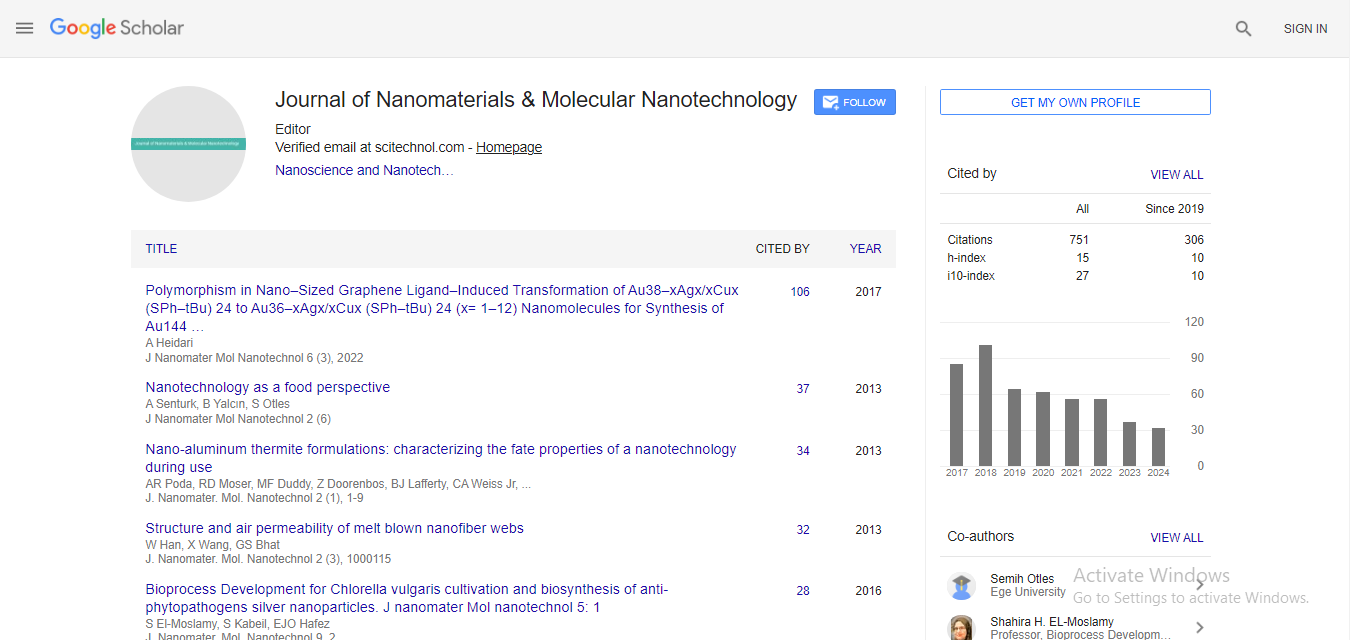
Review Article, J Nanomater Mol Nanotechnol Vol: 9 Issue: 4
Nanomaterial Approaches for the Prevention, Diagnosis and Treatment of COVID-19: A Paradigm Shift
Sougata Ghosh1,2, Ebrahim Mostafavi2, Ada Vernet-Crua2, and Thomas J Webster2*
1Department of Microbiology, School of Science, RK University, Rajkot, 360020, India
2Department of Chemical Engineering, Northeastern University, Boston, 02115, USA
*Corresponding Author : Thomas J Webster
Department of Chemical Engineering, Northeastern University, Boston, 02115, USA
E-mail: th.webster@neu.edu
Received: June 05, 2020 Accepted: June 15, 2020 Published: July 31, 2020
Citation: Ghosh S, Mostafavi E, Vernet-Crua A, Webster TJ (2020) Nanomaterial Approaches for the Prevention, Diagnosis and Treatment of COVID-19: A Paradigm Shift. J Nanomater Mol Nanotechnol 9:4. doi: 10.37532/jnmn.2020.9(4).280
Abstract
The global impact of the 2019 novel coronavirus (Severe Acute Respiratory Syndrome Coronavirus 2(SARS-CoV-2)) that emerged in Wuhan, China is alarming due to its rapid spread to 203 countries and territories by April 2020. To date, 14,909,279 individuals have been infected which has claimed 614471 lives. Although originating in animals, the virus has adapted a human-to-human mode of transmission presently which has challenged all existing antiviral therapies. Unfortunately, no drug or vaccine has yet been approved to treat COVID-19 because available therapeutics like monoclonal antibodies, oligonucleotide-based therapies, peptides, interferon therapies and small-molecule drugs might not effectively target the virus and take too long to develop. Hence, it is likely that it will take at least a year before treatment (e.g., a vaccine) becomes available, which is distressing. Herein, we present the first nanoscale alternatives (including one of the most successful nanomedicines developed by Moderna) for the effective control and containment of COVID-19 considering the urgency of the SARS-CoV-2 outbreak.
Keywords: COVID-19; Human emergence; Global impact; Therapeutic challenges; Nanoprophylactic strategies
Introduction
The emergence of the 2019 novel coronavirus, designated as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is responsible for the severe disease now denoted as COVID-19. Its rapid cross border transmission has led to its quick spread into 203 countries and territories which prompted the World Health Organization (WHO) to declare COVID-19 a global pandemic on March 11, 2020. As of July 21, 2020 there were at least 23,676,599 patients diagnosed with COVID-19 worldwide among which 813,789 have died. Further, it is widely known that there are under reported cases and deaths due to the wide disparity in how they are reported around the world. Among the affected countries, USA has the largest population of confirmed cases (3,964,361) followed by Brazil (2,121,645) and India (1,171,356). The highest death toll (177,284) has been recorded in USA which has surpassed its place of origin in China (4634) [1,2].
Coronavirus belongs to the family Coronaviridae and the order Nidovirales and is broadly distributed in humans and other mammals [3]. Generally, most human coronavirus infections are not lethal. However, in past two decades, betacoronaviruses, like severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East Respiratory Syndrome coronavirus (MERS-CoV) resulted in more than 10,000 cases, with 9.6% and 34.4% mortality rates, respectively [4-10]. The absence of prophylactic vaccines against this enveloped non-segmented positive sense RNA virus has been attributed to its uncontrolled prevalence now throughout the globe.
Outbreak of COVID-19
Wuhan in Hubei Province of China witnessed a marked increase in cases of severe pneumonia due to an unknown cause in December, 2019 and the outbreak was associated with exposures in one seafood market. As per the WHO, the clinical signs and symptoms included mainly dry cough, malaise, and fever, with a few cases having difficulty in breathing, and chest radiographs showing invasive pneumonic infiltrates in both lungs. However, no clear evidence of 'humanto- human' transmission was reported at this point (WHO-Novel coronavirus). Immediate investigation to characterize the disease included isolation of the patients, close monitoring of personal contacts, collection of clinical and epidemiological data from patients and efforts to develop diagnostic and treatment methods. A novel coronavirus designated as SARS-CoV-2 was isolated from patients in Wuhan by January 7, 2020 which enabled the rapid development of point-of-care real-time RT-PCR diagnostic tests specific for SARSCoV- 2 based on the full genome sequence data on the Global Initiative on Sharing All Influenza Data (GISAID) platform [11]. Cases were no longer limited to Wuhan and, thus, more than 800 cases were also confirmed in other provinces in China, as it shortly spread to Thailand, Japan, South Korea, and the USA [3].
A turning point emerged in the COVID-19 threat when [12] reported human-to-human transmission [12]. Among six family members from Shenzhen, Guangdong Province, China, who travelled to Wuhan, five were identified as infected with SARS-CoV-2. It is interesting to note that one family member, who did not travel to Wuhan, also became infected with the virus after several days of contact with four family members. In view of this background, it was speculated that although this novel coronavirus might have first originated from animals and now jumped into humans, the mode of person-to-person transmission could gain prominence. Contraction of the viral infection by patients with no known history of exposure to markets or animals might be from rapid intercity spreading, even possibly by air travel [12,13] had predicted a potential threat posed by the circulating bat as SARS CoV SHC014 because of the ability of chimeric SHC014 viruses to replicate in human airway cultures [13,14]. It was reported that SARS-like coronaviruses, isolated from Chinese horseshoe bats may gain the ability to attach to Angiotensin Converting Enzyme 2 (ACE2) receptors in the lower respiratory tract of humans. This mechanism to gain entry may facilitate cross infectivity of human hosts [13,14]. They had warned about the high probability of this mutated virus to evade current therapeutics. This emphasized the need for surveillance and preparedness for improved therapeutics against circulating SARS-like viruses [14].
Challenges in the diagnosis and therapies for COVID-19
The evolution in host/vector specificity indicates that potentially more novel and severe underlying zoonotic events may empower the virus to acquire new traits, mode of infection and resistance to available drugs. As an RNA virus, SARS-CoV-2 has the inherent feature of a high mutation rate that might enable the viral pathogen to adapt for more efficient transmission from person to person and possibly become more virulent [11]. Rapid detection and effective public health measures are being designed to ensure containment of the infection. Hereby, it is very critical to arm the front-line clinics with validated point-of-care diagnostic kits for early detection and therapy. Advanced technologies including reverse transcription PCR (RT-PCR), real-time reverse transcription PCR (rRT-PCR), reverse transcription loop-mediated isothermal amplification (RTLAMP), and real-time RTLAMP as well as multiplex nucleic acid amplification and microarray-based assays are being used for SARSCoV- 2 detection in humans as well as other animal hosts. Ritonavirboosted lopinavir monotherapy has been launched for SARS-CoV-2 (ChiCTR2000029308). Various vaccine development strategies include inactivated SARS-CoV-2, pre-fusion S protein, Matrix-M and recombinant SARS-CoV-2 for inducing an immunogenic. The vector based recombinant vaccine include the adenovirus type 5 vector (Ad5-nCoV) and chimpanzee adenovirus vaccine vector (ChAdOx1). Further, optimized DNA vaccines encoding S protein of SARSCoV- 2 are in Phase I/II of clinical trials but not yet commercially available [15]. The NIH in the USA has prioritized the evaluation of the therapeutic potential of remdesivir, corticosteroids (including dexamethasone), immune-based therapy using mesenchymal stem cells, vitamin C, vitamin D, zinc supplements, Janus Kinase (JAK) inhibitors and Bruton’s Tyrosine Kinase (BTK) inhibitors for the treatment of COVID-19 [16].
Despite the wide spread talk over making detection methods more available, it appears that it will be at least a year before treatment (e.g. a vaccine) becomes available, which is unacceptable and necessitates a paradigm shift in our thinking. We clearly need platform technologies that can be easily adapted to every new virus or virus mutations to accelerate such viral treatments.
Nanomedicine as antiviral theranostics
Theranostics, the combination of diagnosis and treatment, is proposed to be one of the principal options towards controlling and eliminating viral infections. In the past years, rather than relying on the immune system, investigations have been focused on obtaining vaccine formulations. Table 1 shows several vaccine formulations that have been successfully developed and applied over the years for different viral infections such as hepatitis C, smallpox or measles, showing a sharp decrease on associated mortality and morbidity, hence demonstrating that vaccines are a vital component for viral disease prevention [17]. Special efforts have been completed towards CoV vaccines due to the 2002-2003 SARS outbreak, as reported by McPherson et al. [18] in which insect cell expression was used for the rapid production of the SARS vaccine [18]. Although there are several promising vaccines for different respiratory viruses, the high level of antigenic drift which generates genetic mutations of some viruses, challenges the efficacy and methods used in developing vaccines today, especially if they take over a year every time a new virus presents a healthcare problem. This could be observed in Tseng et al. [19], where four different SARS-CoV vaccine formulations were tested in mice and ferret models demonstrating variable efficacy and histopathologic changes due to possible differences in viral replication [19].
| Material | Size (nm) | Virus | Antigen/Epitope | Adjuvant |
|---|---|---|---|---|
| Inorganic nanoparticles | ||||
| Gold | 12 | Influenza | M2e | CpG |
| Polymeric nanoparticles | - | |||
| PLGA | 225.4 | Bovine parainfluenza 3 virus | BPI3V proteins | - |
| (BPI3V) | ||||
| 200-300 | Swine influenza virus (H1N2) | Inactivated virus H1N2 antigen | - | |
| Chitosan | 140 | Influenza (H1N1) | H1N1 antigen | - |
| 300-350 | Influenza (H1N1) | HA-Split | - | |
| Polyanhydride | 200-800 | RSV | F and G glycoproteins | - |
| Self-assembling proteins and peptide-based nanoparticles | ||||
| N nucleocapside | 15 | RSV | RSV phosphoprotein | R192G |
| protein of RSV | ||||
| Ferritin | 12.5 | Influenza (H1N1) | M2e | - |
| Others | ||||
| VLP | 80-120 | Influenza (H1N1) | Hemagglutinin | - |
| DLPC (Dilauroylphosphatidylcholine) liposomes | 30-100 | Influenza (H1N1) | M2, HA, NP | MPL and trehalose 6,6′ dimycolate |
Table 1: Nanoparticle-based vaccines against respiratory viruses delivered via the intranasal route [20].
Therefore, innovative alternatives related to the concept of “universal vaccines” are needed at this time. The use of nanotechnology, or with material dimensions below 100 nm in at least one dimension, has gained popularity in numerous fields most notably medicine. The use of Nanoparticle (NPs) formulations against respiratory viruses propose an advantage to current alternatives in terms of safety, effectivity and cost [20]. The reason behind this is mainly related to their small size, since SARS-CoV-2 with their associated proteins, falls within the same size range (60 nm-140 nm), hence facilitating the interaction [21,22]. Moreover, NPs have a non-replicating nature and nanoscale morphology that allows multivalent antigen display as well as controlled delivery that provides increased efficacy as tested in malaria, influenza or HIV formulations [23]. As an example, the use of protein NPs in combination with adenovirus serotype 5 and an aluminium adjuvant was used as a vaccine formulation for the treatment of Middle East Respiratory Syndrome coronavirus (MERSCoV). The study showed improved humoral and immunogenic responses in mice due to the use of protein NPs that could probably avoid weak T-cell response [24]. Other advantages in the use of nanomaterials are related to the ease of administration of NPsbased antiviral vaccines (known as nanoprophylactic vaccines) via sub-cutaneous, intramuscular injections, oral and intranasal routes helping efficient penetration through the capillaries as well as mucosal surfaces [25]. Besides, it is significant to note that NPs can protect the native structure of antigens from proteolytic degradation and/or improve antigen delivery to Antigen-Presenting Cells (APCs), even promoting their bioactivity, which is critical for boosting the immune response [26]. Further, a phenomenon called the local depot effect can be achieved when using NP formulations. This effect allows for the slow release of an antigen, hence ensuring prolonged antigen presentation to immune cells which leads to effective immunomodulation [27].
Different nanoplatforms, displaying relevant antigenic moieties, including inorganic (gold and silver) NPs, polymeric NPs, Virus-Like Particles (VLPs), liposomes and self-assembled protein NPs have been studied as potential viral vaccine formulations (Figure 1). From all those approaches, VLPs have received significant attention recently for the treatment of CoV since they present high immunogenic behavior in a safer approach since no attenuated or inactivated virus are used [28]. For instance, SARS-VLPs containing SARS S and influenza M1 proteins showed high immunogenic behavior and neutralized antibodies in mice, suggesting a possible formulation to provide protection for such diseases [29]. Similarly, Wang et al. [30] produced MERS-CoV VLPs that showed excellent immunogenicity on Rhesus macaques via T-helper 1 cell immunity mechanisms [30]. Additionally, the use of self-assembling proteins is based on the structure that CoV presents. This type of virus presents four different structural proteins, hence by introducing protein-based NPs it can be possible to neutralize antibodies in a rapid and effective way. This was reported by Coleman et al. [31] where MERS- and SARS-CoV protein spike NPs induced higher titre antibodies in mice [31].
Figure 1: Targets for nanotherapeutics against SARS-CoV-2 [20].
On the other hand, the rest of the NP formulations have also been highly investigated for other viral infections. Polymeric NPs allowed for high encapsulation efficiency as well as controlled release of vaccine adjuvants and drugs with low associated toxicities [32]. In an elegant study, Lee et al. [33] presented a polymer-templated protein nanoball system which was capable to orient hemagglutinin1 in influenza virus and increase immunogenicity in mice. This kind of structure showed and presented an advantage regarding VLPs due to a straightforward and cost-effective approach without the necessity of using complex genetic techniques [33].
Furthermore, inorganic NPs present smaller sizes with highly active and tunable surfaces, representing reasons why they are mainly used as diagnosis tools [34]. For instance, a gold (Au) NP singlestep, highly sensitive electrochemical immunosensor was used to selectively detect MERS-CoV at quantities as small as 0.4 pg/ml. This was possible due to the excellent optical and electronic properties of AuNPs which increase due to the high surface area to volume ratios of NPs [35].
What makes these materials interesting is that they are highly tunable in terms of size, shape, solubility, surface chemistry or hydrophilicity making these structures ideal for the incorporation of antigens by encapsulation (physical entrapment) or by conjugation (covalent functionalization). The immunological response of AuNPs against the West Nile virus was found to be size and shape dependent. The authors demonstrated that while 40 nm spherical NPs induced a high release of antibodies, this was 50% reduced when rod-shaped or 20 nm spherical NPs were employed [36].
Jung et al. [37] showed that Gold Nanorods (GNRs) mediated plasmonic photothermal therapy where both adenoviral gene delivery and hyperthermia were achieved simultaneously. Well defined structures of the GNRs exhibited a localized Surface Plasmon Resonance (SPR) peak in the near-infrared wavelength. GNRs with SPR peak in the near-infrared region (700 nm-900 nm) were found to be favorable for in-vivo studies as light within this spectrum window has a deeper penetrating power than visible light. Moreover, this wavelength is not substantially absorbed by the aqueous environment. At 0.4 W/cm2 laser power of NIR, the temperature increased from 23.5°C to 41.2°C for 24 μg/mL of GNRs. Similarly, a PEGylated GNR concentration of 48 μg/ml resulted in the desired temperature for in vivo studies at 42°C. This mild hyperthermia improves the rate of cellular uptake of nanoparticle loaded drugs or vaccines, due to better internalization via clathrin mediated endocytosis. This photothermal therapy can be further explored for hindering intracellular viral replication against SARS-CoV-2.
When summarizing the use of NPs-based vaccines, it is clear that they are a powerful alternative to overcome current limitations in the field. The use of nanotechnology might provide cost-effective, straightforward, easy to scale-up and fast methodologies to such changing diseases. Nonetheless there is still work to do regarding cytotoxicity as well as efficacy of the formulations, taking into account the current length of vaccine approval which is an average of 10 years.
Nanoprophylactic strategies against COVID-19
Nanoparticles (such as carbon nanotubes (CNTs), graphene oxides, poly (lactic-co-glycolic acid) (PLGA), polystyrene, titanium dioxide (TiO2), mesoporous silica, and aluminium oxyhydroxide) have all been reported to induce NLRP3-associated inflammasome activation [38]. Dendrimer-based RNA nanoparticle vaccine mediated immunization resulted in a unique H-2Db-restricted epitope specific CD8+ T cell response in a mouse model that was effective to control the Zika virus (ZIKV) [39]. On internalization by Antigen Presenting Cells (APCs), these nanoparticles generated signals that triggered lysosomal destabilization and generation of Reactive Oxygen Species (ROS), leading to the release of lysosomal content, including cysteine protease cathepsin B. This protease was further sensed by NLRP3 which subsequently activated the formation of the inflammasome complex [22]. Interleukins are secreted to promote downstream signalling. Immune cells are activated and recruited for the effective elimination of a virus. In view of this background, nanoscale antigen carriers and immune cell activators can prove to be a powerful strategy for the control of SARS-CoV-2 and should be the focus of more investigation. A platform nanoparticle approach could be approved as a strategy simply modified to treat additional viruses as they pose new threats to human health, to collectively introduce a much faster way to treat viral infections than today’s slow vaccine development methods.
Since there are no available vaccines or specific treatments for COVID-19, researchers from various domains are trying to develop new therapeutic strategies to inhibit their pathogenicity. It is important to note that the size of a virus (120 nm) provides a significant cue for developing nano-scale medicine and technology to treat the disease. Nanostructures with similar dimensions can adhere to SARS-CoV-2 which may further disrupt their structure simply upon attachment or when irradiated with infrared light. This structural alteration would then impair infectivity, survival and multiplicity of the virus. These nanoscale materials could also have dual benefits for effective detection of the virus as well as therapy, within the same nanoparticle. This is in contrast to our slow current approach of developing one method to detect viruses and yet another method to treat viruses.
Human-to-human transmission of the virus may happen due to generation of tiny droplets of viral particles-from breathing, talking, sneezing, coughing-that enter the body through the eyes, mouth, or nose. These viruses may remain viable for several days on inanimate surfaces. Bioactive nanomaterials can inhibit the virus upon spraying onto surfaces. As just one of many example, nanotextures have been placed on everyday surfaces to create surface energies that can repel water droplets that contain viruses. Exotic magnetic nanoparticles can also be directed by magnetic fields to specifically target organs like the lungs and other areas susceptible to respiratory complications after contracting viral infections. Moreover, nanocarriers loaded with antiviral drugs can be targeted with viral antigen (spike) specific antibodies (monoclonal and polyclonal neutralizing antibodies).
Inorganic Gold Nanoparticles (AuNPs) have been functionalized with the peptide consensus M2e of influenza A viruses with a non-native cysteine residue at the C-terminal end via thiolate-Au chemistry. Intranasal administration of M2e-AuNPs in mice with a CpG (cytosine-guanine rich oligonucleotide) adjuvant showed a strong immune response against the influenza virus PR8 strain [20].
Polymeric nanoparticles like spherical PLGA-NPs (200 nm- 300 nm of diameter) were used to encapsulate inactivated Swine Influenza Virus (SwIV) H1N2 antigens (KAg) via a water/oil/water double emulsion solvent evaporation. Milder disease was observed in pigs vaccinated twice with this preparation on infection with a virulent heterologous influenza virus strain [20].
Virus like particles with spherical supramolecular assemblies 20 nm-200 nm diameter composed of self-assembled viral capsid proteins have also shown promise. Intranasal delivery of influenzaderived VLPs exposing 5 repeats of the M2e epitopes elicited humoral and cellular immune responses against different serotypes of influenza viruses [20].
Self-Assembling Protein Nanoparticles (SAPNs) ranging in diameter from 20 nm-100 nm identical to the sizes of many viruses can be used as nanovaccine candidates against respiratory viruses. SANPs, fabricated to show an immune response against Respiratory Syncytial Virus (RSV), were explored using the nucleoprotein (N) from the virus nucleocapsid. The N protein is the prime target for an antigenspecific cytotoxic T-cell response. Supramolecular nanorings 15 nm diameter are formed due to the self-assembly of N protein protomers. Further modification was achieved by fusing the FsII epitope targeted by the monoclonal neutralizing antibody (palivizumab) to the N protein, resulting in the formation of chimeric nanorings with an enhanced immune response and virus protection against RSV [20].
Targeting with nanotherapeutics as a future strategy
CoVs possesses an envelope made up of a lipid bilayer that is derived from the host cell membrane. The primary structural proteins associated with the virus are spike (S), membrane (M), envelope (E), and nucleocapsid (N) proteins, and hemagglutinin-esterase (HE) protein in some betacoronaviruses. The N protein is located in the core that forms the nucleocapsid and interacts with the viral RNA for its packaging during viral assembly. It is important to note that the RNA genome of CoVs is the second largest of all RNA viruses, ranging from 26 to 32 Kilobases (Kb) in size. S, M, and E proteins are all embedded in the viral envelope. Profusely glycosylated S protein forming homometric spikes facilitates viral entry into the host cell. The most abundant M protein is responsible for the shape, while the E protein is present in low quantities and mediates the assembly and formation of the envelope [40,41]. CoV-2 is closely related to SARS-CoV, which has only a 12.8% difference with SARS-CoV in the S protein and has 83.9% similarity in minimal receptor-binding domain with SARS-CoV. Further, SARS-CoV-2 has an additional novel glycosylation site [41,42].
Jiang et al. [43] confirmed that the S protein of SARS-CoV-2 consists of a S1 subunit which contains two functional domains, the N-Terminal Domain (NTD) and a Receptor-Binding Domain (RBD), both of which are responsible for binding of the virion to the receptor on the host cell (Figure 1) [43,44]. This part harbors several conformational neutralizing epitopes which can serve as potential targets for the fabrication of neutralizing monoclonal antibody-(mAbs) functionalized nanomaterials. These target specific nanomedicines can selectively bind to the S1 subunit of the S protein, particularly the RBD leading to impairment of host surface recognition and attachment [45]. The S2 subunit contains three functional domains, a fusion peptide (FP), and heptad repeat (HR) 1 and 2. Binding of RBD in S1 to the receptor results in a conformational change in the S2 subunit due to insertion of FP into the host cell membrane and association between HR1 and HR2 to form six helical bundles (6-HB). This leads to fusion between viral and cellular membranes that facilitate the entry of the viral genetic materials into the host cell through the fusion pore for replication in the cell [45]. Thus, nanoparticles targeting this fusion process may be crucial for blocking the entry of the viral genome into the host cell if it interacts with the HR1 region in the viral S protein to form heterologous 6-HB, resulting in the inhibition of homologous 6-HB formation between HR1 and HR2 domains in the viral S protein [46].
The recently designed and engineered pan-CoV fusion inhibitor, EK1 peptide, has been reported to inhibit infection of five human coronaviruses, including SARS-CoV and MERS-CoV, and three bat- SL-CoVs [47]. Intranasal nanoformulations of the EK1 peptide can help to protect one from COVID-19 [48,49]. Further, nanostructures co-functionalized with neutralizing mAbs targeting non-RBD regions, including the NTD and S2 of SARS-CoV-2, also proved to be a powerful strategy to check viral infection [30,50].
It is certainly a good beginning to witness the development of lipid nanoparticles based on Moderna's mRNA-1273 vaccine in partnership with the National Institute for Allergy and Infectious Diseases, National Institute of Health. Moderna’s mRNA-based technology was the fastest to enter Phase I clinical trial in the US, which began on the 16th March 2020. In this study, 45 healthy individual adults between the age group of 18 to 55 years received two vaccinations, 28 days apart, with mRNA-1273 in a dose of 25 μg, 100 μg, or 250 μg. Each dose group consisted of 15 participants. It is significant to note that followed by the first vaccination, the antibody response was higher with a higher dose (day 29 enzyme-linked immunosorbent assay anti-S-2P antibody Geometric Mean Titer (GMT), 40,227 in the 25 μg group, 109,209 in the 100 μg group, and 213,526 in the 250 μg group). The titers further increased after the second vaccination (day 57 GMT, 299,751, 782,719, and 1,192,154, respectively), indicating the efficiency of the lipid nanoparticle based vaccine to mediate the induction of the anti-SARS-CoV-2 immune response [15,51].
Zhao et al. [52] reported the synthesis of poly (amino ester) with a carboxyl group (PC)-coated magnetic nanoparticles (pcMNPs) based viral RNA extraction method for the efficient detection of SARSCoV- 2. Fabrication of the pcMNPs involved two steps which started with a one-pot synthesis of NH2-MNPs using a co-precipitation reaction and hydrolysis of TEOS/APTES. Once the PC polymer was successfully synthesized, its reaction with NH2-MNPs resulted in the formation of pcMNPs with an average diameter of 10.22 nm ± 2.8 nm. Upon the incubation of 2 μg RNA molecules with 20 μg pcMNPs in a 200 μl lysis/binding buffer, more than 90% of the RNA was absorbed by the pcMNPs within 10 min. Notably, this simplified process could purify viral RNA from multiple samples within 20 min using a simple manual method or an automated high-throughput approach. Two different regions (ORFlab and N gene) of the viral RNA were identified with a 10-copy sensitivity and a strong linear correlation between 10 and 105 copies of SARS-CoV-2 pseudovirus particle was achieved [52].
The unavailability of an approved and effective vaccine has inspired the re-evaluation of potential prophylactic and/or therapeutic effects of drugs clinically approved for other diseases, especially for their efficiency against SARS-CoV-2. Chloroquine and its derivative, hydroxychloroquine, mainly used for antimalarial therapy, were found to be effective against human coronavirus OC43 and SARSCoV in in vivo and in vitro studies, respectively. Chloroquine reduced the expression of the phosphatidylinositol binding clathrin assembly protein (PICALM), which is a critical cargo-selecting clathrin adaptor that senses and drives membrane curvature, thereby regulating the rate of endocytosis. It was found that as compared to chlorpromazine (a well-known clathrin-dependent endocytosis inhibitor), chloroquine was more effective in preventing nanoparticle uptake in macrophages. Importantly, chloroquine could inhibit the endocytosis of nanoparticles in resident macrophages which may be used as a powerful strategy to ensure longer retention of nanovaccines or drug-loaded nanoparticles in the circulation and sustained release of drugs [22].
Conclusion
Whatever the nanoparticle strategy, it is clear that we need to rethink our old approaches for developing viral treatment and separating detection from treatment if we want to accelerate our answer to this and future viruses. The major challenge brought by the SARS-CoV-2 can only be solved at the nanoscale in order to hit the right target with the right sized nanodrugs. This is certainly emphasized by some of the best nanomedicine strategies advancing today, especially that developed by Moderna. Only integrative strategies with knowledge of SARS-CoV-2 structural dimension and nanotherapeutics may help to develop effective viral theranostics with prolonged efficacy to control the disease, and it’s high time to think small to fix this and future big threats.
Acknowledgments
Dr. Sougata Ghosh acknowledges the Department of Science and Technology (DST), Ministry of Science and Technology, Government of India and Jawaharlal Nehru Centre for Advanced Scientific Research, India for funding under the Post-doctoral Overseas Fellowship in Nano Science and Technology (Ref. JNC/ AO/A.0610.1(4) 2019-2260 dated August 19,2019).
Authors’ Contribution
Sougata Ghosh, Ebrahim Mostafavi, Ada Vernet-Crua, and Thomas J. Webster substantially contributed to the conception of the work and drafting. All authors approved the submitted version.
References
- Zhang C, Zhen W, Huang X, Bell EW, Zhou X, et al. (2020) Protein structure and sequence reanalysis of 2019-nCoV genome refutes snakes as its intermediate host and the unique similarity between its spike protein insertions and HIV-1. J Proteome Res 19: 1351-1360.
- https://www.worldometers.info/coronavirus/
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497-506.
- Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, et al. (2003) A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 348: 1953-1966.
- Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, et al. (2003) A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 348: 1953-1966.
- Kuiken T, Fouchier RAM, Schutten M, Rimmelzwaan, Amerongen GV, et al. (2003) Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet 362: 263-270.
- de Groot RJ, Baker SC, Baric RS, Brown CS, Drosten C, et al. (2013) Middle east respiratory syndrome coronavirus (MERS-CoV): announcement of the Coronavirus Study Group. J Virol 87: 7790-7792.
- Zaki AM, Boheemen SV, Bestebroer TM, Osterhaus ADME, Fouchier RAM (2012) Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med 367: 1814-1820.
- Drosten C, Gunther S, Preiser W, Werf SVD, Brodt HR, et al. (2003) Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med 348: 1967-1976.
- https://www.who.int/csr/sars/country/table2004_04_21/en/
- https://www.who.int/emergencies/mers-cov/en/
- Wang C, Horby PW, Hayden FG, Gao GF (2020) A novel coronavirus outbreak of global health concern. Lancet 395: 470-473.
- Menachery VD, Yount BL Jr, Debbink K, Agnihothram S, Gralinski LE, et al. (2015) A SARS-like cluster of circulating bat coronaviruses shows potential for human emergence. Nat Med 2: 1508-1513.
- Chan JFW, Yuan S, Kok KH, To KKW (2020) A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395: 514-523.
- Harypursat V, Chen YK (2020) Six weeks into the 2019 coronavirus disease (COVID-19) outbreak- it is time to consider strategies to impede the emergence of new zoonotic infections. Chin Med J (Engl) 133: 1118-1120.
- Shin MD, Shukla S, Chung YH, Beiss V, Chan SK, et al.(2020) COVID-19 vaccine development and a potential nanomaterial path forward. Nat Nanotechnol. 1-10.
- https://www.covid19treatmentguidelines.nih.gov/whats-new/
- Arvin AM, Greenberg HB (2006) New viral vaccines. Virology 344: 240-249.
- McPherson C, Chubet R, Holtz K, Honda-Okubo Y, Barnard D, et al. (2016) Development of a SARS coronavirus vaccine from recombinant spike protein plus delta inulin adjuvant. Methods Mol Biol 1403: 269-284.
- Tseng C-T, Sbrana E, Iwata-Yoshikawa N, Newman PC, Garron T, et al. (2012) Immunization with SARS coronavirus vaccines leads to pulmonary immunopathology on challenge with the SARS virus. PLoS One 7: e35421.
- Al-Halifa S, Gauthier L, Arpin D, Bourgault S, Archambault D (2019) Nanoparticle-based vaccines against respiratory viruses. Front Immunol. 10: 1-11.
- Hu TY, Frieman M, Wolfram J (2020) Insights from nanomedicine into chloroquine efficacy against COVID-19. Nat Nanotechnol 15: 247-249.
- Laval JM, Mazeran PE, Thomas D (2000) Nanobiotechnology and its role in the development of new analytical devices. Analyst 125: 29-33.
- Chattopadhyay S, Chen JY, Chen HW, Hu CJ (2017) Nanoparticle vaccines adopting virus-like features for enhanced immune potentiation. Nanotheranostics 1: 244-260.
- Schneider CS, Xu Q, Boylan NJ, Chisholm J, Tang BC, Schuster BS, et al. (2017) Nanoparticles that do not adhere to mucus provide uniform and long-lasting drug delivery to airways following inhalation. Sci Adv. 3: e1601556.
- Jung SY, Kang KW, Lee EY, Seo DW, Kim HL, et al. (2018) Heterologous prime-boost vaccination with adenoviral vector and protein nanoparticles induces both Th1 and Th2 responses against Middle East respiratory syndrome coronavirus. Vaccine 36: 3468-3476.
- Pachioni-Vasconcelos Jde A, Lopes AM, Apolinario AC, Valenzuela-Oses JK, Costa JS, et al. (2016) Nanostructures for protein drug delivery. Biomater Sci 4: 205-218.
- Fredriksen BN, Grip J (2012) PLGA/PLA micro- and nanoparticle formulations serve as antigen depots and induce elevated humoral responses after immunization of Atlantic salmon (Salmo salar L.). Vaccine 30: 656-667.
- Yong CY, Ong HK, Yeap SK, Ho KL, Tan WS (2019) Recent advances in the vaccine development against Middle East Respiratory Syndrome-Coronavirus. Front Microbiol 10: 1781.
- Liu YV, Massare MJ, Barnard DL, Kort T, Nathan M, et al. (2011) Chimeric severe acute respiratory syndrome coronavirus (SARS-CoV) S glycoprotein and influenza matrix 1 efficiently form virus-like particles (VLPs) that protect mice against challenge with SARS-CoV. Vaccine 29: 6606-6613.
- Wang C, Zheng X, Gai W, Zhao Y, Wang H, et al. (2017) MERS-CoV virus-like particles produced in insect cells induce specific humoural and cellular immunity in rhesus macaques. Oncotarget 8: 12686-12694.
- Coleman CM, Liu YV, Mu H, Taylor JK, Massare M, et al. (2014) Purified coronavirus spike protein nanoparticles induce coronavirus neutralizing antibodies in mice. Vaccine 32: 3169-3174.
- Han J, Zhao D, Li D, Wang X, Jin Z, et al. (2018) Polymer-based nanomaterials and applications for vaccines and drugs. Polymers 10: 31.
- Lee C, Jeong J, Lee T, Zhang W, Xu Li, et al.(2018) Virus-mimetic polymer nanoparticles displaying hemagglutinin as an adjuvant-free influenza vaccine. Biomaterials 183: 234-242.
- Layqah LA, Eissa S (2019) An electrochemical immunosensor for the corona virus associated with the Middle East respiratory syndrome using an array of gold nanoparticle-modified carbon electrodes. Microchim Acta 186: 224.
- Poon C, Patel AA (2020) Organic and inorganic nanoparticle vaccines for prevention of infectious diseases. Nano Express 1: 012001.
- Ahmed SF, Quadeer AA, McKay MR (2020) Preliminary identification of potential vaccine targets for the COVID-19 coronavirus (SARS-CoV-2) based on SARS-CoV immunological studies. Viruses 12: 254.
- Jung BK, Lee YK, Hong JW, Ghandehari H, Yun CO (2016) Mild hyperthermia induced by gold nanorod-mediated plasmonic photothermal therapy enhances transduction and replication of oncolytic adenoviral gene delivery. ACS Nano 10: 10533-10543.
- Chahal JS, Fang T, Woodham AW, Khan OF, Ling J, et al. (2017) An RNA nanoparticle vaccine against Zika virus elicits antibody and CD8+ T cell responses in a mouse model. Sci Rep 7: 252.
- Zhu M, Wang R, Nie G (2014) Applications of nanomaterials as vaccine adjuvants. Hum Vaccin Immunother. 10: 2761-74.
- Kumar S, Maurya VK, Prasad AK, Bhatt MLB, Saxena SK (2020) Structural, glycosylation and antigenic variation between 2019 novel coronavirus (2019-nCoV) and SARS coronavirus (SARS-CoV). Virus Dis 31: 13-21.
- Ashour HM, Elkhatib WF, Rahman MM, Elshabrawy HA (2020) Insights into the recent 2019 novel coronavirus (SARS-CoV-2) in light of past human coronavirus outbreaks. Pathogens 9: 186.
- Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, et al (2020) Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell 181: 281-292.
- Jiang S, Du L, Shi Z (2020) An emerging coronavirus causing pneumonia outbreak in Wuhan, China: calling for developing therapeutic and prophylactic strategies. Emerg Microbes Infect 9: 275-277.
- Zhou Y, Yang Y, Huang J, Jiang S, Du L (2019) Advances in MERS-CoV vaccines and therapeutics based on the receptor-binding domain. Viruses 11: 60.
- Du L, He Y, Zhou Y, Liu S, Zheng BJ, et al. (2009) The spike protein of SARS-CoV-a target for vaccine and therapeutic development. Nat Rev Microbiol 7: 226-236.
- Liu S, Xiao G, Chen Y, He Y, Niu J, et al. (2004) Interaction between heptad repeat 1 and 2 regions in spike protein of SARS associated coronavirus: implications for virus fusogenic mechanism and identification of fusion inhibitors. Lancet 363: 938-947.
- Xia S, Yan L, Xu W, Agrawal AS, Algaissi A, et al. (2019) A pan-coronavirus fusion inhibitor targeting the HR1 domain of human coronavirus spike. Sci Adv 5: eaav4580.
- Du L, Tai W, Yang Y, Zhao G, Zhu Q, et al. (2016) Introduction of neutralizing immunogenicity index to the rational design of MERS coronavirus subunit vaccines. Nat Commun 7: 13473.
- Du L, Yang Y, Zhou Y, Lu L, Li F, et al. (2017) MERS-CoV spike protein: a key target for antivirals. Expert Opin Ther Targets 21: 131-143.
- Chen Y, Lu S, Jia H, Deng Y, Zhou J, et al. (2017) A novel neutralizing monoclonal antibody targeting the N-terminal domain of the MERS-CoV spike protein. Emerg Microbes Infect 6: e37.
- Zhao Z, Cui H, Song W, Ru X, Zhou W, et al. (2020) A simple magnetic nanoparticles-based viral RNA extraction method for efficient detection of SARS-CoV-2. bioRxiv.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi