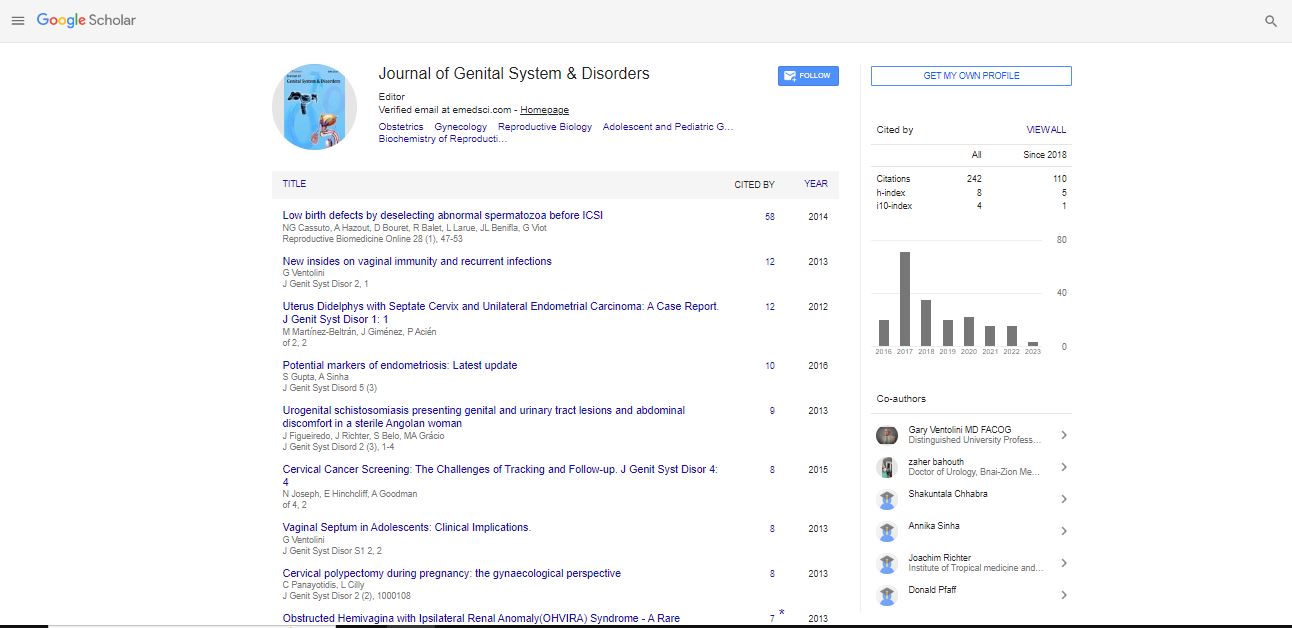
Editorial, J Genit Syst Disor S Vol: 0 Issue: 1
The Fascinating World of Androgen Insensitivity Syndromes
| Lawrence S Amesse1,2* | |
| 1Section of Pediatric-Adolescent Gynecology, Division of Reproductive Endocrinology and Infertility, Department of Obstetrics Gynecology, Wright State University Boonshoft School of Medicine, Dayton, Ohio, USA | |
| 2Department of Pediatrics, Wright State University Boonshoft School of Medicine, Dayton, Ohio, USA | |
| Corresponding author : Lawrence S Amesse Berry Women’s Pavilion, Suite 4130, Miami Valley Hospital, One Wyoming Street, Dayton, Ohio 45409-2793, USA Tel: (937) 208-6810; Fax: (937) 208-3359 E-mail: lsamesse@gmail.com |
|
| Received: March 07, 2013 Accepted: March 08, 2013 Published: March 15, 2013 | |
| Citation: Amesse LS (2013) The Fascinating World of Androgen Insensitivity Syndromes. J Genit Syst Disor S1. doi:10.4172/2325-9728.S1-e001 |
Abstract
The Fascinating World of Androgen Insensitivity Syndromes
The androgen insensitivity syndromes (AIS) comprise a fascinating group of X-linked recessive disorders of sex development (DSD), known collectively as 46 XY DSD. Since their identification as “testicular feminization syndrome” in 1953 by Dr. John Morris at Yale, significant technological advancements and refinements have heightened our understanding of the underlying molecular mechanisms that in part delineate the role of impaired of androgen responsiveness on the developing male fetus.
Keywords: Androgen Insensitivity Syndrome; X-linked recessive disorders
| The androgen insensitivity syndromes (AIS) comprise a fascinating group of X-linked recessive disorders of sex development (DSD), known collectively as 46 XY DSD. Since their identification as “testicular feminization syndrome” in 1953 by Dr. John Morris at Yale, significant technological advancements and refinements have heightened our understanding of the underlying molecular mechanisms that in part delineate the role of impaired of androgen responsiveness on the developing male fetus [1]. These advancements and refinements have also lead to a better understanding of the secondary sexual characteristics manifested during pubertal transition of young males affected with the disorder. Females (46 XX) with a mutation in one androgen receptor (AR) gene will be minimally affected and since they are carriers they should receive genetic counseling. | |
| The heterogenetic phenotypic manifestations of AIS reflect the AR status. Individuals with AIS may manifest variable phenotypic expressions while having in common a similar pathophysiology and androgen insensitivity consequent to similar mutations in the AR gene, suggesting differences in expressivity, even among families. The eight-exon AR gene, a member of the nuclear receptor superfamily, is located on Xq11-12. Over 800 different AR mutations have been identified, including complete and partial gene deletions, point mutations and small insertions and deletions [2]. Although many of these mutations are inherited from one generation to the next, 30% of all AIS cases are de novo mutations, i.e., germ line, germ cell mosaicism, fertilized egg or post-zygote stage, and this represents an area of potential research [3,4]. There are also cases of AIS that do not have mutations of the AR gene and this is another fertile area for future research. | |
| The AIS are categorized into 3 groups according to residual AR function: complete androgen insensitivity syndrome (CAIS), incomplete androgen insensitivity syndrome (IAIS) and mild androgen insensitivity syndrome (MAIS). Individuals with CAIS appear as phenotypic females yet express the XY karyotype. The most common presentation is primary amenorrhea. Breast development is normal and may be enhanced by unopposed estrogen in the absence of androgens. Axillary and pubic hair is absent to scant. Complete AIS may also present during infancy with inguinal or labial swelling due to a testis in an otherwise phenotypic female. The gonads are testes independent of phenotype owing to the presence of the Y-chromosome [5]. | |
| The Wolffian duct derived structures fail to develop in the AIS even in the presence of adequate testosterone owing to variable degrees of AR function. At the same time, the testes generate normal antimüllerian hormone levels that suppress müllerian duct development, although uterine vestiges may be evident [2]. The external genitalia are female, and the labia and clitoris are marginally underdeveloped. Vaginal development will vary; often it is absent or a short pouch is evident. The differential diagnosis of CAIS in adolescents includes XY complete gonadal dysgenesis or Swyer syndrome. In infancy, the 17β-hydroxy steroid dehydrogenase (17β-HSD) deficiency should be considered, as it will result in decreased serum testosterone concentrations necessary for development of Wolffian duct derived structures. | |
| Incomplete androgen insensitivity syndrome (IAIS) is characterized by incomplete masculinization of the external genitalia consequent to partial androgen responsiveness. These patients typically have ambiguous genitalia at birth with variable degrees of Wolffian structures evident. The characteristic phenotype includes perineoscrotal hypospadias, micro-penis and a bifid scrotum. The bifid scrotum may contain testes, but often are undescended and remain intra-abdominal. Other manifestations can occur, with the most severe characterized by isolated clitoromegaly or in the milder forms, isolated hypospadias. The external genitalia can also mimic those associated with the CAIS. | |
| Other under virilization conditions must be considered in the differential diagnosis of PAIS. Potential etiologies include partial gonadal dysgenesis, LH receptor mutations, 17, 20-lyase deficiency, 17 β-HSD and 5-α reductase deficiencies as well as syndromic disorders such as Klienfelter and Smith-Lemli-Opitz. | |
| Mild androgen insensitivity syndrome (MAIS) represents the opposite end of the AIS continuum. It currently represents an underexplored area full of potential for new discoveries. MAIS has been identified in a small subset of men with male factor infertility characterized by oligospermia or azoospermia, normal serum testosterone levels and elevated LH concentrations. Genetic studies have demonstrated a defect of the androgen receptor gene [6]. These men have normal male external genitalia and a male gender orientation [7]. | |
| Diagnosis of AIS can be challenging in infancy. Female infants with inguinal hernias should undergo fluorescence in situ hybridization (FISH) or karyotype studies for the presence of a Y chromosome to help confirm the CAIS diagnosis. In the pubertal patient with CAIS, serum LH and testosterone levels are at or above normal male ranges. Serum estradiol is increased in these patients consequent to direct hormone contributions from the testes as well as peripheral conversion of excess testosterone. Serum FSH concentrations are normal to slightly elevated. Resistance to androgenic and metabolic effects of testosterone is evident [8]. In utero screening tests for congenital malformations may reveal a karyotype-ultrasound gender mismatch suggestive of the disorder. | |
| The definitive diagnosis of AIS often requires both genetic and biochemical studies. Gene sequencing of the AR gene will identify an abnormal AR in most cases. In vitro functional assays that measure AR binding in fibroblasts obtained from scrotal, foreskin or labial tissue will be absent in CAIS or reduced in IAIS and will assist in confirming the disorder. Diagnostic testing that detects MAIS is limited and this area represents a promising new area in developing diagnostic testing. Ultrasound can be useful in identifying the presence of vestigial müllerian structures. | |
| Management involves a multidisciplinary approach. The approach is aimed at treating the symptomatology as well as addressing gender assignment and sex of rearing. Clinical considerations, such as hormone replacement therapy, as well as surgical treatments and their proper timing, i.e., inguinal heriniorraphy, genitoplasty, gonadectomy, should be addressed. Careful consideration regarding the risk of tumor development as well as genetic and psychosocial counseling are essential components of proper management strategies that enhance wellbeing and improve quality of life parameters. | |
| Androgen Insensitivity Syndromes challenge the clinician at multiple levels. Sex of rearing in CAIS is female and indicates the important role of androgens in brain development and sexual orientation, independent of chromosomal karyotype. More difficult is the IAIS when it is not always clear which gender should be assigned. The general consensus is that majority be assigned the male gender and sex of rearing, although cases should be considered on an individual basis until guidelines have been established. | |
| Significant effort has been placed in mapping the location of AR mutations and this will continue to be an emerging area of research, particularly with the MAIS where precious little is known. The marked phenotypic heterogeneity observed for an identical mutation suggests other confounding factors influence phenotype expression and clearly this is an area for additional investigations. | |
| Gonadal removal can be problematic for the clinician and represents an ongoing controversial issue. In some cases, the gonads are intra-abdominal, while in other cases they are located in either the inguinal canal or labial area. Gonad location will often determine what specialist will be performing the procedure. Most obstetricians and gynecologists will be comfortable removing intra-abdominal gonads, while surgeons may be more adept at removing inguinal canal structures. In CAIS, the general recommendation is to time gonad removal after the patient has transitioned through puberty even though there is a small albeit measurable risk of gonad malignant transformation. It has been postulated that gonadal androgens facilitate a fluent pubertal transition. However, the definitive role of androgens in the pubertal transition has not been fully explored. That stated, androgens are converted to estrogens that are involved in breast development, the female habitus and bone maturation. After the gonadectomy, the type and amount of hormonal supplementation still remains controversial and is another area of advancing research. | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi