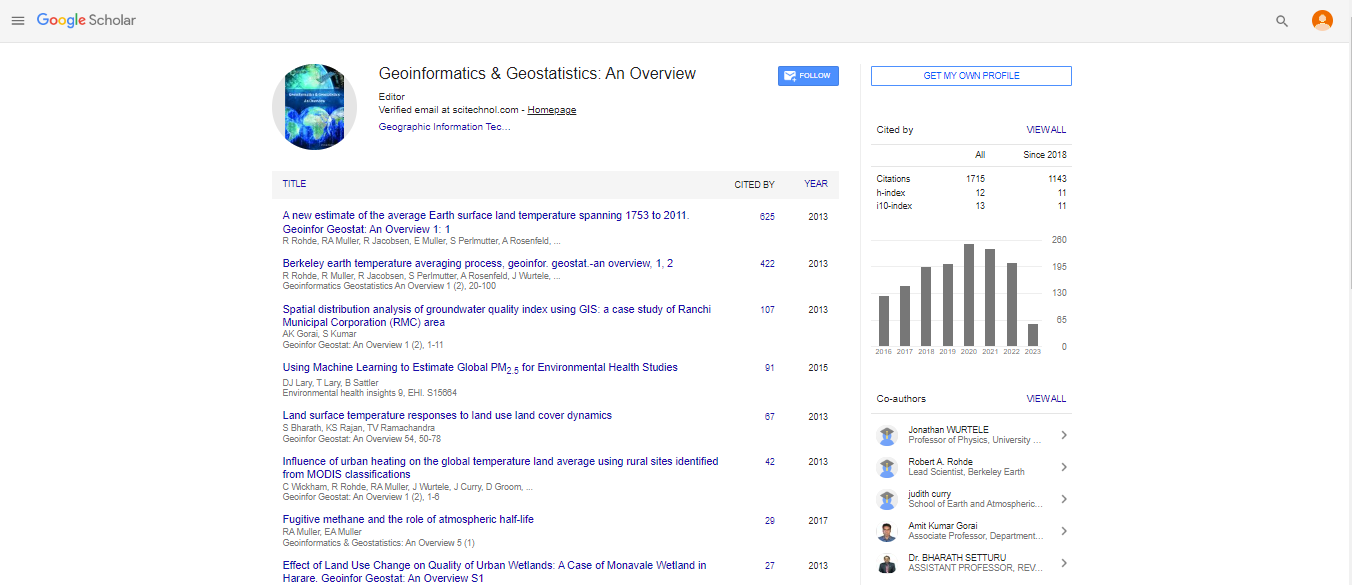
Review Article, Geoinfor Geostat An Overview Vol: 4 Issue: 4
Traffic-Related Air Pollution Exposure and Asthma, Hayfever, and Allergic Sensitisation in Birth Cohorts: A Systematic Review and MetaAnalysis
| Joachim Heinrich1,2*, Feng Guo2 and Elaine Fuertes3,4,5 | |
| 1Institute of Epidemiology I, Helmholtz Zentrum München - German Research Center for Environmental Health, Neuherberg, Germany | |
| 2Institute and Outpatient Clinic for Occupational, Social and Environmental Medicine, University Hospital Munich, Ludwig Maximillian University Munich, Member of German Center for Lung Research (DZL) | |
| ISGlobal, Centre for Research in Environmental Epidemiology (CREAL), Barcelona, Spain | |
| 4Universitat Pompeu Fabra (UPF), Barcelona, Spain | |
| 5CIBER Epidemiología y Salud Pública (CIBERESP), Barcelona, Spain | |
| Corresponding author : Joachim Heinrich
Institute and Outpatient Clinic for Occupational, Social and Environmental Medicine, University Hospital Munich, Ludwig Maximillian University Munich, Ziemssenstr. 1, D-80336 Munich, Germany Tel: +49 89 440053251 E-mail: joachim.heinrich@med.uni-muenchen.de. |
|
| Received: May 26, 2016Accepted: August 22, 2016 Published: August 26, 2016 | |
| Citation: Heinrich J, Guo F, Fuertes E (2016) Traffic-Related Air Pollution Exposure and Asthma, Hayfever, and Allergic Sensitisation in Birth Cohorts: A Systematic Review and Meta-Analysis. Geoinfor Geostat: An Overview 4:4. doi:10.4172/2327-4581.1000153 |
Abstract
Background: The causal role of ambient air pollution for asthma and allergic conditions continues to be debated. We provide a systematic review and meta-analysis of birth cohort studies with follow-ups from birth to adolescence.
Methods: In a previous systematic review by Bowatte et al. 19 birth cohort studies published from 1960 to March 2014 were identified. Using the same methodology, we extended this search up to January 2016, which allowed several key new studies to be considered. Random effects meta-analysis was used to obtain combined estimates.
Results: In total, 338 references published between April 2014 and January 2016 were identified. Of these, 88 were duplicates and 216 studies did meet the inclusion criteria. Manual searches identified 4 additional papers. These new studies were added to those previously identified by Bowatte et al. Ultimately, 27 eligible papers were included in the systematic review, 15 of which could be used in meta-analyses. Combined associations between asthma with particulate matter with a diameter of less than 2 µm (PM2.5) [1.11 (95% CI 0.97, 1.26) per 2 µg/m3 increment] and nitrogen dioxide (NO2) [1.08 (95% CI 0.96, 1.20) per 10 µg/m3 increment] were not significant. Also for wheeze, the combined association was not significant neither for PM2.5 [1.13 (95% CI 1.00, 1.28) per 2 µg/m3 increment] nor for NO2 [1.08 (95% CI 0.98, 1.18) per 10 µg/m3 increment]. None of the combined associations with allergen sensitization or hay fever reached statistical significance. There were too few birth cohort studies on eczema to conduct a metaanalysis.
Conclusion: Despite the existence of a wealth of high quality, large, longitudinal birth cohort studies, the epidemiological evidence supporting an association between traffic-related air pollution with asthma and other allergic health outcomes remains insufficient to confirm a causal association.
Keywords: Traffic-related air pollution; NO2 ; PM2.5; Asthma; Hayfever; Allergic sensitization; Wheeze; Children; Adolescents; Birth cohorts
Keywords |
|
| Traffic-related air pollution; NO2; PM2.5; Asthma; Hayfever; Allergic sensitization; Wheeze; Children; Adolescents; Birth cohorts | |
Introduction |
|
| Exposure to particulate matter with a diameter less than 2.5 μm (PM2.5) and less than 10 μm (PM10), as well as nitrogen dioxide (NO2), is consistently associated with increased asthma exacerbation (in terms of increased respiratory symptoms), lower lung function and higher medication needs in children and adults [1]. However, the potential for these ambient air pollutants to induce asthma and other allergic conditions continues to be controversially debated in epidemiological research, with the strength of the evidence oscillating with time over the last two decades. The cross-sectional study by Wjst et al. [2] was one of the first to report that children attending schools in areas with high road traffic had poor respiratory health. This observation stimulated the need for improved exposure assessment strategies and studies with prospective designs. Indeed, heaps of study results and several reviews have been published during the last 20 years. | |
| The first comprehensive expert panel review, organized by the World Health Organization, concluded that the results from epidemiological studies did not support the notion that exposure to traffic-related air pollution (TRAP) caused asthma, hayfever and allergic rhinitis [3,4]. Two later reviews by Salam et al. [5] and Braback and Forsberg [6] concluded that the evidence for a causal role of traffic-related air pollution exposure on asthma onset was suggestive. One year later in 2010, the most comprehensive review to date was published by the Health Effects Institute [7]. This report made a more conservative conclusion, stating that the evidence was not sufficient to support a causal role of ambient air pollutants on asthma onset, a view that was shared by another review published two years later by Gowers et al. [8]. In contrast, Gasana et al. [9] reported increased risks for the association between nitrogen dioxide and incident childhood asthma and between particulate matter and wheeze in a systematic review and meta-analysis. Interestingly, these two latter systematic reviews were published in the same year but came to different conclusions. Only a few years later, two more reviews were published but with consistent conclusions. The systematic review by Anderson et al. [10] in 2013 included cross-sectional and prospective studies and reported an increased risk between traffic-related air pollution and asthma in children. In 2015, Bowatte et al. [11] focused on prospective birth cohorts only and came to the same conclusion. | |
| While most of the previous reviews were not restricted to studies with longitudinal designs, birth cohort studies are ideal for assessing the existence of possible causal associations due to their prospective study design, individual-based exposure assessments and repeated outcome measurements throughout life. Presumably, this was the reason why the most recent review by Bowatte et al. included only studies based on birth cohorts. However, since a few relevant papers were omitted in this systematic review (Fuertes and Heinrich) [12] and because several other papers with extended follow-ups were published since the end of the search period used in Bowatte et al. an extension of this latest effort is urgently needed. In order to increase comparability, we followed the same search strategy used by Bowatte et al. The current work thus provides a complete review of the evidence derived from birth cohort studies with a specific focus on early life exposure published up to January 2016. Combined meta-analytic effect estimates for the associations between NO2 and PM2.5 exposure with asthma, wheeze, hayfever, allergic sensitisation and eczema are presented. | |
Materials and Methods |
|
| This review is an extension of the most recent systematic review by Bowatte et al. [11], which considered studies published from 1960 to March 2014, and ultimately included 19 publications. We performed an identical systematic literature search for the period between April 2014 and January 2016, which was in accordance with PRISMA guidelines for systematic reviews and MOOSE guidelines for meta-analyses [13,14]. In addition, manual searches were conducted to identify additional studies, including those omitted in Bowatte et al. [12]. | |
| Search strategy | |
| Searches were performed in three electronic databases (MEDLINE-PubMed, EMBASE and ISI Web of science) for studies published between April 2014 and January 2016, using the following combination of terms, which are identical to the keywords used in Bowatte et al. [11] (major roads, roads, roadways, motorways, traffic, traffic exposure/exhaust, automobile exhaust, traffic pollution/ pollutants, traffic related pollutants/air pollutants, air pollution, living near motorways/freeways/roadways, distance to major roads/ highway, proximity to roadways/ major road/highway/freeway, vehicle emissions, traffic emissions, automobile emissions) AND (childhood OR early life) AND (asthma, respiratory tract diseases, respiratory symptoms, respiratory illnesses, respiratory health chronic obstructive pulmonary disease, chronic obstructive lung disease, emphysema, chronic bronchitis, wheeze, shortness of breath, asthma symptoms, IgE, allergic sensitisation, hayfever, eczema, allergic rhinitis and skin prick test). We also manually searched the reference list of extracted papers and previous reviews. Duplicates were removed. If a cohort published associations between traffic exposures and health outcomes at different ages (either independently or as part of a collaboration), only the effect estimates from the longest follow up (i.e. highest age) were used. We contacted correspondent authors of selected studies if the effect estimates were not originally published in a format that could be used in a meta-analysis (for example, in the case of a collaborative analysis). | |
| Outcome definitions | |
| Information on asthma, wheeze, hayfever and eczema are mostly based on parental reported doctor diagnoses. Questions for asthma and hayfever usually referred to the single year before follow-up, although occasionally a longer period was also considered. , For wheeze, only data on symptoms occurring during the last 12 months was used, with the exception of GASPII, which reported only ever wheeze until age of 7 years. Allergic sensitisation was assessed by measuring specific Immunoglobulin E (IgE) antibodies using radio immunosorbent tests. All extracted studies used a cut-off of > 0.35 kU/L. As outcomes for allergic sensitisation we used allergic sensitisation to any allergens and in addition allergic sensitisation to aeroallergens. | |
| TRAP exposures | |
| We consider PM2.5 and NO2 as measures of traffic-related air pollution exposure. Most of the birth cohort studies applied land use regression (LUR) models to estimate long-term annual average concentrations of these pollutants to the home addresses of participants. All European birth cohorts applied the standardized LUR exposure model developed within the EU funded project ESCAPE (www.escape.eu). | |
| Inclusion criteria | |
| In this systematic review, we included studies that met the following criteria: (a) prospective birth cohort study, (b) evaluated associations between PM2.5 or NO2 exposures in early life and subsequent allergic outcomes reported at any age, (c) published in a peer-reviewed journal by the 31st of January, 2016 and (d) written in English. We did not include reviews, letters to the editor, experimental studies or human exposure studies. We did not consider non-traffic related air pollutants, such as SO2, and a few traffic-related air pollutants, such as ozone and black carbon. | |
| Data extraction | |
| Data extraction was carried out in duplicate by two reviewers (GF, JH) and synthesised according to the PRISMA and MOOSE guidelines. We recorded study name, year published, age of subjects, exposure marker, exposure level, exposure metric, outcome category and adjusted effect estimates from selected studies, as summarized in Table 1 and supplement Tables S1-S9. | |
| Table 1: Summary of available studies (× indicates that a study was included in the respective systematic review). | |
| Quality assessment | |
| The methodological quality was assessed by two researchers (JH, FG) using the Newcastle- Ottawa scale for cohort studies (accessed April 2016) [15]. A quality score was calculated based on three major categories: group selection (four items), comparability between groups (one item) and outcome assessment (three items). A maximum of one point was allocated to each item in the group selection, outcome assessment and exposure assessment categories and a maximum of two points was awarded for comparability. Therefore, the maximum possible score was nine points and represents the highest methodological quality. | |
| Meta-analysis | |
| If a series of selected studies were based on the same birth cohort study, we included only the effect estimate corresponding to the maximal follow-up period (i.e. oldest age). We conducted a metaanalysis for asthma, wheeze, allergic sensitisation and hayfever, as the number of extracted studies with similar exposures was sufficient (more than two). We performed both fixed and random effect metaanalyses to obtain combined effect estimates and 95% confidence intervals (CIs). Since overall effect estimates were very similar we only showed results for the random effects models, because these models can better include the methodological heterogeneity across the included studies. Effect estimates are shown for increments of 2 μg/m3 for PM2.5 and 10 μg/m3 for NO2. The I2 statistic was computed to illustrate the heterogeneity between studies [16]. Meta-analyses were performed using R, version 3.2.3. (Package: ‘metafor’ [17]) | |
| As sensitivity analyses we left out those cohorts of very young age from INMA and CHILD and results from the high risk cohort of CAPPS. | |
Results |
|
| Literature search | |
| For the publication period between April 2014 to January 2016, a total of 338 references were identified using the search terms. After excluding duplicates (n=88), the titles and abstracts of the remaining 250 papers were reviewed. Most papers were excluded as they did not meet our inclusion criteria (n=216; reviews, commentaries, not performed as a birth cohort study, exposure not relevant, no allergic outcomes considered). The full text of the remaining 34 studies was reviewed, and six met the inclusion criteria. These six papers were added to the 19 previously identified (using the same search strategy) by Bowatte et al. Further, we identified four additional papers that were published before March 2014 but that were missed by Bowatte and colleagues. Finally, one paper [19] that was included in Bowatte et al, but that is not related on any of the outcomes of interest, was excluded and one paper [18] that was a panel study on the short-term effects of air pollution was excluded. . Ultimately, we identified 27 eligible papers and 15 of them provided effect estimates that could be used for meta- analysis. This selection process is depicted in Figure 1. | |
| Figure 1: Study selection, The exclusion of the high risk CAPPS cohort from meta-analysis. | |
| Cohort characteristics | |
| The characteristics of the extracted papers are summarized in Table 1. Briefly, all studies were based on randomly selected subjects, except for the CAPPS cohort, which is a cohort of children with a parental history of allergic diseases. Of the 15 birth cohort studies, eight are based in Europe (Olso (Norway), BAMSE (Sweden), GINIplus (Germany), LISAplus (Germany), PIAMA (The Netherlands), INMA (Spain), GASPII (Italy), MAAS (UK)), four in Canada (SAGE, CAPPS, CHILD and BCBC), two in the US (CCAAPS and CCCEF) and one in Taiwan (TBCS). The sample size of the cohorts included in the published analyses ranged from 178 (SAGE, Canada) to 37,401 (BCBC, Canada). While most of the studies on asthma had a follow up period of approximately 10 years, the studies on wheeze tended to have a shorter follow up period. The comprehensiveness of the follow-up examinations differed across studies. | |
| The outcome prevalences differed substantially across cohorts, ranging from 4% to 10.9% for asthma, from 5% to 28.9% for wheeze, from 2.6% to 11.5% for hayfever, from 16% to 40.4% for any allergen sensitisation, from 5% to 34.9% for aeroallergen sensitisation, and from 4.9 % to 15.5% for eczema. These differences are mainly driven by the selection of high risk subjects (CAPPS) and the different follow-up durations (that is, age of the participants at the time of assessment). However, it is also highly likely that cultural and geographical differences also play a role. The average levels of the ambient air pollution concentrations also differed substantially across cohorts (see table S1-S9). On average, the vast majority of subjects were exposed to TRAP levels below the current guidelines provided by the World Health Organization, which are an annual mean exposure of 10 μg/m3 for PM2.5 and 40 μg/m3 for NO2. While most of the studies used the standardized LUR models developed by ESCAPE, some cohorts applied dispersion modeling (BAMSE and OSLO study). | |
| Quality assessment of included cohorts | |
| All 27 included studies reached at least 7 out of 9 (the highest score possible) on the Newcastle- Ottawa scale [15]. Since the health assessment is mainly based on self-reports or parental reports of respiratory diseases and symptoms, no study reached the highest score possible. A substantial loss to follow up of more than 40% of the initial recruited cohorts occurred in a few studies, especially those with long follow up durations. Since loss to follow up is not at random, the results of these studies may be affected by bias. | |
| Meta-analysis | |
| Asthma: The combined estimate from the seven studies on PM2.5 and incident asthma was elevated but not statistically significant (1.11 (95% CI 0.97, 1.26) per 2 μg/ m3 increase; Figure 2). There was some heterogeneity across the single study results. The same pattern was observed for NO2 (1.08 (95% CI 0.96, 1.20) per 10 μg/ m3, based on ten studies, Figure 3). Leaving out the high risk CAPPS study, the effect estimates attenuated to 1.03 (95% CI 0.97, 1.10) for PM2.5 and 1.06 (95% CI 0.95, 1.19) for NO2. | |
| Figure 2: Asthma and PM2.5 exposure (per 2 µg / m3 increase). | |
| Figure 3: Asthma and NO2 exposure (per 10 µg / m3 increase). | |
| Wheeze: The combined effect estimate for wheeze was elevated for PM2.5 (1.13 (95% CI 1.00, 1.28), based on four studies, Figure 4), but not statistically significant for NO2 (1.08 (95% CI 0.98, 1.18), based on nine studies, Figure 5). When leaving out the high risk CAPPS study, the effect estimates attenuated to 1.09 (95% CI 0.99, 1.20) for PM2.5 and did not change for NO2, when results from the very young children from INMA were additionally not included. | |
| Figure 4: Prevalent wheeze and PM2.5 exposure (per 2 µg / m3 increase). | |
| Figure 5: Prevalent wheeze and NO2 exposure (per 10 µg / m3 increase). | |
| Allergic sensitization: A meta-analysis was not performed for PM2.5 and allergic sensitisation as there was no new information that was not used in the meta-analysis by Gruzieva et al. [20] in 2014, which reported a non-significant positive association between PM2.5 and sensitization to any allergen. There were six studies that evaluated the effect of NO2 on sensitization to any allergen, and the combined meta-analytic result showed no association (1.00 (95% CI 0.98, 1.02) per 10 μg/m3 increment; Figure 6). When the high risk cohort CAPPS is left out, this has no impact on the overall effect estimates. For sensitization specifically to aeroallergens, a weak positive association was observed for PM2.5 (1.05 (95% CI 1.00, 1.11) per 2 μg/m3 increase, based on six studies, Figure 7), but not for NO2 (1.02 (0.92, 1.13) per 10 μg/m3 increase, based on eight studies, Figure 8). The overall effect estimate remained unchanged for PM2.5, and was slightly reduced to (1.00 (0.89, 1.13) for NO2, when CAPPS data and CHILD data was excluded from meta-analysis. | |
| Figure 6: Sensitisation to any allergen and NO2 exposure (per 10 µg / m3 increase). | |
| Figure 7: Sensitisation to aeroallergens and PM2.5 exposure (per 2 µg / m3 increase). | |
| Figure 8: Sensitisation to aeroallergens and NO2 exposure (per 10 µg / m3 increase). | |
| Hayfever: The combined effect estimate for hayfever was not significant for PM2.5 (1.02 (95% CI 0.85, 1.21) per 2 μg/m3 increase, based on five studies, Figure 9) or NO2 (1.01 (95% CI 0.85, 1.19) per 10 μg/m3 increase, based on six studies, Figure 10). The exclusion of the high risk CAPPS cohort from meta-analysis lead to almost unchanged effect estimates of (1.02 (95% CI 0.83, 1.24) for PM2.5 and (1.00 (95% CI 0.82, 1.22) for NO2. | |
| Figure 9: Hayfever and PM2.5 exposure (per 2 µg / m3 increase). | |
| Figure 10: Hayfever and NO2 exposure (per 10 µg /m3 increase). | |
| Eczema: A meta-analysis was not possible for eczema, as only three very heterogeneous studies exist [21,22,23]. These studies report associations for different ambient air pollutants (PM2.5, NO2, and PM10) on eczema assessed at different ages (six months, six years, and eight years). | |
Discussion |
|
| This review summarizes the most recent state of the art birth cohort studies on early life TRAP exposure and asthma and allergic health outcomes in childhood and adolescence. It includes numerous large, long-term studies that were only very recently published and for nearly all outcomes considered, a sufficient number of studies existed to allow a meta-analysis to be conducted. This was not the case in previous work, such as that by Bowatte et al. [11]. However, despite this wealth of information, which includes over 50 years of research, it appears that the “jury is still out” as to whether traffic-related air pollution causes asthma and other allergic health outcomes. The meta-analytic effect estimates between PM2.5 and NO2 with asthma, wheeze and allergen sensitization tended to be elevated but failed to reach statistical significance. For hay fever, no increased risk was observed, which is consistent with the single published meta-analysis of European studies by Gehring et al. [24], which also included all studies considered here except one Canadian study. The three existing eczema studies vary substantially in terms of methodology and therefore could not be combined [21,22,23]. | |
| Despite the mostly inconclusive evidence from epidemiological studies, the existence of a possible association is rather strongly supported by the results of laboratory studies and human exposure experiments, which are comprehensively summarized in three major reports [1,3,7]. The evidence from experimental studies for the adverse effects of particulate matter, in particular fine particles, is especially strong, whereas the support for an adverse role of NO2 is weaker, possibly due to a lower number of existing investigations. In observational studies, NO2 is mainly used as a proxy for a mixture of air pollutants originating from traffic exhaust whereas PM2.5 is used as a surrogate of combustion emissions originating from traffic, industry and home heating. | |
| Overall, this review did not show any statistically significant association between asthma and NO2 or PM2.5, albeit the combined effect estimates are above 1. Thus, this more comprehensive review, which includes data from more birth cohorts and with longer followup durations, does not support Bowatte’s conclusion of a major role of TRAP on asthma. Apart from this different conclusion and the methodological heterogeneity across the cohorts our systematic review provides some support of the notion by Bowattee et al. [11] that the magnitude of the association between early childhood exposures to PM2.5 might increase with age. Our more conservative null asthma findings are however in-line with those of a previous meta-analysis of European birth cohort data by Molter et al. [25] which included data from almost the same studies as our review, but with shorter follow ups. The only study published on asthma beyond the search data used in Bowatte et al. [11] was on the Dutch PIAMA birth cohort. A statistically significant association between asthma and TRAP markers was reported [26]. The PIAMA study is large and contributes substantially elevated risk estimates to the overall combined results (Figures 2 and 3). The reason for the large heterogeneity in asthma associations across birth cohorts is unclear. At least for the European birth cohorts, which make up the majority of the included studies, a standardized exposure assessment methodology was applied (see www.escape.org) and the questions used to assess the existence of health outcomes is very similar. However, it is not known whether same clinical criteria for an asthma diagnosis by the general practitioner have been used across the European studies and whether these diagnostic procedures have changed over time. Different sources of air pollution might be one possible explanation. Another could be the different, levels of TRAP across cohorts, however this latter explanation is unsatisfactory as cohorts with similar average levels of TRAP still show different associations. Moreover, the degree of urbanization and the mixture between urban and rural areas differ across cohorts and may play a role. Finally unmeasured confounding by socioeconomic factors, second-hand smoking and allergic predispositions cannot be ruled out. As wheeze is a key symptom of asthma, it is not surprising that the results of these two outcomes are similar. However, when present in early life, it can also be a proxy for a mixture of respiratory problems caused by viral or bacterial infections, and it is thus important to consider this outcome as a separate entity. | |
| No meaningful effects were found for allergic sensitization (any allergen or restricted to aeroallergens) in the current meta-analysis, which is in line with the previous pooled analysis by Gruzieva et al. [20], which included many of the same studies. | |
| Further, the only existing meta-analysis for hayfever did not show any statistically significant increased risk for NO2 [24], congruent with the results of the current work. It is important to note that the overlap between the cohort studies included in these two works is high. Nonetheless, several single cohort analyses on hayfever with shorter follow up durations also reported null associations (up to eight years in PIAMA [23] and up to 10 years in GINI-LISA [27]). No additional studies on PM2.5 using birth cohort data were published beyond the meta-analysis by Gehring et al. [24] which found no association with PM2.5 | |
| Thus, so far, there appears to be only very weak evidence supporting an association between TRAP and hay fever and allergic sensitization. | |
| Associations between TRAP exposure and eczema were only considered in three papers, all of which did not report statistically significant increased risks [21-23]. These studies are too heterogeneous and too few for a meta-analysis and consequently, to draw any firm conclusions. Nonetheless, one could cautiously conclude that observational study results from birth cohorts to date do not support the notion of an adverse effect of TRAP on eczema onset. | |
| Asthma and other allergic conditions are complex diseases with multi factorial aetiologies, which are influenced by environmental and life-style factors as well as genetic make-up [28]. The list of environmental factors and co-exposures considered in each of the individual studies included in this review differed by cohort. Thus, it is not entirely surprising that the association between TRAP and the studied outcomes is not homogeneous and straightforward. Future studies might include epigenetic factors, which may shed more light on the role of TRAP exposure on the development of asthma and allergic disorders. | |
Strengths and Limitations |
|
| that justify their use in the investigation of long-term TRAP effects (particularly in early life) on respiratory health, they are not without limitations. Cohort studies tend to have lower participation rates at recruitment compared to cross-sectional studies and loss to follow up is higher among participants with lower socio-economic status [29]. If subjects who are not recruited or who drop out sooner have higher TRAP exposures, as was shown by Brauer et al. [30], this might lead to an underestimation of the risk [31]. Our decision to limit our review and meta-analysis to birth cohort studies could perhaps thus be seen as a limitation for these reasons, and also, because studies that recruit subjects years after birth and follow them up throughout life are also informative, despite not being able to consider perinatal exposures. Nonetheless, as it is widely accepted that exposures that occur during the perinatal period have an important influence on respiratory health [32]. We thus believe that the strengths associated with using only birth cohort data outweigh the limitations. | |
Conclusions |
|
| Despite the comprehensiveness of our approach and decision to focus only on high quality birth cohort data, this systematic review and meta-analysis provides only weak support for the existence of a causal role of PM2.5 and NO2 exposure in early life on asthma and wheeze during childhood and early adolescence. Combined effect estimates from existing birth cohort studies do not support a causal role of PM2.5 and NO2 exposure on hayfever and allergic sensitization. | |
Authors’ Contributions |
|
| JH initiated this review, developed the methodology, evaluated the identified papers for full-text review, and drafted the manuscript. FG did the primary literature search, reviewed title and abstract of extracted references and performed the meta-analysis. All authors contributed to interpretation, discussion and revision of the manuscript. All authors approved the final version of this manuscript for submission agreed to be accountable for all aspects of the work. | |
Acknowledgments |
|
| We thank Dr. Olena Gruzieva, Stockholm, Dr. Elaina MacIntyre, Toronto, and Dr. Ulrike Gehring, Utrecht, for providing cohort-specific effect estimates for their evaluated associations between TRAP with asthma and allergic conditions. | |
Role of the Funding Source |
|
| This review is not funded by a third party. | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi