Research Article, J Clin Nutr Metab Vol: 1 Issue: 1
Monitoring of Nutrition Intake in Hospitalized Patients: Can We Rely on the Feasible Monitoring Systems?
Holst M*, Ofei KT, Skadhauge LB, Rasmussen HH and Beermann T
Centre for Nutrition and Bowel Disease, Department of Gastroenterology, Aalborg University Hospital, Aalborg, Denmark
*Corresponding Author : Mette Holst
Centre for Nutrition and Bowel Disease, Department of Medical Gastroenterology, Aalborg Hospital, Aarhus University Hospital, Moelleparkvej 4, Reception 3, 9000 Aalborg, Denmark
Tel: +45 27113236
Fax: +45 99326107
E-mail: mette.holst@rn.dk
Received: September 20, 2017 Accepted: October 04, 2017 Published: October 11, 2017
Citation: Holst M, Ofei KT, Skadhauge LB, Rasmussen HH, Beermann T (2017) Monitoring of Nutrition Intake in Hospitalized Patients: Can We Rely on the Feasible Monitoring Systems? J Clin Nutr Metab 1:1.
Abstract
Rationale: Monitoring nutrition intake provides the basis for decision making on nutrition therapy in patients at nutritional risk and provides data on efficacy in nutrition intervention studies. Sufficient monitoring seems however difficult to achieve, and little is known about the specificity of current practises. This study aimed to investigate whether the nurses’ quartile nutrition registration method and the 24-hour recall dietary interview, may be used as a valid indication of a patient's energy- and protein intake in daily practice as well as clinical research, with regard to accuracy and feasibility.
Methods: For four week days, patients at nutritional risk admitted to Department of Medical Gastroenterology had all oral nutrition intakes measured by the nurses’ quartile nutrition registration method, the 24-hour recall dietary interview, single item weighed method, and the Dietary Intake Monitoring System [DIMS]. Statistical evaluation was performed between the three first methods, and a narrative assessment was made for the feasibility of the DIMS. Results: The 32 patients consumed on average 6755.5 ± 4921.2 kJ/day. Average protein intake was 54.5 ± 36.7 G/day. Average requirement was 6953 kJ/day and 80.8g protein/day. Overall, the nurses’ registration was well associated with the weighed method for energy as well as protein, with a slight but insignificant overestimation. The 24-hour dietary recall underestimated average total intake (E and P) significantly compared to the weighed method, mainly caused by underestimation of snacks and in particular lunch and drinks. However the difference may in a clinical point of view, be reasonable correlated to the weighed food record. The DIMS was found very positive for further development. Conclusion: The nurses’ quartile method for registration of food intake is practicable and sensitive enough for clinical practice as well as for research purposes. The 24-hour dietary recall interview is found less sensitive, however sensitive enough for decision-making in clinical practice. Not all patients were able to comply with the 24-hour recall interview.
The DIMS seems promising in individual planning of nutritional therapy.
Keywords: Nutritional risk; Clinical practice; Nutritional therapy; Gastroenterology; Dietary
Introduction
Monitoring nutrition intake is an important task and is included in good nutritional practice concerning hospitalized patients at nutritional risk. Information about a patient’s food intake is required in clinical practice, for evaluation of the energy- and protein intake, thus implying a need for supplementation, a revised nutrition plan, and a consultation by the clinical dietician. The dietary record form is thus mandatory for monitoring nutrition intake. Monitoring food intake allows early identification and prevention of nutritional decline in patients with a poor food intake during hospitalization, and has been recommended in various guidelines [1-3]. Recent reviews of nutritional procedures for medical in-patients suggest, based on ESPEN recommendations, that body weight is maintained in nutritional risk patients, who is able to reach 75% of their nutritional requirements [4-6]. In a recent double-blind, randomized, placebocontrolled study, it was shown that a specialized nutrient-dense oral nutritional supplement (ONS) containing high protein did not alter the primary composite endpoint of hospital readmission rates and mortality in malnourished hospitalized patients [6]. Thus, enteral tube feeding in patients at nutritional risk, should be implemented in medical in-patients with or at-risk of disease related malnutrition (DRM) who will not reach 75% of their energy- and protein targets within 5 days of oral feeding. Food intake should be re-assessed every 24 to 48 hours [1]. Despite this firm recommendation for nutrition intake, neither this review, or the guidelines question or recommend which methods to use for obtaining information about food intake, also known as “dietary record methods” [1-4]. The same lack of information about methods for dietary recording was found in another recent randomized controlled study (RCT), which had a specialized, nutrient-dense ready-to-drink liquid as intervention compared to another less dense liquid [6]. This was also seen, in systematic reviews and meta-analysis, which investigated nutritional support and outcome in malnourished medical in-patients, that no specific methods for monitoring and calculating nutrition intake were included [2,7].
Thus, there seems to be an obvious lack of interest for the diet registration methods used in clinical trials, although the result of a diet registration is mandatory to assist the clinician to decide on the launching of various forms of nutritional therapy before, during and after the clinical course, for patients at nutritional risk. Furthermore, the dietary record form in clinical nutrition research is especially relevant with regard to applied research studies, where nutrition intake is profound in the evaluation of the efficacy of interventions, as seen in several studies beforehand [8-12].
In clinical practice, as well as in studies using nutrition monitoring, it has been shown that dietary recording is difficult to implement, and often time consuming [9,12]. Studies have indicated, that lack of feasibility, especially with regard to time consumption and knowledge for the nursing staff in order to make nutrition monitoring part of daily practice for, clinical decision-making is too low, which also have been questioned in clinical research [9,12]. With regard to clinical research however, there is an even more important lack of accuracy, which has been described as related to misreporting, including underreporting as well as over-reporting as the main bias [13-22]. Especially regarding the little eating patients, the lack of accuracy may be a relevant bias, which we find have been questioned far too little in intervention studies.
In clinical practice, a relative estimate with a reasonable accuracy is probably sufficient. Earlier studies have concluded that accuracy within +/-17% weighted energy intake in 70% of individuals in a patient held diet record was sufficient for clinical practice [13]. Another study investigated the accuracy of a plate diagram sheet,- in the estimation of pre-plated meals, and found an overestimation of energy intake by +/-353 kcal/day and +/-16.4 g/day for protein intake, but found that this overestimation did not encompass the little eating patients [15].
The 24-hour dietary interview has been used in several studies and in several forms. The method has been challenged with regard to “patient” underreporting food intake when used with weight loss in mind. An Indian study used the method in dialysis patients at nutritional risk. In this study an under-reporting of 10% was seen, which was regarded acceptable for both research purposes, as for clinical practice purposes [21]. A resent review included 16 studies using 24-hour recall, and found a similar reporting bias [19]. Moreover, the method was used to estimate intake in a multimodal intervention study in a broad population of hospitalized patients. This study however found the challenge that only 63.7% of the 545 participants were able to comply with the interview, and that the interviews were very time consuming, and demanded the presence of a clinical dietician [10].
The weighed method is regarded the gold standard for accuracy towards registering food intake in the hospital setting. However, this method is extremely time-consuming and impractical for use in daily practice.
In daily practice today the nurses diet recording system, also called the “quartile method” is used by nurses for diet recording at Aalborg University Hospital, and was subsequently used in earlier studies in this setting [9-12,18]. Especially one of these studies however evaluated that the practicability of the dietary recording system for the nurses was low, since a very high number of forms were inadequately completed, and thus had to be excluded from the study. Some of these excluded forms would have most likely been adequate for use in clinical practice, but for the purpose of research, they were found invalid [9].
Aims
The purpose of the study was to investigate whether the nurses’ quartile nutrition registration method and the 24-hour recall dietary interview, may be used as a valid indication of a patient’s energy- and protein intake in daily practice as well as clinical research, with regard to accuracy and feasibility.
Secondly, the aim of the study was to narratively evaluate whether weighed images evaluation of the portions before and after eating, measured by the Dietary Intake Monitoring System [DIMS] [17,23,24], might provide a practical possibility for assessing food intake by a dietician.
Subjects and Methods
The study, which went on for four week-days, was designed as a comparison between four dietary registration methods, where the weighed method was considered the gold standard. The Bland- Altman method was used to determine the quality of the nurses’ registration method, the 24-hour diet recall method and DIMS, compared to the gold standard.
Participants were patients admitted to a department of medical gastroenterology at Aalborg University Hospital. All patients who were present at meals, and who were able and willing to understand the information given about the project, were invited to participate. Patients were informed about the registration procedures, and that serving of meals and handling of their trays afterwards, on the four study days, would possibly slightly delay the meals. Patients gave informed consent for participation.
Inclusion criteria
Patients were selected in cooperation with the nurse in charge, in the afternoons, every day before the study took place. This selection took place after ward rounds, to reduce the risk that enrolled patients who were discharged before end of study on the following day.
The patients included in the study were all patients at nutritional risk, according to screening by NRS-2002 [1]. Patients included should be able to eat and drink and not solely rely on tube or parenteral feeding, be willing to have their food weighed in single items, having food recording done by the nurses, and be able to contribute to a 24-hour diet recall interview. Furthermore, patients had to comply with having DIMS-pictures taken of their plates before and after the portion was eaten. Patients who had parenteral nutrition could participate if parenteral nutrition was supplemental to oral food intake, and if the amount of parenteral intake was stated. Including these patients was necessary since the unit included also patients with intestinal failure.
Description of the setting
The study was performed at the hospital ward at a department of medical gastroenterology at Aalborg University Hospital. In 24 beds, the ward provides therapy for hospitalized patients with intestinal failure, liver disease and inflammatory bowel disease, as well as a minor number of acute general medical conditions.
The daily servings include three main meals [breakfast, lunch and dinner] and three in-between snack meals. All food is prepared and delivered from the hospital central kitchen to a small satellite kitchen, placed just outside the ward. Here, the final preparation and arranging of the food is done before the serving assistant serves it from a trolley buffet. For the three main meals the buffet trolley is staffed with a service assistant, who serves meals for patients able to fetch the food by themselves. The nurses deliver meals to bed bound patients, and are also responsible for serving snack meals. Patients can order hot and cold drinks all day and food as well as oral nutritional supplementations 24 hours a day on request. During the study all intake was registered for patients included.
The model for serving food at Aalborg University Hospital is individually targeted decentralized portion serving, which in the dietary recording is plotted as served “small- medium or normal” portions. For the consumed portion it is recorded in quartiles whether respectively ¼, ½, ¾ of the entire served portion has been eaten. The portion sizes are calculated from the kitchen side per patient in accordance with “Recommendations of the Danish Institution Diet” [25].
24-hour dietary recall method
24-hour dietary recalls were obtained by a trained dietician on the day following the nurses’ registration and weighed food records. The recalls were conducted with photos of the actual meals and beverages, served within the past 24 hours. The photos illustrated all menu options at four different portion sizes. All patients who had been part of the nurses’ registration were invited to be included in the dietary recall. The interviewer started with the last served meal, and worked the way 24 hours back [10,21].
If patients had parenteral nutrition as supplement or single feeding, it was excluded from the recording during the study.
Nurses registration method
Nutrition intake was registered by the unit nursing staff on the diet record paper sheet which was implemented for use in daily practice 10 years ago, and has been adjusted for new food items on a regular basis. In the food registration system, foodstuffs and drinks were premeasured for energy (calories and kilojoules) and protein (grams) and registered in a computer program. Registrations were divided into registration of three main meals, in-between meals/snacks and drinks. Calculations for the main servings, drinks and supplements were registered on the back side of the registration records that was replaced on the bed side table by the patients every early morning in the night shift. All foodstuffs and drinks were written down on the registration record when served to, or taken by the patient. Food was registered in pieces or approximate quartile portion sizes as pre-printed on the registration record, and drinks were registered in approximate milliliters [9-11,18]. When the patient’s tray or dish was taken out, it was noted how much of the portion was taken, measured by what was left of the served portion. During the night shift the nursing staff collected the registration records and calculated the intake in the computer program. Results were registered in the registration records as well as in the patient files.
The DIMS
The DIMS is a combination of photo and weighed food portion data meant to obtain vital information on how much food is served and eaten in grams, as well as visual information of food choice preferences and intakes. The data available from the DIMS indicated in a former study, that measuring weight can improve the accuracy of estimating portion size from photo images, which are required for a more accurate energy and nutrient intake calculation. The data from DIMS might furthermore qualify the dietician to evaluate food intake and preferences by the choices patients have had and what they left on the plate, in order to make an improved individualized nutrition plan for nutritionally at risk patients [17,23-24].
Weighed method
A clinical dietician weighed all food items separately before they were put on the plate. After consumption, the patient / nurse presented the plate to the dietician again, and all left food items were weighed separately. The remaining food leftovers in grams per food item were subtracted from the served portion [13].
Statistics
Statistical analyses were performed using Excel 2013 for Windows. Baseline data are described as mean ± standard deviation [SD] and range. The mean energy and protein intakes estimated by the nurses’ registration and 24-hour dietary recall were compared with the results from the weighed records by paired t-test. Pearson correlations were used to assess associations between the different methods. The overall agreement for energy- and protein intakes between the methods was assessed by Bland-Altman plots and the limits of agreement estimated (average difference±1.96 SD of the difference). A p-value ≤ 0.05 was regarded as statistically significant.
For the narrative analysis of the DIMS, experienced dieticians were presented to these data separated from the weighed method.
Ethical considerations
Prior to inclusion, the patients were given written and oral information about the study. The participants were informed that they could withdraw from participation at any time during the study. The study was conducted according to the rules of the Helsinki Declaration of 2002. The study was put forward to the local ethic committee, which found that the project was not covered by the committees’ [Act no. 593 of 06/14/2011] definition of biological health science research, Committee Legislation § 14.1, see. § 2, Nos. 1-3.
Results
Demographic information
Over the four days, 32 patients were included in the study. All had meals, snacks and drinks registered by the nurses’ records and weighed food records. Above 75% of nutritional requirements were overall fulfilled by 97% of patients with regard to energy and 67% with regard to protein in both methods. Of the 32 patients, only 27 participated in 24-hour dietary recall on the following day. The patients that did not participate in the 24-hour dietary recall [n=5] was significantly diverse regarding: older age, higher BMI, higher protein requirement and lower intake. The main reason for drop-out from the 24-hour dietary recall was fatigue. The baseline characteristics of the study population can be seen in Table 1.
| All | + 24-hour recall | -24-hour recall | p-value | |
|---|---|---|---|---|
| n | 32 (25 W/7 M) | 27 (23 W/4 M) | 5 (2 W/3 M) | W/M ratio: 0.012 |
| Age (years) | 63.5 ± 12.9 (44-87) | 61.6 ± 12.7 (44-87) | 73.8 ± 8.6 (60-80) | 0.024 |
| Body weight Kg/Range | 67.5 (42-93.9) | |||
| BMI | 22.7 ± 4.7 (15.2-31.1) |
21.9 ± 4.4 (15.2-30.3) |
27.0 ± 4.0 (23.3-31.1) |
0.012 |
| NRS-2002 score | 4.0 ± 1.1 (3-7) | 4.1 ± 1.1 (3-7) | 3.8 ± 0.8 (3-5) | NS |
| Energy requirement kJ | 6953.1 ± 1033.1 (4500-9850) |
6864.8 ± 1094.8 (4500-9850 ) |
7430 ± 378.5 (6950-8000) |
NS |
| Protein requirement G | 80.8 ± 17.9 (50-122) |
77.8 ± 16.4 (50-122) |
96.8 ± 18.6 (79-117) |
0.013 |
| %energy fulfilled/ kJ/Kg/day | 97.1% / 100 | |||
| %protein fulfilled G/Kg/day | 67.5% / 0.81 |
Table 1: General characteristics of the participants.
Nutrition intake
The subjects consumed on average 6755.5 ± 4921.2 kJ/day. Average protein intake was 54.5 ± 36.7 g/day. Average requirement was 6953 kJ/day and 80.8 g protein/day. Data from the three methods are shown in Table 2.
| Energy kJ | Protein G | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Weighed | Registered | 24-hour recall | p-value weighed vs nurse registered |
p-value weighed vs 24-hour recall | Weighed | Registered | 24-hour recall | p-value weighed vs nurse registered |
p-value weighed vs 24-hour recall | |
| Breakfast | 832.6 ± 793.3 (0-2781) |
967.4 ± 1065.3 (0-4105) |
818.6 ± 704.4 (0-2145) |
5.3 ± 5.3 (0-19) |
5.1 ± 5.6 (0-23) |
6.1 ± 5.6 (0-15) |
||||
| Lunch | 1141.8 ± 899.6 (0-3953) |
940.5 ± 893.3 (0-4170) |
763.0 ± 665.4 (0-2730) |
10.4 ± 10.9 (0-49) |
9.6 ± 10.0 (0-50) |
8.2 ± 9.7 (0-40) |
||||
| Dinner | 1140.8 ± 943.9 (0-3941) |
1152.1 ± 1077.1 (0-3890) |
1058.9 ± 974.5 (0-3514) |
10.7 ± 8.4 (0-24) |
9.0 ± 7.4 (0-30) |
11.5 ± 9.9 (0-35) |
||||
| Snacks | 1474.6 ± 1846.5 (0-7893) |
1495.6 ± 1613.9 (0-6680) |
1299.3 ± 1766.9 (0-7460) |
9.0 ± 11.2 (0-43) |
8.7 ± 10.6(0-38) |
7.8 ± 10.1 (0-43.6) |
||||
| Drinks | 2179.5 ± 2101.0 (0-6774) |
2437.5 ± 2036.7 (0-6740) |
1857.6 ± 1599.7 (0-5890) |
19.1 ± 18.0 (0-68) |
21.1 ± 19.5 (0-76) |
17.7 ± 17.9 (0-63) |
||||
| Total | 6755.5 ± 4921.2 (272-23783) | 6993.1 ± 4878.4 (347-20775) |
5815.0 ± 4506.3 (1178-19761) |
0.37 | 0.04 | 54.5 ± 36.7 (5-160) | 53.5 ± 35.2 (3-149) |
51.4 ± 37.3 (7-153) |
0.21 | 0.002 |
Table 2: Correlations between methods, Energy (kJ/day) and protein (g/day) intake estimated by the nurses’ registration (registered) and 24-hour dietary recall compared to weighed food intake (weighed).
Nurses’ registration vs weighed method
Overall, the nurses’ registration was well associated with the weighed method. On average, total energy intake was slightly, but not significantly, overestimated by the nurses registration compared with the weighed method (237.6 kJ) (p=0.37), mainly attributable to an overestimation of the drinks (258 kJ) and breakfast (134.8 kJ). However, lunch seemed to be underestimated by the nurses’ registration (201.3 kJ).
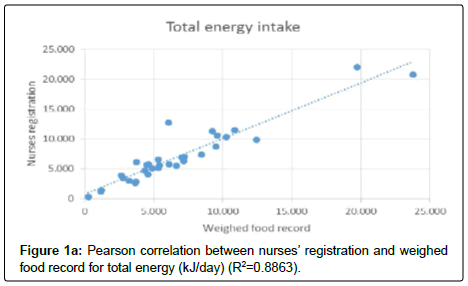
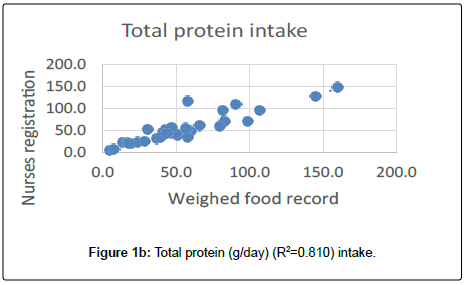
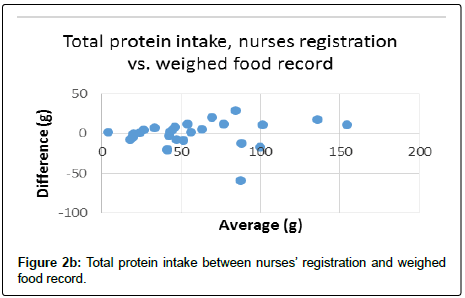
Total protein intake was not significantly different between the two methods. On average the nurses’ registration underestimated by 1 g/day (p=0.21). Total energy and protein intake estimated by the nurses’ registration were highly correlated to the weighed food record (Figure 1a and 1b).
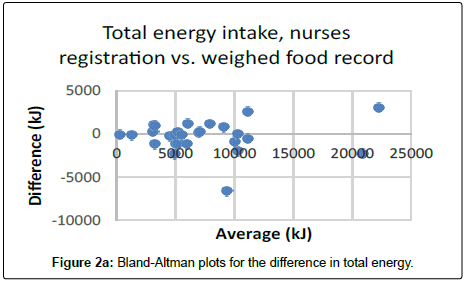
The limits of agreement between weighed records and nurses registration for energy intake were -2126.8 kJ/day to 1475.6 kJ/day (R2=0.883) and for protein intake -17.2 g/day to 16.4 g/day (R2=0.758). The Bland–Altman plots can be seen in Figure 2a and 2b.
24-hour dietary recall vs weighed method
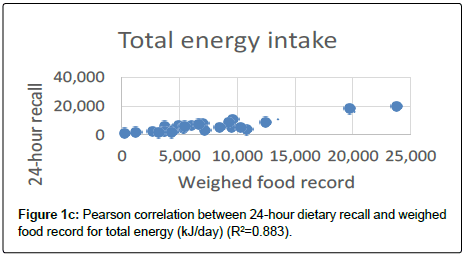
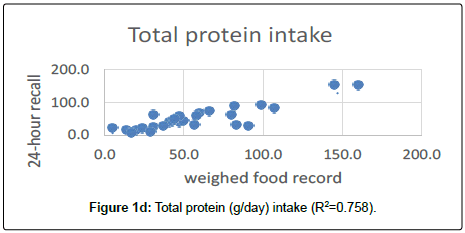
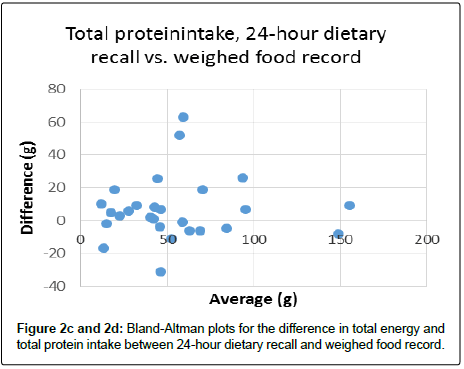
The average total energy intake was significantly underestimated (940.5 kJ, p=0.004) by the 24-hour dietary recall compared to the weighed method (p=0.04). Mainly caused by underestimation of snacks (175.3 kJ) and in particular lunch (378.8 kJ), and drinks (321.9 kJ). On average, total protein intake was underestimated by 3.1 g (p=0.002). Again, this was caused by snacks, lunch and drinks. However, total energy and protein intake estimated by the 24-hour dietary recall May in a clinical point of view, be seen as reasonably correlated to the weighed food record (Figure 1c and Figure1d).
The Bland–Altman plots can be seen in Figure 2c and Figure 2d. The limits of agreement between weighed records and 24-hour dietary recall for energy intake were -918.2 kJ/day to 3678.4 kJ/day and for protein intake -12.5 g/day to 25.9 g/day.
Discussion
This study aimed to investigate whether the nurses’ nutrition registration method and the 24-hour recall dietary interview, may be used as a valid indication of a patient’s energy -and protein intake in daily practice as well as in clinical research, with regard to accuracy and feasibility.
We included 32 patients, and anticipated that patients would have all registration methods performed. The single food item weighed method was used as “gold standard”. As expected, this method was found extremely time consuming for staff and for patients waiting for their food. However, the single item weighing of all served food 24 hours daily ensured the accuracy of this study, as opposed to another recent study, which weighed single items of leftovers, only for breakfast and lunch in a selected population [13].
This study showed a significant correlation between the nurses’ registration of food intake and actual intake as measured by weighing the food, and seemed to be more accurate than 24-hour dietary recall, that significantly underestimated the energy -and protein intake. The correlation between the nurses’ registration and weighed method showed that the nurses’ registration methods were more accurate compared to the 24-hour recall method. This difference could be expected since the nurses’ registration is prospective, and done immediately during and after the meal. Thus, the risk of under- or overestimation due to recall bias, as seen by 24-hour recall method in other studies, will be eliminated [19,21]. The reported mean differences in energy, calculated using the 24-hour recall and the weighed method, could be related to reporting and portion size estimation errors . The 24-hour recall method which relies on memory is prone to leave out of some of the food items consumed- The estimation of portion size presents one of the challenges in dietary assessment, especially if it is done by untrained persons such as patients. They are more likely to underestimate portion sizes, which can increase the inaccuracy of the method. As recognized in a former study, we did not succeed in having 24-hour recall interviews with all patients, even though their specific inclusion was discussed with the nurse in charge. Again, this was due to patients feeling too tired to go through with the interviews [10]. Nevertheless, we find that the data is sensitive enough to support that we would still recommend 24-hour recall for selected patients, i.e. patients who need a nutrition plan right on admission, or some ambulatory patients, who did not have the opportunity to do nutrition registration at home.
Narrative evaluation of the DIMS
The combination of accurate total weight with pictures of the portion before and after food consumption, was found by the dieticians to give a very good idea of energy and protein consumed, and especially also about patient preferences. This way, they found, that for clinical practice, this would be a very good and practical tool to use for preparation of an individual counseling with the patients. This could also give the opportunity to bring relevant special suggestions for a food menu, after consultation with the hospital kitchen, before the patients was seen. They found that this was definitely a method to further develop in to clinical practice, but also, that the system was not sensitive enough for either clinical practice or research. They found that a performance in 3D would improve the possibility to see how much food of each item was on the plate, and that recipes are mandatory for accurate evaluation of hot meals, especially stews and soups.
In relation to the DIMS, a previous study conducted in the same setting indicated that before and after consumption digital images and total weight of plate contents could be useful in addressing memory recall and portion size estimation errors. Although it does not provide weight of each food item, the total weight estimated by the 24-hour recall method could be compared and adjusted. An IT on-line based registration model would be preferred in the near future, and can be based on the knowledge from the existing system.
A tool for diet recording in a university hospital setting must
1. Be sufficiently accurate for use in clinical practice as well as in research, thus appropriate regarding internal and external validity.
2. Be practicable and able to be used by the staff who serve meals, by the nurses and by patients capable of registering themselves.
3. Be adjustable for development of new food items and serving methods.
Limitations
The fulfilling of energy and protein above 75% is strived in all nutritionally at risk patients. In this study this was practically fulfilled in all patients with regard to energy, but only in 76% of the patients for protein.
However, there may be some uncertainty associated with this serving model, as all caregivers, including nurses serving for patients, are not professionally trained to estimate portion size according to the recommendations, and serving in this study was done as usual practice, since we aimed at practicability.
The participating nurses used a registration method of which they were familiar, since this method was implemented in the setting many years before. This study does not support, whether the method would be as accurate in a setting to where it is new, or in patients who would prefer to fill the form in themselves.
Conclusions
The nurses’ method for registration of food intake including quartiles of served portion had a statistically significant correlation to weighed method, and is evaluated to be practicable and sensitive enough for clinical practice as well as for research purposes.
The 24-hour dietary recall interview is found less sensitive, however sensitive enough for decision-making in clinical practice. Not all patients were able to comply with the 24-hour recall interview.
The DIMS seems to be a very promising assessment tool for dieticians in individual planning of nutritional therapy.
References
- Kondrup J, Allison SP, Elia M, Vellas B, Plauth M (2003) ESPEN Guidelines for Nutrition Screening 2002. Clin Nutr 22: 415-421.
- Bounoure L, Gomes F, Stanga Z, Keller U, Meier R, et al. (2016) Detection and treatment of medical inpatients with or at-risk of malnutrition: Suggested procedures based on validated guidelines. Nutrition 32: 790-798.
- Braga M, Ljungqvist O, Soeters P, Fearon K, Weimann A, et al. (2009) ESPEN Guidelines on Parenteral Nutrition: surgery. Clin Nutr 28: 378-386.
- Kondrup J, Bak L, Hansen BS, Ipsen B, Ronneby H (1998) Outcome from nutritional support using hospital food. Nutrition 14: 319-321.
- Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, et al. (2016) ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 36: 49-64.
- Deutz NE, Matheson EM, Matarese LE, Luo M, Baggs GE, et al. (2016) Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: A randomized clinical trial. Clin Nutr 35: 18-26.
- Bally MR, Blaser Yildirim PZ, Bounoure L, Gloy VL, Mueller B, et al. (2016) Nutritional Support and Outcomes in Malnourished Medical Inpatients: A Systematic Review and Meta-analysis. JAMA Intern Med 176: 43-53.
- Sullivan SC, Bopp MM, Weaver DL, Sullivan DH (2016) Innovations in Calculating Precise Nutrient Intake of Hospitalized Patients. Nutrients 8: 412.
- Holst M, Mortensen MN, Jacobsen BA, Rasmussen HH (2010) Efficacy of serving bed-side in-between meals - An intervention study in three medical departments. ESPEN J 5: e30-36.
- Holst M, Beermann T, Mortensen MN, Skadhauge LB, Lindorff-Larsen K, et al. (2015) Multi-modal intervention improved oral intake in hospitalized patients. A one year follow-up study. Clin Nutr 34: 315-322.
- Holst M, Sondergaard LN, Bendtsen MD, Andreasen J (2016) Functional training and timed nutrition intervention in infectious medical patients. Eur J Clin Nutr 70: 1039-1045.
- Holst M, Laursen BS, Rasmussen HH (2012) Caring for Dinner in Hospital. J Nurs Care 1: 117.
- Gariballa SE, Forster SJ (2008) Dietary intake of older patients in hospital and at home: the validity of patient kept food diaries. J Nutr Health Aging 12: 102-106.
- Cox Sullivan S, Bopp MM, Roberson PK, Lensing S, Sullivan DH (2016) Evaluation of an Innovative Method for Calculating Energy Intake of Hospitalized Patients. Nutrients 8: 557
- Bjornsdottir R, Oskarsdottir ES, Thordardottir FR, Ramel A, Thorsdottir I, et al. (2013) Validation of a plate diagram sheet for estimation of energy and protein intake in hospitalized patients. Clin Nutr 32: 746-751.
- Budiningsari D, Shahar S, Manaf ZA, Susetyowati S (2016) A simple dietary assessment tool to monitor food intake of hospitalized adult patients. J Multidiscip Healthc 9: 311-322.
- Ofei KT, Dobroczynski MT, Holst M, Rasmussen HH, Mikkelsen BE (2014) The Dietary Intake Monitoring System (DIMS)- An Innovative Device for Capturing Patient’s Food Choice, Food Intake and Plate Waste in a Hospital Setting.
- Olin AO, Osterberg P, Hadell K, Armyr I, Jerstrom S, et al. (1996) Energy-enriched hospital food to improve energy intake in elderly patients. JPEN J Parenter Enteral Nutr 20: 93-97.
- Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van't Veer P (2009) Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr 2: 73-85.
- Ribas Barba L, Serra-Majem L, Roman-Vinas B, Ngo J, Garcia-Alvarez A (2009) Effects of dietary assessment methods on assessing risk of nutrient intake adequacy at the population level: from theory to practice. Br J Nutr 2: 64-72.
- Sharma M, Rao M, Jacob S, Jacob CK (1998) Validation of 24-hour dietary recall: a study in hemodialysis patients. J Ren Nutr 8: 199-202.
- Sullivan SC, Bopp MM, Weaver DL, Sullivan DH (2016) Innovations in Calculating Precise Nutrient Intake of Hospitalized Patients. Nutrients 8: 412.
- Ofei KT, Holst M, Rasmussen HH, Mikkelsen BE (2015) Effect of meal portion size choice on plate waste generation among patients with different nutritional status. An investigation using Dietary Intake Monitoring System (DIMS). Appetite 91: 157-164.
- Ofei KT, Holst M, Rasmussen HH, Mikkelsen BE (2014) How practice contributes to trolley food waste. A qualitative study among staff involved in serving meals to hospital patients. Appetite 83: 49-56.
- Pedersen AN, Ovesen L (2009) Recommendations for the Danish Institution Diet.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi