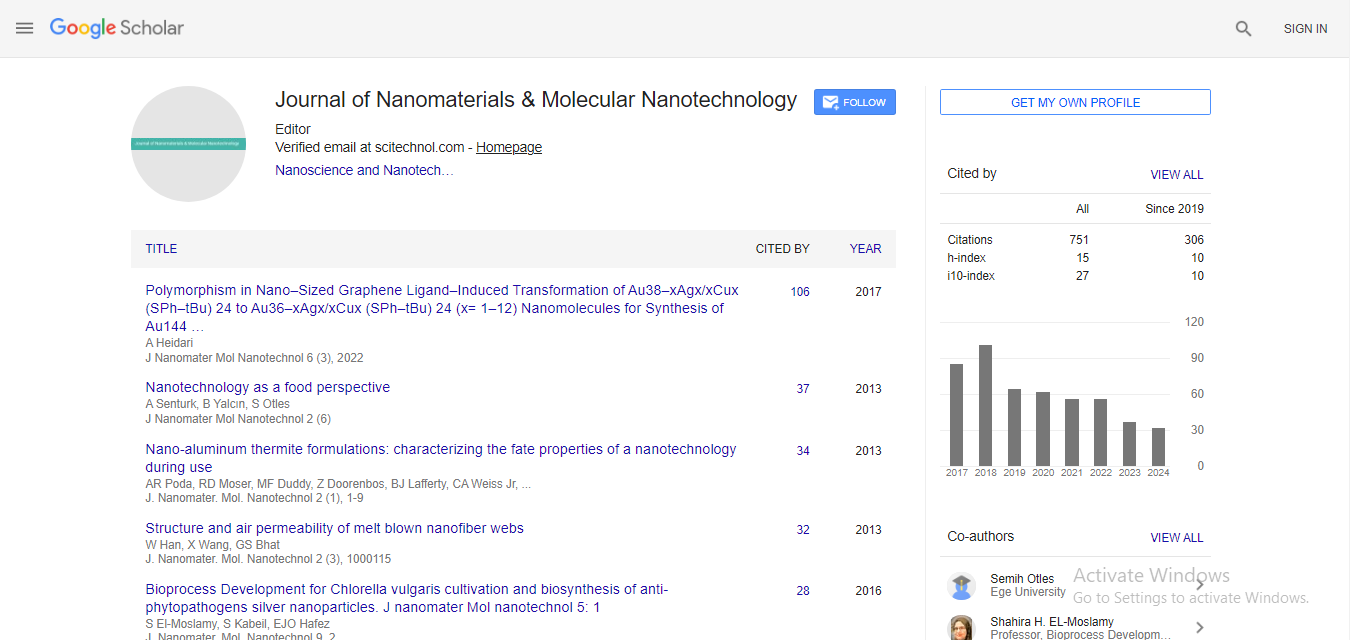
Editorial, J Nanomater Mol Nanotechnol S Vol: 0 Issue: 2
Broader Aspects of Nanopharmaceutical Safety: Need for an Integrated Approach
| S. M. Moghimi1,2*, Z. S. Farhangrazi3 | |
| 1Centre for Pharmaceutical Nanotechnology and Nanotoxicology, Department of Pharmacy, Faculty of Health and Medical Sciences, University of Copenhagen, Universitetsparken 5, DK-2100 Copenhagen, Denmark | |
| 2NanoScience Centre, Faculty of Science, University of Copenhagen,Universitetsparken 5, DK-2100 Copenhagen, Denmark | |
| 3Biotrends International, Denver Technological Center, Greenwood Village,Colorado, USA | |
| Corresponding author : Prof. SM Moghimi Centre for Pharmaceutical Nanotechnology and Nanotoxicology, Department of Pharmacy, Faculty of Health and Medical Sciences, University of Copenhagen, Universitetsparken 5, DK-2100 Copenhagen, Denmark Tel: +35 35336528 E-mail: moien.moghimi@sund.ku.dk |
|
| Received: April 09, 2014 Accepted: April 14, 2014 Published: April 16, 2014 | |
| Citation: Moghimi SM, Farhangrazi ZS (2014) Broader Aspects of Nanopharmaceutical Safety: Need for an Integrated Approach. J Nanomater Mol Nanotechnol S2:e001. doi:10.4172/2324-8777.S2-e001 |
Abstract
Broader Aspects of Nanopharmaceutical Safety: Need for an Integrated Approach
Nanoparticulate drug carriers and multifunctional nanoparticles are beginning to provide a range of unique therapeutic and diagnostic opportunities. However, there is an increasing concern regarding nanoparticle safety for human use, but these are not often viewed within the context of clinical dosing, administration route, and pathological conditions in question. A complex array of interrelated physicochemical and biological factors control nanoparticle pharmacokinetics, site-specific targeting, therapeutic efficacy and safety, and these have been reviewed recently. From a clinical perspective, it is imperative to identify and translate realistic opportunities offered by understanding of pathophysiological processes to the design and engineering of efficient and safe nanopharmaceuticals. Such strategies will most likely enhance benefit-to-risk ratio, as opposed to empirical approaches that tend to find forced biomedical applications for a broad range of emerging nanomaterials, which eventually contributes to increased toxicity concerns.
| Nanoparticulate drug carriers and multifunctional nanoparticles are beginning to provide a range of unique therapeutic and diagnostic opportunities [1,2]. However, there is an increasing concern regarding nanoparticle safety for human use, but these are not often viewed within the context of clinical dosing, administration route, and pathological conditions in question. A complex array of interrelated physicochemical and biological factors control nanoparticle pharmacokinetics, site-specific targeting, therapeutic efficacy and safety, and these have been reviewed recently [2]. From a clinical perspective, it is imperative to identify and translate realistic opportunities offered by understanding of pathophysiological processes to the design and engineering of efficient and safe nanopharmaceuticals. Such strategies will most likely enhance benefit-to-risk ratio, as opposed to empirical approaches that tend to find forced biomedical applications for a broad range of emerging nanomaterials, which eventually contributes to increased toxicity concerns [2,3]. | |
| For the most pharmaceutically viable and promising nanoformulations, we still need to establish the interdependency of nanoparticle size, shape, and surface characteristics to interfacial forces, controlled drug release, metabolism and excretion of particulate components, pathology and possible adverse effect [2,3]. However, in many pre-clinical studies realistic dosing with nanoparticles in relation to disease type, stage and progression is often ignored, which inadvertently contributes to adverse effects. We may not be able to eliminate materials’ toxicity fully, but can increase their performance to an extent that may outweigh adverse effects and, hence, clinically justifiable for use/or to use. For instance, for some patients, certain degree of toxicity is acceptable, since there may be no alternative or other effective therapeutic approaches to prolong life. Regardless, the chosen material must be pharmaceutically acceptable and manageable. | |
| Precision characterization of nanopharmaceuticals and multifunctional nanocarriers is still a challenging issue [2,3]. Poor characterization may translate to increased toxicity, failed trials and withdrawals. Today, the complex nature of many engineered nanoparticles/nano carriers makes such studies cumbersome and difficult, but this may be overcome by improving and investing in characterization tools, and introducing methodologies that generate precisely defined nanoparticles, particularly with respect to surface properties and surface domains [2,4]. Indeed, on introduction into the body many nanoparticles will be challenged and intercepted by the immune system [1,2]. Throughout the evolution, the immune system has developed sophisticated sensing strategies that can recognize and eliminate foreign objects safely (even the so-called ‘stealth’ materials). The immune system rarely discriminates between size and shape, but rather senses surface characteristics elegantly. Our own efforts have addressed these issues in relation to phagocytic clearance (including different macrophage sub-populations) and nanoparticle-mediated complement activation [5–9]. The complement system is a key effector of both innate and cognate immunity, and is responsible for rapid detection and elimination of particulate intruders in nano- and micro-size ranges [6,8]. Complement triggering primes the intruders’ surface for rapid recognition and clearance by phagocytic cells [6,8]. It also induces inflammatory responses, but responses arising from uncontrolled complement activation could be life threatening [6,7]. Complement recognizes danger signals primarily through pattern recognition. This is of prime concern in the design and engineering of nanomedicine as these entities are often composed of polymeric components and other patterned nanostructures [6]. There is compelling evidence that complement activation may be a contributing factor in eliciting acute-like reactions to regulatoryapproved particulate and polymeric medicines (including stealth entities) in many individuals [6,7]. Accordingly, we have addressed mechanistic issues pertaining to these responses in relation to stealth nanomedicine (liposomal and polymeric nanospheres), thermoresponsive gels, micellar systems, carbon nanotubes, graphene oxide, and other related entities of interest to healthcare, and in some cases have introduced measures to by-pass complement triggering [5–11]. Our recent efforts have further attested to the possible role of intratumoral nanoparticle-mediated complement activation in promoting tumor growth, and hence a need for radical thinking in relation to the development of safer anti-cancer nanomedicine [12]. | |
| With the advent of material science and nanoparticle engineering, many are revisiting the protein adsorption phenomenon, but interpretations are rather over stated, irrelevant, and not analysed within the broader context of dynamic pathophysiological processes and the systems immunology [13]. Accordingly, immune toxicity issues are often missed or under estimated, and outside the scope of systems immunology and broader disease context. Likewise, many do not consider the molecular aspects of nanomaterial toxicity in relation to dynamic integrative cellular responses and the kinetics of the cell-death dimension [14–16]. Again attempts are usually empirical and restricted to a simple yes or no cell death response. A clear lack of molecular understanding and profiling may translate to lost opportunities in terms of better design and optimization strategies. However, it is the dynamic dimension of cell-stress responses as well as cellular heterogeneity within a typical population that makes realization of global safety protocols very difficult. Indeed, each case (formulation) must be considered separately and within the scope of benefit-to risk ratio, and the clinical condition in question, but forced extrapolation must be avoided. | |
| Finally, we must improve on animal models representing human diseases. This is a serious shortfall, since we rarely have preclinical models that can provide better insights to therapeutic responses and be of high value to translational phases. One example is cancer, where massive investments have been made for development of anticancer nanomedicine [17,18]. Unfortunately, the majority of these developments have led to disappointing therapeutic efficacy and incremental clinical success [19,20]. Realistically, the animal models have not been good enough. For instance, mouse tumor xenograft models have routinely been employed, and often based on monogenic human tumor cell lines. These cell lines bear little resemblance to primary cancers, and furthermore tumor progression is rapid, often few days in mice compared with periods of years in humans. Another prominent difference is the tumor stroma and its cell and matrix constituents, which is of murine, and not human, origin. Least but not last, the inbred mice models lack human immune system. Therefore, it is not surprising that the observed therapeutic responses in mice, which are often hyped and unrealistic, show little resemblance to clinical conditions. We must build on these deficiencies and introduce viable and validated models of the human disease in order to help the translational phase. | |
| The influence of political and market forces as well as financial outcomes, and emerging buzz-words (such as ‘personalized and translational nanomedicine’) should not be the key driving force for development of human nanopharmaceuticals. Future plans and investment in nanopharmaceuticals should take the above mentioned concerns into consideration, and call for a paradigm shift in approach and design of future therapeutic strategies based on improved characterization technologies, systems biology, realistic opportunities offered by the human disease states and validated models representing human pathologies. | |
Acknowledgment |
|
| SMM acknowledges financial support by the Danish Agency for Science, Technology and Innovation, references 09-065736 (Det Strategiske Forskningsråd), and 12-126893 (Technology and Production). | |
| Authors declare no competing financial interests. | |
References |
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi