Editorial, Dent Health Curr Res Vol: 5 Issue: 1
Trends in CT Examinations and Diagnostic Reference Level (DRL)
Midori Yoshida* and Eiichi Honda
Department of Oral and Maxillofacial Radiology, Tokushima University Graduate School. 3-18-15 Kuramoto, Tokushima 770-8504, Japan
*Corresponding Author : Midori Yoshida
Department of Oral and Maxillofacial Radiology, Tokushima University Graduate School, 3-18-15 Kuramoto, Tokushima 770-8504, Japan
Tel: 81-886335461
Fax: 81-886335335
E-mail: midori2@tokushima-u.ac.jp
Received: June 15, 2018 Accepted: December 26, 2018 Published: January 07, 2019
Citation: Yoshida M, Honda E (2019) Trends in CT Examinations and Diagnostic Reference Level (DRL). Dent Health Curr Res 5:1. doi: 10.4172/2470-0886.1000e107
Abstract
Medical exposure is increasing year by year. The main reason is an increase in CT examinations. X-ray examination has been shifting from conventional radiography to CT imaging. Although CT examinations account for only 7.9% of the total number of diagnostic medical examinations, the contribution is about 47% of the total collective effective dose due to diagnostic medical radiology in health-care level I countries according to the 1997-2007 survey by UNSCEAR. Dental X-ray examinations have hardly contributed it, but CT examination is indispensable in dentistry. Dentists also should follow the requirements for CT imaging by the
ICRP recommendation and review CT imaging protocol based on national diagnostic reference level (DRL).
Keywords: CT examination; DRL; CTDI; ICRP; OECD; UNSCEAR
Background
Radiography is very important in dental treatment, and dental radiography and panoramic radiography are routinely implemented in dental practitioners. According to UNSCEAR 2008 report, the annual frequency of dental examinations has remained fairly constant for health-care level I countries (defined as those in which there was at least one physician for every 1,000 people in the general population) [1]. The number of dental examinations per 1,000 population in the 1997-2007 survey was 275, which was lower than 320 in the 1970- 1979 survey. Annual collective effective dose due to dental X-ray examinations and diagnostic medical examinations were 9,900 and 2,900,000 (man Sv), and the total radiation exposure from diagnostic radiology increased about 2.2 times from 1988 to 2008. Although CT examinations accounted for only 7.9% of the total number of diagnostic medical examinations, the contribution was about 47% of the total collective effective dose due to diagnostic medical radiology in health-care level I countries according to the 1997-2007 survey.
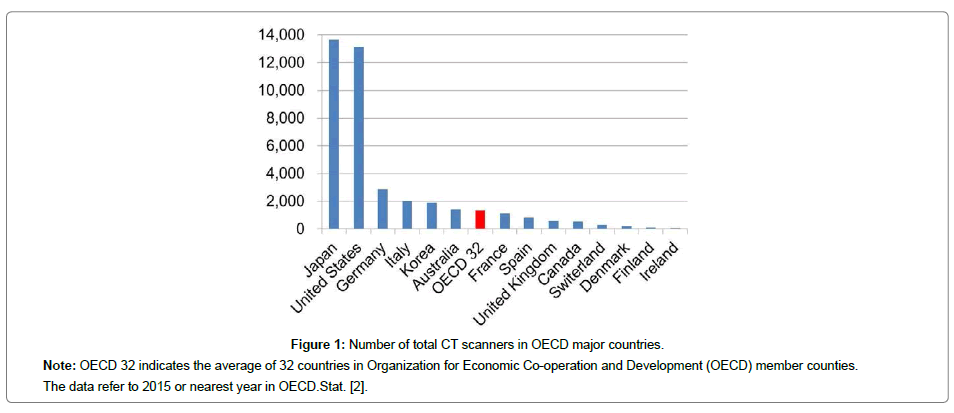
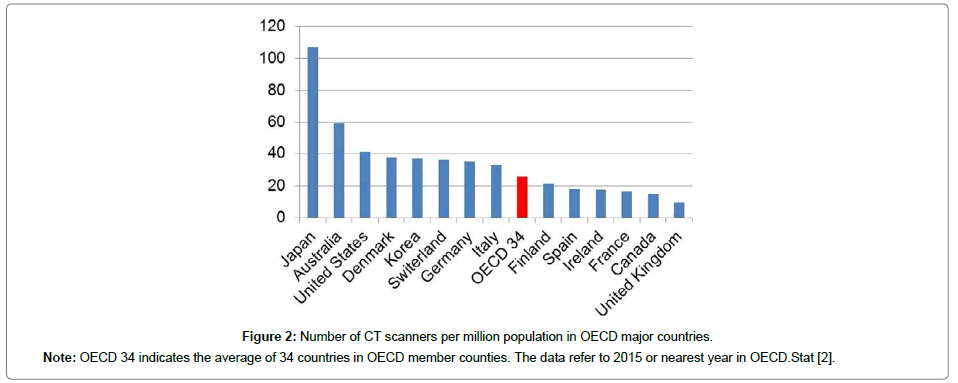
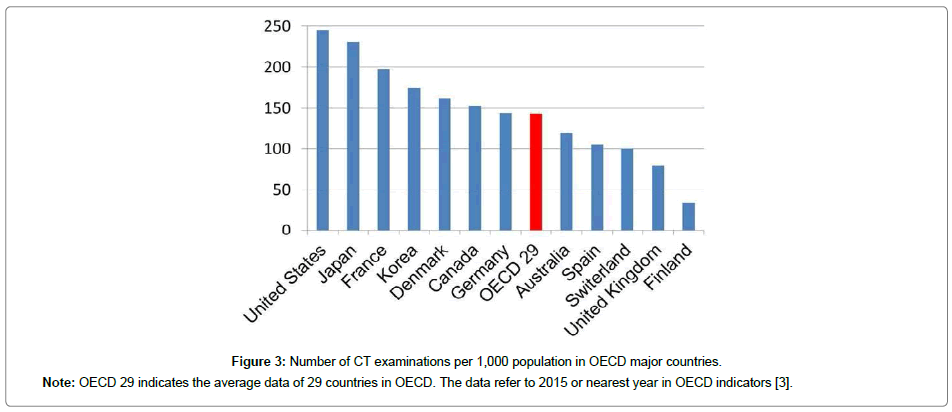
Dental radiography does not contribute to an increase of medical exposure as previously mentioned. Although CT examination is limited to hospitals and the number of the examinations is also small, CT imaging is indispensable in dentistry. The main reason for the increase in medical exposure is due to an increase of CT examinations. Current X-ray examinations have shifted from conventional radiography to CT imaging. The technology of CT scanners greatly improves diagnostic information but at the same time increases patient exposure. The availability of CT scanners has increased rapidly over the last fifteen years (Table 1) [2]. Especially, the increase rate is rising in countries with fewer CT scanners. The number of CT scanners in Japan and the United States is overwhelmingly high, and it is largely different from other countries (Figure 1) [2]. And Japan has the highest number of CT scanners per million population (Figure 2) [2]. There is not much difference in the number of CT examinations per 1,000 population in the top countries (Figure 3) [3].
Figure 1: Number of total CT scanners in OECD major countries.
Note: OECD 32 indicates the average of 32 countries in Organization for Economic Co-operation and Development (OECD) member counties.
The data refer to 2015 or nearest year in OECD.Stat. [2].
Figure 2: Number of CT scanners per million population in OECD major countries.
Note: OECD 34 indicates the average of 34 countries in OECD member counties. The data refer to 2015 or nearest year in OECD.Stat [2].
Figure 3: Number of CT examinations per 1,000 population in OECD major countries.
Note: OECD 29 indicates the average data of 29 countries in OECD. The data refer to 2015 or nearest year in OECD indicators [3].
| Year | 2000 or nearest year | 2015 or nearest year | Increase rate |
|---|---|---|---|
| Denmark | 61 | 214 | 3.5 |
| Australia | 500 | 1,418 | 2.8 |
| France | 426 | 1,103 | 2.6 |
| United Kingdom | 315 | 611 | 1.9 |
| Canada | 303 | 538 | 1.8 |
| Finland | 70 | 118 | 1.7 |
| Italy | 1,203 | 2,023 | 1.7 |
| United States | 8,230 | 13,150 | 1.6 |
| Germany | 2,023 | 2,866 | 1.4 |
| Japan | 11,803 | 13,636 | 1.2 |
Table 1: Change in the number of CT scanners for 15 years in OECD major countries.
The International Commission on Radiological Protection (ICRP) changed the limit of equivalent dose to the lens of the eye for occupational exposure in ICRP Publication 118 (2012) [4]. The value was set to 20mSv per year, averaged over defined periods of 5 years, and with no single year exceeding 50mSv. Moreover the ICRP stated to lower the threshold for cataracts to 0.5Gy, and to recommend the first ever threshold of 0.5Gy for cardiovascular disease to the heart and cerebrovascular disease to the brain. The change has a very important meaning to dentists because the regions such as the lens of the eye and the brain are constantly included in the exposure field at dental radiography, especially CT imaging of the maxillary sinus. The value has the possibility of being achieved by repeated CT examinations. Dentists also need to pay sufficient attention. The ICRP made recommendations on CT examinations in ICRP Publication 87 (2000) (Table 2) [5].
| 1. | Request for CT examination should be generated only by properly qualified medical or dental practitioners depending upon national educational and qualification system. The physician is responsible for weighing the benefits against risks. |
| 2. | Clinical guidelines advising which examinations are appropriate and acceptable should be available to clinicians and radiologists |
| 3. | Consider whether the required information be obtained by MRI, ultrasonography |
| 4. | Consider value of contrast medium enhancement prior to commencing examination |
| 5. | CT scanning in pregnancy may not be contraindicated, particularly in emergency situations, although examinations of the abdomen or pelvis should be carefully justified |
| 6. | CT examination should not be repeated without clinical justification and should be limited to the area of interest. |
| 7. | Clinician has the responsibility to communicated to the radiologist about previous CT examination of the patient. |
| 8. | CT examination for research purpose that does not have clinical justification (immediate benefit to the person undergoing the examination) should be subject to critical evaluation by an ethics committee. |
| 9. | CT examination of chest in young girls and young females needs to be justified in view of high breast dose. |
| 10. | Once the examination has been justified, radiologist has the primary responsibility for ensuring that the examination is carried out with good technique. |
Table 2: ICRP recommendation on actions for physician and radiologist in CT examination.
On the other hand, the ICRP proposed the three principles of justification, optimization, and dose limitation for radiation protection in ICRP Publication 26 (1977) (Table 3) [6]. After then the ICRP was keeping the principles and it followed a new recommendations of ICRP Publication 103 (2007) [7]. Regarding optimization of the principles, the ICRP recommended the use of dose constraints or investigation levels selected by the appropriate professional or regulatory agency in ICRP Publication 60 (1991) [8]. The dose or levels was defined as diagnostic reference level (DRL) in ICRP Publication 73 (Table 4) [9]. And the ICRP stated the principle of optimization of protection was implemented through the use of DRLs in website [10] and Publication 103 [7]. In European Union (EU), the document on DRLs for medical exposures was issued by the European Commission in 1999 [11].
| Justification Any decision that alters the radiation exposure situation should do more good than harm. |
| Optimization of protection The likelihood of incurring exposure, the number of people exposed, and the magnitude of their individual doses should all be kept as low as reasonably achievable, taking into account economic and societal factors. |
| Application of Dose Limits The total dose to any individual from regulated sources in planned exposure situations other than medical exposure of patients should not exceed the appropriate limits specified by the Commission. |
Table 3: Three fundamental principles of radiation protection.
| Commission’s term for a tool used to aid in optimisation of protection in the medical exposure of patients for diagnostic and interventional procedures. A DRL value is a selected level of a radiation dose quantity for broadly defined types of equipment for typical examinations for groups of standard-sized patients or, in certain specific circumstances, a standard phantom. |
| The purpose is advisory. It is a form of investigation level to identify unusually high levels, which calls for local review if consistently exceeded. In principle, there could be a lower level also (i.e. below which there is insufficient radiation dose to achieve a suitable medical image). Diagnostic reference levels are not for regulatory or commercial purposes, not a dose constraint, and not linked to limits or constraints. |
Table 4: Definition and purpose of diagnostic reference levels (DRLs).
Currently, A DRL is considered to be an optimum tool on radiation protection in medical imaging in international guidelines for international basic safety standards by the International Atomic Energy Agency (IAEA), the ICRP, some countries in EU, the American College of Radiology (ACR), the American Association of Physicists in Medicine (AAPM), the National Council on Radiation Protection and Measurements (NCRP), the Japan Network for Research and Information on Medical Exposure (J-RIME), and so on, established DRLs based on it (Tables 5 and 6) [12-19]. DRLs (CTDIvol [20]) of adult head CT imaging, range from 56 to 85 (mGy) (Table 5). In this way, the value is not absolute and has a certain range because a DRL depends on the patient’s standard body type, age, imaging protocol, types of equipment, and so on. Thus, dentists also should periodically review CT protocol with reference to national DRL of own country or region.
| Country or region | Year | CTDIvol (mGy) |
|---|---|---|
| Adult | ||
| European Union [12] | 2014 | 60 |
| Ireland | 2012 | 66.2 |
| United Kingdom [14] | 2016 | 60 |
| United States [15] ACR DIR ACR-AAPM NCRP |
||
| 2016 | 56 | |
| 2013 | 75 | |
| 2012 | 75 | |
| Canada [16] | 2016 | 79.1 |
| Japan [17] | 2015 | 85 |
| Australia [18] | 2018 | 52 |
Table 5: National DRL for adult head CT examinations.
| Country or region | Year | Age range CTDIvol (mGy) |
||||
|---|---|---|---|---|---|---|
| European Union [19] | 2015 | 0-9 | 10-14 | 15-29 | 30-59 | >60 |
| 25 | 25 | 38 | 53 | 60 | ||
| United Kingdom [14] | 2016 | 0-1 | 2-5 | >5 | ||
| 25 | 40 | 60 | ||||
| Canada [16] | 2016 | 0-3 | 4-7 | 8-13 | ||
| 37 | 51.5 | 52.9 | ||||
| Japan [17] | 2015 | 0 | 1-5 | 6-10 | ||
| 38 | 47 | 60 | ||||
| Australian [18] | 2018 | 0-4 | 5-14 | |||
| 30 | 35 | |||||
Table 6: National DRL for paediatric head CT examinations.
References
- United Nations scientific committee on the effects of atomic radiation (2010) Sources and effects of ionizing radiation, UNSCER 2008 report to the general assembly with scientific annexes 1 New York, United Nations.
- OECD (2018) Medical technology, Health care resources. OECD Stat.
- OECD (2017), Health at a glance 2017: OECD indicators, OECD publishing, France.
- ICRP (2012) ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs - threshold doses for tissue reactions in a radiation protection context. Ann ICRP 41: 1-322.
- ICRP (2000) Managing patient dose in computed tomography. A report of the International Commission on Radiological Protection. Ann ICRP 30: 7-45.
- ICRP (1977) Recommendations of the ICRP. Ann ICRP 1: 1-242.
- ICRP (2007) The 2007 recommendations of ICRP. Ann ICRP 37: 1-332.
- ICRP (1991) 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP 21: 1-201.
- ICRP (1996) Radiological protection and safety in medicine. Eur J Nucl Med 24: 1207-1209.
- ICRP (2001) Diagnostic reference levels in medical imaging: review and additional advice. Ann ICRP 31: 33-52.
- European Commission (1999) Guidance on diagnostic reference levels (DRLs) for medical exposures. Radiation protection 109.
- European Union (2014) Diagnostic reference levels in thirty-six European Countries. Radiation Protection No 180.
- Foley SJ, McEntee MF, Rainford LA (2012) Establishment of CT diagnostic reference levels in Ireland. Br J Radiol 85: 1390-1397.
- Public Health England (2016) Guidance: National diagnostic reference levels (NDRLs).
- Kanal KM, Butler PF, Sengupta D, Bhargavan-Chatfield M, Coombs LP, et al. (2017) U.S. diagnostic reference levels and achievable doses for 10 adult CT examinations. Radiology 284: 120-133.
- Government of Canada (2016) Canadian computed tomography survey - national diagnostic reference levels.
- The Japan Medical Imaging and Radiological Systems Industries (2015) Diagnostic reference levels based on latest surveys in Japan -Japan DRLs 2015.
- Australian Radiation Protection and Nuclear Safety Agency, Australian Government (2018) Current Australian national diagnostic reference levels for multi detector computed tomography.
- European diagnostic reference level for Pediatric Imaging (2015) European guidelines on DRLs for paediatric imaging.
- Nagel HD (2018) CT Parameters that influence the radiation Dose. Science & Technology for Radiology.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi