Case Report, Dent Health Curr Res Vol: 3 Issue: 2
Evaluation of Coagulation and Healing Effect of Laser and Hemostatic Sponge on Post Extraction Dental Socket for a Diabetic: A Case Report
Al-Wardi NA*, Al-Maliky MA and Mahmood AS
Department of Biomedical Applications, Institute of Laser for Postgraduate Studies, University of Baghdad, Baghdad, Iraq
*Corresponding Author : Noor A Al-Wardi
Department of Biomedical Applications, Institute of Laser for Postgraduate Studies, University of Baghdad, Baghdad, Iraq
Tel: 009647812793745
E-mail: noor198250@yahoo.com
Received: August 17, 2017 Accepted: August 29, 2017 Published: September 03, 2017
Citation: Al-Wardi NA, Al-Maliky MA, Mahmood AS (2017) Evaluation of Coagulation and Healing Effect of Laser and Hemostatic Sponge on Post Extraction Dental Socket for a Diabetic: A Case Report. Dent Health Curr Res 3:2. doi: 10.4172/2470-0886.1000130
Abstract
Complications after dental extraction for diabetics are common, this work was made to compare between hemostatic and healing effects of 940 nm diode laser and hemostatic sponge on the dental alveolus in a diabetes patient. We report an instance of 50 years of age diabetic female with history of post extraction entanglements (draining and swelling) went to dental center for various extractions, at that point diode laser and hemostatic wipe were utilized to quit dying. Results showed that 940 nm diode laser was better than hemostatic sponge in coagulation and healing of the extraction area.
Keywords: Bleeding; Diabetics; Diode laser; Extractions; Healing effects; Hemostatic sponge; Swelling
Introduction
Diabetes mellitus is a systemic disease that characterized by elevation in blood glucose level due to insulin reduction or resistance this lead to defect in the metabolism of proteins, carbohydrates and fats this defect lead to acute and chronic complications [1].
Diabetes indications reach out to the oral pit and cause numerous issues including: periodontal ailments, salivary disfunction, ailments of oral mucosa, oral contagious diseases, taste adjustment, neurosensory disarranges, and increment the weakness of dental caries, lacquer hypoplasia and tooth affectability [2,3].
Diabetic patients need special care during dental procedures, morning appointments are preferable and patient must be instructed to have breakfast before attending the clinic to avoid hypoglycemia which occurred mainly in fasting diabetes patients [4]. Post dental extraction complications are more common in diabetics than in nondiabetic patients, swelling, discomfort, prolong bleeding, infections and dry socket can be seen in high percentage of diabetes teeth extraction sites [5].
Healing of the extraction wound can be affected by diabetes, immunity diminution of those patients causes delayed or defected wounds healing [6,7]. Many methods are applied to fastening clot formation and wound healing after teeth extraction, hemostatic colloidal silver gelatin sponge is used to control post extraction bleeding by stimulating clotting process, also colloid silver works as an antibacterial agent due to its ability to kill many species of antibiotic resisted oral bacteria when it inserts in the dental socket [8,9].
Diode lasers are used in dentistry soft tissue procedures they are used to coagulate deep portions of oral mucosa due to their absorption by hemoglobin, their antibacterial effects reduce the number of bacteria in the mouth [10,11].
Case Report
A 50 year-old female patient has been referred to our clinic for dental complaints. Patient’s medical history revealed diabetes mellitus type 2 which was diagnosed 13 years ago Clinical examination revealed multiple carious teeth and retained roots.
The patient was complaining from dull pain in the mandibular central incisors and left canine, and a sharp pain in the maxillary left 2nd premolar.
Pervious conventional dental extractions of the patient were followed by bleeding and swelling in the extraction area, therefore, treatment plane was to apply 940 nm diode laser in continuous mode and dose of 103.44 J/cm2 by using Epic 10 diode laser 940 nm (Biolase, USA) device with a tip (Biolase E3-7) 7 mm in length and 300 μ in diameter on the dental alveolus of incisors and 2nd premolar, and the use of hemostatic colloidal silver gelatin sponge (Roeko Gelatamp, Coltène /Whaledent Inc. Germany) on the canine dental alveolus. Before extraction some investigations were done which included: random blood sugar (RBS) = 180 mg/ dl, Hemoglobin A1C test = 9.30%, bleeding time = 90 s, clotting time = 210 s, hemoglobin level = 13.30 mg/dl and Packed Cell Volume (PCV) = 41. The patient is using Glibenclamide 5 mg as an anti-diabetic medication since 5 years, blood sample of 0.5 cc in volume was taken from the patient before teeth extraction and temperature changes of the sample after laser application was measured at 4 and 13 mm deep to the sample surface, by the use of digital thermometer (AMPROBE TMD®-56, Everett, WA, USA), to ensure the safety of the selected laser dose.
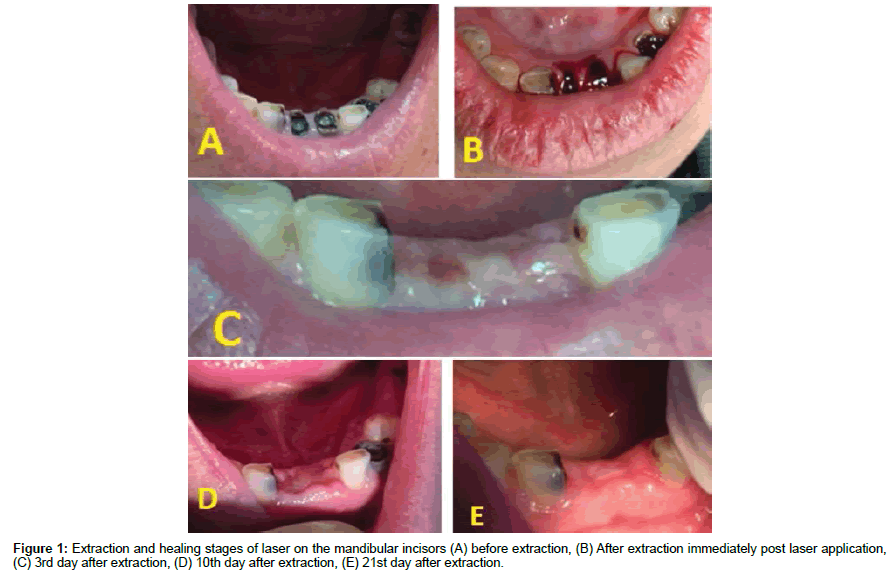
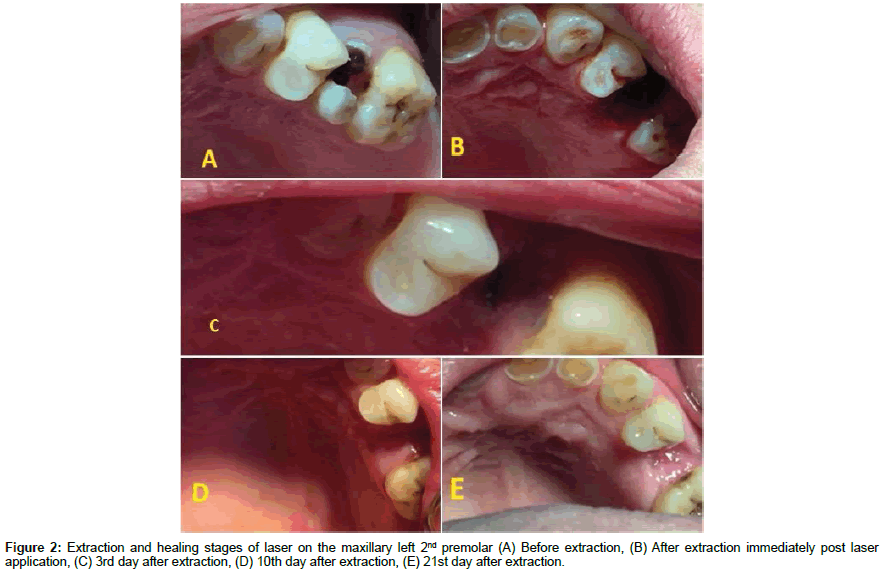
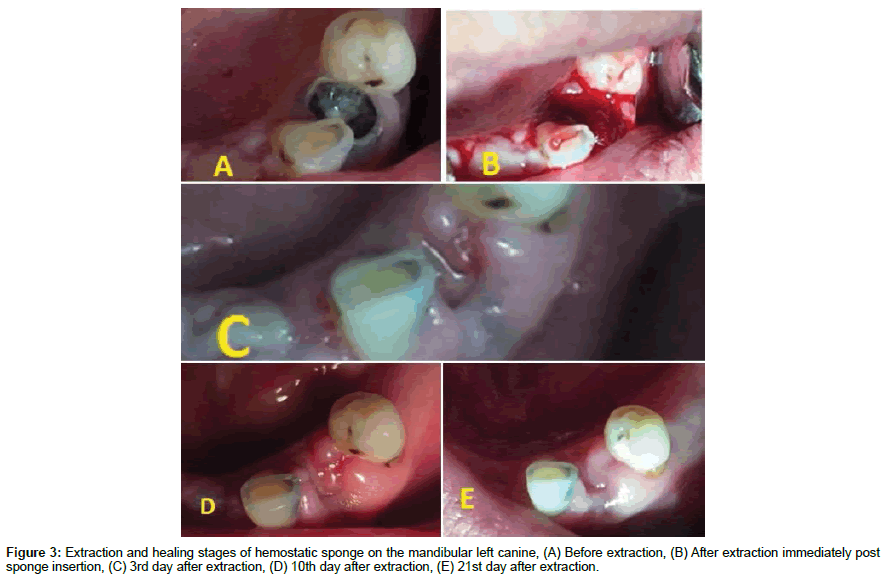
1st teeth to be extracted were the mandibular incisors extraction was done for the both of the incisors at the same appointment Figures 1(a)-1(b) then diode laser with a dose of 103.44 J/cm² was immediately applied after extraction to coagulate the socket blood, 2 weeks later maxillary left 2nd premolar was extracted Figures 2(a)-2(b) and the same dose of laser was used for coagulation. After two weeks of premolar extraction, mandibular left canine was extracted (Figures 3(a)-3(b)) and a gelatin sponge was inserted in the dental alveolus. Patients follow up in 3, 10 and 21 days after each extraction to examine the healing process of the extraction wounds. Coagulation effect of diode laser after teeth extraction was faster than that of the hemostatic sponge; wounds needed 10 s to be coagulated by laser, while few minutes were needed to the sponge to stop bleeding.
On 3rd and 10th days, inflammatory reactions (redness and swelling) were obvious in the canine extraction site while they were relatively absent in incisors and premolar extraction sites.
On day 21st, laser coagulated extraction wounds were closed, no inflammation was seen, while the wound that coagulated by the sponge still unclosed and relatively inflamed.
Discussions
Lasers have many benefits in oral soft tissue applications such as sterilization, reduction of bacteremia, post- operative pain, edema, scar and wound contraction, also they are very good hemostatic agents [12]. Temperature measurement before teeth extraction showed that the mean temperature elevation was 1.55°C at depth of 4 mm and the mean at 13 mm depth was 1.23°C, which were much lower than the critical temperature of periodontal damage.
The elevation of socket temperature by 10°C for one minute causes irreversible destruction of the periodontium in that area [13]. Laser coagulated the socket blood faster than hemostatic sponge did, in both cases laser and hemostatic sponge assisted coagulation, clot was stable, no dry socket occurred, but the healing results of diode laser were better than that of the hemostatic sponge, no swelling, faster wound healing and closer of the dental alveolus which exposed to laser, as shown in figures below.
Figure 1 showed extraction and healing stages of laser on the mandibular incisors. Figure 2 showed extraction and healing stages of laser on the maxillary left 2nd premolar. Figure 3 showed extraction and healing stages of hemostatic sponge on the mandibular left canine.
Conclusions
The comparison between 940 nm diode laser and hemostatic colloidal silver gelatin sponge revealed that, diode laser produced faster coagulation and better healing without any thermal damage of the surrounding tissues.
Acknowledgement
We confirm that we have no conflict of interest, also we confirm that all patients are agree to publish their teeth extraction and the stages of follow up photos in your journal.
References
- Wilson M, Fitzpatric J, Mc Ardle N, Stassen L (2010) Diabetes mellitus and its relevance to practice of dentistry. J The Irish Dental Association 56: 128.
- Thayumanavan B, Jeyanthikumari T, Vani NV (2015) Diabetes and oral health- an overview of clinical cases. International Journal of Medical and Dental Sciences 4: 901- 903.
- Matthews D (2002) The relationship between diabetes and the periodontal diseases. J Canadian Dental Association 68: 162.
- Alamo S, Soriano Y, Perez M (2011) Dental consideration for the patient with diabetes.J Clin Exp Dent 3: e27.
- Karbassi M, Saleh R, Kheirollahi K, Targhi M, Sadarbad M, et al. (2015) The relationship between socket blood sugar and post-extraction complications in type II diabetic and non-diabetic patients. Iranian Journal of Diabetes and Obesity 7: 13.
- Al-Obaidi M, Al-Bayaty F, Al Batran R, Hussaini J, Khor G (2014) Impact of Ellagic acid in bone formation after tooth extraction: an experimental study on diabetic rats. The Scientific World Journal 908098: 1.
- Lan C, Wu C, Huang S, Wu I, Chen G (2013) High-glucose environment enhanced oxidative stress and increased interleukin-8 secretion from keratinocytes new insights into impaired diabetic wound healing. J Diabetes 62: 2530.
- Maani S, Saleh M, Melek L, Sadaka M (2015) Evaluation of colloidal silver gelatin sponge (gelatamp) in patients receiving anticoagulant after tooth extraction (clinical study). Alexandria Dental Journal 40: 101-102.
- Yang W, Ouyang X (2015) Radiographic and clinical outcomes of ridge augmentation in molar extraction socket with sever bone wall defect. The Chinese Journal of Dental Research 18: 222.
- Azma E, Safavi N (2013) Diode laser application in soft tissue oral surgery. J Lasers in Medical Sciences 4: 206.
- Licht F (2014) Diode laser treatment as an alternative to antibiotic premedication. European Scientific Journal 10: 4.
- Amid R, Kadkhodazadeh M, Ardakani M, Hemmatzadeh S, Refoua S (2012) Using diode laser for soft tissue incision of oral cavity. J Lasers in Medical Sciences 3: 37.
- Ribeiro A, Nogueira G, Antoniazz J, Moritiz A, Zezell D (2007) Effects of diode laser (810 nm) irradiation on root canal walls: thermographic and morphological studies. J Endodontics 33: 252.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi